BRICS health and tuberculosis control collaborations during an era of global health
—
Abstract
Introduction
In 2001, Jim O’Neill, a British economist at Goldman Sachs, grouped Brazil, Russia, India, and China together, given their growing proportion of the global gross domestic product (GDP), which in turn raised ‘important issues about the global economic impact of fiscal and monetary policy in the BRICs’ (O’Neill 2001, S01). Nearly ten years on, in 2009, the acronym ‘BRIC’ evolved into ‘BRICS’ when the four countries were joined by South Africa. In 2011, BRICS convened the first formal meeting of health ministers; the resulting Beijing Declaration committed to ‘support and undertake inclusive global public health cooperation projects, including through South–South and triangular cooperation’ (BRICS Health Ministers 2011). While acknowledging their diversity, they highlighted shared ‘public health challenges, including inequitable access to health services and medicines, growing health costs, infectious diseases such as HIV and tuberculosis (TB), while also facing growing rates of non-communicable diseases’ (BRICS Health Ministers 2011). In short order, BRICS moved beyond their original economic grouping to work on health, despite not sharing a common geographical region, official language, or political history.
Scholarly interest in BRICS has grown in recent years, and health in particular has received much attention. In a systematic literature review, Andrew Harmer and colleagues (2013, 1) noted an ‘overwhelming tendency to describe individual BRICS countries [sic] influence’ (see also Ezziane 2014). Much of the literature has concentrated on country-specific analyses (Lancet 2009, 2011a, 2011b, 2012, 2013), investigations of shared health challenges (Creswell et al. 2014; Cashwell et al. 2014; Ernest et al. 2014; Marten et al. 2014; Rao et al. 2014), or opportunities for technological developments (Ezziane 2014; Kaddar, Milstien, and Schmitt 2014). Several researchers have examined BRICS health initiatives vis-à-vis global health (Fleck and Harmer 2014; Watt, Gomez, and McKee 2014; Buss, Ferreira, and Hoirisch 2014), in large part asking: ‘to what extent does it make sense to talk of “the BRICS” as a coherent unit of analysis?’ (Harmer and Buse 2014, 130).
Using TB control collaborations as a grounding example, in this think piece I attempt to grasp the specificity of BRICS health collaborations in an era of global health, asking: What are the broader characteristics of BRICS health collaborations, which seek to confront both infectious diseases, such as TB, HIV, and malaria, and noncommunicable diseases, including harmful alcohol use, obesity, and road safety? What is prioritized under such health collaborations? Can BRICS countries’ collaborations on health be understood as a new form that escapes the existing conceptual frames of both global and international health?
In doing so, I am less concerned with the tangible evidence of BRICS collaborations, or how such collaborations fit into theoretical models or frameworks (for examples, see Harmer and Buse 2014; Watt, Gomez, and McKee 2014). Rather, I adopt a genealogical approach in order to understand how collaborations are being framed, particularly in contrast to international and global health programs. After providing a historical overview of the context in which BRICS health collaborations developed, I describe TB control initiatives in order to highlight what BRICS collaborations deem to be possible. Finally, I discuss novel aspects of BRICS collaborations, contrasting them to other health collaborations. I argue that BRICS health collaborations hold the nation-state as the primary referent, aspire towards the global, and remain flexible in the ways in which they operate, gesturing towards a neoliberal ethic.
A note on terminology: As Harmer and colleagues (2013) have pointed out, the acronym ‘BRICS’ is used with both indefinite and definite articles. Further, ‘BRICS’ is used in the singular and plural. In taking BRICS as a unit, I use the term as a singular noun. I also use ‘BRICS’ as an adjective, such as in ‘BRICS health collaborations’. Finally, I use ‘BRICs’ to indicate the pre-2010 grouping without South Africa, and ‘BRICS’ to refer to the unit after South Africa’s inclusion.
Historical forms: Developing BRICS health collaborations during the transition from international to global health
International efforts to confront health challenges date to the mid-eighteenth century, initiated through work aimed at preventing the importation of diseases such as cholera (Hardy 1993; Valeska 2006). Colonialism and religious medical missions further served to establish a network of laboratories, treatment centers, and physicians around the world (Cohen 1983; Arnold 1993; Monnais 2006; Heinrich 2008). The World Health Organization (WHO), like its precursor, the League of Nations’ Health Organization (LNHO) (Dubin 1995), stemmed from such efforts, founded on a nation-state paradigm. Dr. Brock Chisholm (1950, 4661), the WHO’s first Director-General, outlined the fledgling organization’s mandate: for all people to gain ‘the highest possible level of health’ through ‘completely united action’ between ‘the nations of the world’.
By the late 1970s, however, international health collaborations had become severely stymied. The broad, valiant goals of Alma Ata to provide ‘health for all’ under the rubric of primary health care (WHO 1978; UN Sixty-Fourth General Assembly 1981) were replaced with targeted or ‘selective’ interventions during the 1980s (Cueto 2004), in the context of structural adjustment programs at the country level, decreased international aid, and a general global economic downturn (Brown, Cueto, and Fee 2006; Keshavjee 2014). As a result, the 1980s became known as the ‘lost decade’ of development (Escobar 1995; Stiglitz 2002; Hulme 2010).
The space left by structurally adjusted national institutions and international health and development agencies, such as the WHO and the UN Development Programme (UNDP), allowed actors at various levels to grow in prominence, including the World Bank, the Organization for Economic Co-operation and Development (OECD), and civil society groups. Researchers have pointed to this moment as marking the transition from international to global health. As Theodore Brown, Marcos Cueto, and Elizabeth Fee (2006, 62) have noted, ‘“global health” in general implies consideration of the health needs of the people of the whole planet above the concerns of particular nations’, and further emphasizes ‘the growing importance of actors beyond government or intergovernmental organizations and agencies’. Andrew Lakoff (2010) has further distinguished between two contemporary regimes of global health: ‘global health security’, which focuses on emerging infectious diseases and preparedness systems on a global scale rather than simply across national borders (as evidenced by the 2003 SARS pandemic), and ‘humanitarian biomedicine’, which targets diseases afflicting the world’s poor through advanced, cost-effective diagnostic and treatment technologies.
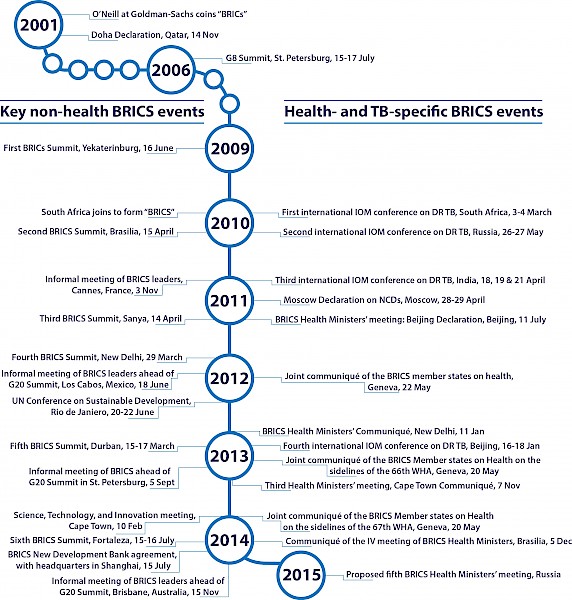
BRICs= Brazil, Russia, India, and China; BRICS= Brazil, Russia, India, China, and South Africa; DR TB = drug-resistant TB; G8/G20 = Group of 8, Group of 20; IOM = US Institute of Medicine; NCDs = noncommunicable diseases; WHA = World Health Assembly.
BRICS health collaborations have developed contemporaneously with the broader transition from international to global health (figure 1). Prior to the first summit of the BRIC heads of state, held in Russia in 2009, several country-level high-profile events emphasized health. For example, in 2006, Russia made infectious disease control a centerpiece of the G8 Summit, held in St. Petersburg. With the addition of South Africa in 2010, a meeting of the BRICS leaders held in Sanya (China) on 14 April 2011 preceded the first official meeting of the health ministers, which was hosted in Beijing a few months later on 11 July. Soon after, BRICS was envisioned as a ‘forum of coordination, cooperation, and consultation on relevant matters related to global public health’ (BRICS Health Ministers 2011). Since then, the BRICS health ministers have held four official meetings; additional informal meetings and conferences have further facilitated dialogue and collaborations, such as sideline meetings at the Sixty-fifth, Sixty-sixth, and Sixty-seventh World Health Assemblies (BRICS Health Ministers 2012, 2013b, 2014b). In addition, in July 2014, BRICS signed an agreement to create the ‘New Development Bank’, headquartered in Shanghai, with a goal of mobilizing ‘resources for infrastructure and sustainable development projects in BRICS and other emerging economies and developing countries’ (BRICS Heads of State 2014). The new bank had an initial subscribed capital and authorized capital of US$50 billion and US$100 billion respectively.
BRICS health collaboration priorities: The case of tuberculosis control
What are BRICS health collaborations? What elements do they prioritize? In order to focus my discussion, I examine a health challenge emphasized in the statements resulting from all four official health ministers’ meetings: TB.
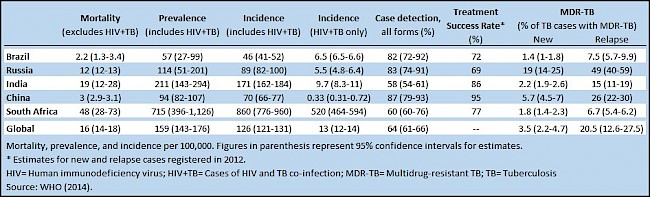
In large part, TB matters to BRICS as aggregated figures constitute a large proportion of the total global burden. Combined, BRICS accounts for 46 percent of global incident cases of TB, and 40 percent of global mortality (Creswell et al. 2014). All five countries are part of the WHO-designated ‘high-burden countries’ for multidrug-resistant (MDR) and extensively drug-resistant (XDR) TB (WHO 2014). Given these figures, controlling TB in BRICS impacts progress towards global targets, such as the 2015 UN Millennium Development Goals (MDGs). Beyond challenges indicated by epidemiological data (table 1), other similarities threaten TB-control efforts. The private health sector, for example, not only constitutes a substantial proportion of overall health spending (Rao et al. 2014), but also offers venues where first- and second-line TB drugs are available due to lack of governmental regulation (Wells et al. 2011), aiding the creation of drug-resistant forms (Gandhi et al. 2010).
Despite similarities, country-level TB indicators demonstrate epidemiological differences. For example, China has drastically lowered prevalence, incidence, and mortality rates from 1990 levels (Wang et al. 2014; WHO 2014). In contrast, prevalence and incidence in India, though uncertain, remain high (Bhatter, Chatterjee, and Mistry 2012), and the TB epidemic in South Africa is severely impacted by co-infection with HIV (Karim et al. 2009; WHO 2014).
The 2013 New Delhi Health Ministers’ Communiqué brought high-level political commitment for BRICS collaboration on TB control. The ministers ‘resolved to collaborate and cooperate’ to ‘reduce the prevalence and incidence of TB through innovation’, including new drugs, vaccines, and diagnostics, and strengthened access to affordable medicines (BRICS Health Ministers 2013a). In addition to official meetings of health ministers, TB experts from BRICS and beyond have met to ‘share the knowledge and best practices through information exchange’, a goal made explicit by the health ministers (BRICS Health Ministers 2013c). For example, the US Institute of Medicine (IOM) supported a series of drug-resistant TB workshops. Four out of six were held internationally, in South Africa (IOM 2011a), Russia (IOM 2011b), and India (IOM 2012); the final workshop, held in Beijing, highlighted MDR-TB as a challenge for all BRICS countries (IOM 2014).
The most recent meeting of the health ministers, hosted in Brasilia on 5 December 2014, put forward a more concrete agenda for collaboration on TB control (BRICS Health Ministers 2014a). Consisting of five distinct points, the list reveals broader collaborative priorities, and is thus worth quoting in full:
- universal access to first line anti-tuberculosis medicines in BRICS countries, as well as in low- and middle-income countries;
- scientific research and innovations on diagnostics [and] treatment including drug resistance and service delivery of TB;
- sharing technologies [and] identifying manufacturing capacities and means of financing;
- to aspire towards a 90-90-90 TB target (90 percent of vulnerable groups screened, 90 percent diagnosed and started on treatment with 90 percent treatment success);
- and other issues of common interest.
This ‘cooperation plan’ for TB control makes clear overarching collaboration priorities. Tuberculosis is positioned as a challenge to health in BRICS, the control of which has been determined to not only be the most cost-effective public health intervention (Lancet 2014), but also to positively impact national GDP (World Bank 1993; Jamison et al. 2013). The solution to this challenge relies on established approaches: affordable medicines and quality care (Rao et al. 2014), delivered through state-sponsored primary health care, with clear quantitative benchmarks for success. However, BRICS emphasis on innovation represents a departure from business as usual, from technological advances (new vaccines, diagnostics, and drugs) to service delivery (e-Health and tele-medicine). Pragmatically, such health initiatives are seemingly inward facing, principally serving national health priorities and populations. Moves to acknowledge problems BRICS shares with ‘low- and middle-incomecountries’ set the stage for an enlarged scope, and the New Development Bank is well positioned to serve as a financial mechanism from which to do so.
This overview of TB-control collaborations might suggest that BRICS health collaborations are narrowly concerned with infectious and neglected diseases. On the contrary, the health ministers have noted a wide range of other health challenges, including climate change; harmful alcohol use; HIV/AIDS; malaria; maternal and child mortality; mental health; overweight, obesity, and malnutrition-related diseases; road safety; and tobacco control. The notable dual focus on communicable and noncommunicable diseases (NCDs) recognizes that ‘NCDs are now a global priority that affects low, middle and high income countries’ (BRICS Health Ministers 2013a). As noted by Andrew Harmer and Kent Buse (2014, 141), ‘that the BRICS stress the need to tackle the social and economic determinants of NCDs … suggests a rather progressive, forward-looking approach to a neglected global health agenda’.
Understanding BRICS health collaborations
Much of the literature on BRICS health initiatives has produced analyses that highlight specific health challenges and collaborative opportunities. Yet, in this literature, researchers have largely concentrated on either individual country-level analyses, or they have fit BRICS health collaborations into existing theoretical frameworks. How should BRICS health collaborations be understood given their initial economic framework, in contrast with other health efforts that were structured by other factors, such as geographic proximity (Fee and Brown 2002), political alignment (Bernstein, Burton, and Healey 2010), historical entanglement (Guénel 1999; Monnais 2006), medical missionary work (Andrews 1997; Heinrich 2008), philanthropy (Bullock 1980), climatic similarities (Arnold 1996), biosecurity (Lakoff and Collier 2008), or humanitarianism (Redfield 2013)?
In answering this question, it is instructive to begin by contrasting BRICS collaborations with prevailing paradigms, that is, international and global health. BRICS health collaborations are international in that they too rely on the nation-state as the primary operational unit and referent. National health priorities are reflected in the language used in the health ministers’ declarations and communiqués, which utilize the following terms and phrases: ‘population’, ‘primary health care’, ‘universal health care’, ‘health surveillance systems’, and ‘health system strengthening’. Yet, as opposed to international health, in the existing sense of the term, BRICS has not come together to prevent the spread of disease across national borders. Indeed, with the exception of the borders China shares with India and Russia respectively, BRICS countries are not contiguous. Moreover, whereas international health has concentrated on the control and spread of infectious diseases, BRICS health collaborations highlight both communicable and noncommunicable diseases.
BRICS health collaborations also do not conform to the conceptual framing of global health, as laid out by Lakoff, Kickbusch, and others. While questions of biosecurity form a part of the discussions, particularly through the need for greater surveillance, they are not the primary focus. Neither do health collaborations follow a humanitarian ethic that is global in scope. Rather, health egalitarianism, such as expanding universal health coverage and ensuring access to affordable medicines, is primarily delimited by the nation-state. This points to a revitalization of the nation-state as the primary provider of health services, even if such solutions are arrived at through partnerships between the private and public sectors.
If BRICS health collaborations are based on precepts that do not align with either international or global health, in the existing sense of the terms, then what are they? Several salient features emerge from health ministers’ declarations and communiqués, and secondary literature. First, BRICS collaborations can be partial, temporally limited, multifaceted, and flexible. While at times BRICS works as a coherent unit with a singular voice, each of the BRICS countries individually engages in bi-, tri-, and multilateral or plurilateral efforts to improve health (Harmer et al. 2013; Buss, Ferreira, and Hoirisch 2014). The temporal instability of these collaborations and the lack of uniformity of positions provides an ambiguity that can, and has, been read as evidence that these are not true ‘collaborations’. Rather, such collaborations should be thought of as convenient and flexible, at times serving the interests of individual BRICS countries, a grouping of BRICS countries, or BRICS as a whole.
Second, these flexible BRICS collaborations are both an aid and a threat to the established (health) order. Part of the anxiety around BRICS, economically or otherwise, is ‘the prospect of a unified geopolitical bloc, consciously seeking to reframe international and global health development with a new set of ideas and values’ (Ezziane 2014, 365). On the one hand, BRICS leverages its financial and technological capacities to reorganize the global order from the outside, particularly in establishing more South–South alliances. For example, overall foreign assistance from BRICS countries has been estimated at US$5.6 billion (Cashwell et al. 2014), though the lack of centralized reporting and recording mire estimates for health aid (Fan et al. 2014). Disrupting traditional aid relations is further reflected in the rhetoric used by BRICS, whereby ‘aid’ is replaced with ‘development assistance’ or ‘cooperation’, and the binary between ‘donors’ and ‘recipients of aid’ is replaced with ‘partnerships’ (Fleck and Harmer 2014; Harmer and Buse 2014).
Simultaneously, BRICS has worked to change existing institutions and structures from within, and BRICS health ministers emphasize their support for organizations, such as the WHO and World Bank, throughout their declarations and communiqués. For example, in the Beijing Declaration, the ministers stated: ‘We are determined to strengthen public health at the global level and to improve the leading and coordinating role of the World Health Organization (WHO) in international health cooperation’ (BRICS Health Ministers 2011). Lara Gautier and colleagues (2014) have examined the role of BRICS in the WHO reforms undertaken since 2009, concluding that the influence of BRICS would likely increase in the future. As such, BRICS collaborations are not a straightforward case of counterhegemony.
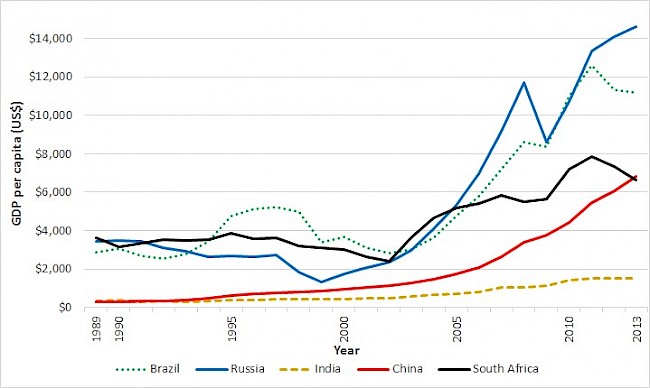 Figure 2. Gross domestic product (GDP) per capita for BRICS countries, 1989 to 2013. Source: World Bank (2015).
Figure 2. Gross domestic product (GDP) per capita for BRICS countries, 1989 to 2013. Source: World Bank (2015).Lastly, as with their original grouping, what seems to be the underlying characteristic of BRICS collaborations is economics. After all, despite inequalities, neoliberal economic reforms in BRICS are cited as having lifted hundreds of millions out of poverty, resulting in marked improvements in health (Acharya et al. 2014). In 1990, BRICS countries had a GDP per capita below US$4,000, which increased to over US$6,000 by 2013 in each country except India (figure 2). In 2001, BRICS accounted for US$2.8 trillion, or 8.5 percent, of the global GDP, estimated at US$33.1 trillion; in 2013, this proportion more than doubled to 20.9 percent of the estimated US$75.6 trillion global GDP (World Bank 2015).
BRICS recognizes ill health as an impediment to economic development, following the economic conceptualization put forward by the World Bank (1993), and others. The health ministers write that they ‘fully [recognize] that there cannot be development without health’ (BRICS Health Ministers 2013b), that ‘public health is an essential element for social and economic development’, and that they are ‘committed to act on economic, social and environmental determinants of health’ (BRICS Health Ministers 2011).
During an era of global health, despite their significant differences, BRICS has come together to collaborate on health. The nature of such collaborations remains based on the nation-state, but gestures towards larger global aspirations. Collaborations are inherently flexible and mutable, depending on context and national priorities, suggesting the importance of a neoliberal ethic.
Conclusion: Rethinking health collaborations
I originally became interested in BRICS health collaborations in 2011 as an intern at the WHO China Country Representative Office in Beijing, as China hosted both the heads of state and health ministers gatherings that year. While I was not able to attend the ministers’ inaugural meeting, and indeed did not know anyone who did, the event sparked a curiosity about the possibilities of this new form, a curiosity that has been reignited by conferences, conversations with health experts, scholarly articles, tweets, blogs, and news reports.
In this think piece, I outlined the novel forms of BRICS health collaborations, particularly in contrast to previous efforts. By using TB control as a grounding example, I have shown that BRICS collaborations have five main characteristics: state-led solutions, particularly through egalitarian policies aimed at expanding universal health coverage; scientific and programmatic innovation; experience and technology sharing; clear benchmarks for progress, based on current best practices for control; and flexibility.
Unlike international health, BRICS health collaborations are not primarily concerned with preventing the importation of infectious disease across national borders. Nor are they based on global health’s concerns regarding biosecurity or a humanitarian biomedicine. Rather, BRICS collaborative health efforts are founded on the nation-state. They aspire towards the global, and remain flexible in the ways in which they operate. Such flexibility allows BRICS countries to work within existing health and development structures, while concomitantly establishing their own institutions from which to change traditional assistance relationships. Finally, BRICS envision health collaborations as a component of economic development, whereby solving health problems improves national economies.
This is just a first step towards understanding the difference that BRICS collaborations introduce in an era of global health. Sustained anthropological fieldwork could contribute a great deal by carefully documenting and analyzing the process and conceptual framing as this flexible form evolves.
About the author
Emilio Dirlikov recently successfully defended his doctoral dissertation and will soon graduate from McGill University’s Department of Anthropology and Social Studies of Medicine. His dissertation is entitled ‘Controlling tuberculosis then and now: Chinese public health policymaking and problematizations in an era of Global Health’, and is based on two years of multisited field research on TB control in China. He sincerely thanks Andrew McDowell, Mark Daku, and Sarah Hazell, as well as Erin Martineau and Eileen Moyer, for their edits and comments on previous drafts of this think piece.
References
Acharya, Shambhu, Sarah-Louise Barber, Daniel Lopez-Acuna, Natela Menabde, Luigi Migliorini, Joaquín Molina, Bernhard Schwartländer, and Pascal Zurn. 2014. ‘BRICS and Global Health’. Bulletin of the World Health Organization 92, no. 6: 386–86A. http://dx.doi.org/10.2471/BLT.14.140889.
Andrews, Bridie J. 1997. ‘Tuberculosis and the Assimilation of Germ Theory in China, 1895-1937’. Journal of the History of Medicine and Allied Sciences 52, no. 1: 114–57. PMID: 9071849.
Arnold, David. 1993. Colonizing the Body: State Medicine and Epidemic Disease in Nineteenth-century India. Berkeley: University of California Press.
Arnold, David. 1996. Warm Climates and Western Medicine: The Emergence of Tropical Medicine, 1500–1900. Amsterdam: Rodopi.
Bernstein, Frances Lee, Chris Burton, and Dan Healey. 2010. Soviet Medicine: Culture, Practice, and Science. DeKalb: Northern Illinois University Press.
Bhatter, P., A. Chatterjee, and N. Mistry. 2012. ‘The Dragon and the Tiger: Realties in the Control of Tuberculosis’. Interdisciplinary Perspectives on Infectious Diseases 2012: 1-10. PMID: 22829815.
BRICS Heads of State. 2014. ‘BRICS New Development Bank: Agreement on the New Development Bank’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/140715-bank.html.
BRICS Health Ministers. 2011. ‘BRICS Health Ministers’ Meeting: Beijing Declaration’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/110711-health.html.
BRICS Health Ministers. 2012. ‘Joint Communiqué of the BRICS Member States on Health’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/120522-health.html.
BRICS Health Ministers. 2013a. ‘BRICS Health Ministers’ Communiqué’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/130111-health.html.
BRICS Health Ministers. 2013b. ‘Joint Communiqué of the BRICS Member States on Health on the Sidelines of the 66th WHA’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/130520-health.html.
BRICS Health Ministers. 2013c. ‘Third Health Ministers’ Meeting: Cape Town Communiqué’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/131107-health.html.
BRICS Health Ministers. 2014a. ‘Communiqué of the IV Meeting of BRICS Health Ministers’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/141205-health.html.
BRICS Health Ministers. 2014b. ‘Joint Communiqué of the BRICS Member States on Health on the Sidelines of the 67th WHA’. Accessed 4 February 2015. http://www.brics.utoronto.ca/docs/140520-health.html.
Brown, Theodore M., Marcos Cueto, and Elizabeth Fee. 2006. ‘The World Health Organization and the Transition from “International” to “Global” Public Health’. American Journal of Public Health 96, no. 1: 62–72. http://dx.doi.org/AJPH.2004.050831.
Bullock, Mary Brown. 1980. An American Transplant: The Rockefeller Foundation and Peking Union Medical College. Berkeley: University of California Press.
Buss, Paulo Marchiori, José Roberto Ferreira, and Claudia Hoirisch. 2014. ‘Health and Development in BRICS Countries’. Saúde e Desenvolvimento nos Países BRICS 23, no. 2: 390–403. http://dx.doi.org/10.1590/S0104-12902014000200004.
Cashwell, Amber, Anupama Tantri, Ashley Schmidt, Greg Simon, and Neeraj Mistry. 2014. ‘BRICS in the Response to Neglected Tropical Diseases’. Bulletin of the World Health Organization 92, no. 6: 461–62. http://dx.doi.org/10.2471/BLT.13.132555.
Chisholm, Brock. 1950. ‘The World Health Organization’. The British Medical Journal 1, no. 4661: 1021-1027. PMCID: PMC2037605.
Cohen, William B. 1983. ‘Malaria and French Imperialism’. The Journal of African History 24, no. 01: 23–36.
Creswell, Jacob, Suvanand Sahu, Kuldeep Singh Sachdeva, Lucica Ditiu, Draurio Barreira, Andrei Mariandyshev, Chen Mingting, and Yogan Pillay. 2014. ‘Tuberculosis in BRICS: Challenges and Opportunities for Leadership within the Post-2015 Agenda’. Bulletin of the World Health Organization 92, no. 6: 459–60. http://dx.doi.org/10.2471/BLT.13.133116.
Cueto, Marcos. 2004. ‘The Origins of Primary Health Care and Selective Primary Health Care’. American Journal of Public Health 94, no. 11: 1864–74. PMCID: PMC1448553.
Dubin, Martin David. 1995. ‘The League of Nations Health Organization’. In International Health Organisations and Movements, 1918-1939, edited by Paul Weindling, 56–80. Cambridge, UK: Cambridge University Press.
Ernest, T., J. Xu, S. Gao, J. H. Chen, W. Hei, R. Perelet, L. M. Birtkoltz, and Z. Xiaonong. 2014. ‘Tackling Inequitable Public Health Burden of Emerging and Neglected Diseases in BRICS Countries’. International Journal of Infectious Diseases 21, no. S1: 234–35. http://dx.doi.org/10.1016/j.ijid.2014.03.909.
Escobar, Arturo. 1995. Encountering Development: The Making and Unmaking of the Third World. Princeton, NJ: Princeton University Press.
Ezziane, Zoheir. 2014. ‘Essential Drugs Production in Brazil, Russia, India, China and South Africa (BRICS): Opportunities and Challenges’. International Journal of Health Policy and Management 3, no. 7: 365–70. http://dx.doi.org/10.15171/ijhpm.2014.118.
Fan, Victoria Y., Karen A. Grépin, Gordon C. Shen, and Lucy Chen. 2014. ‘Tracking the Flow of Health Aid from BRICS Countries’. Bulletin of the World Health Organization 92, 6: 457–58. http://dx.doi.org/10.2471/BLT.13.132472.
Fee, Elizabeth, and Theodore M. Brown. 2002. ‘100 Years of the Pan American Health Organization’. American Journal of Public Health 92, no. 12: 1888–89.
Fleck, Fiona, and Andrew Harmer. 2014. ‘The BRICS Countries: A new force in global health?’ Bulletin of the World Health Organization 92, no. 6: 394–95. http://dx.doi.org/10.2471/BLT.14.030614.
Gandhi, Neel R., Paul Nunn, Keertan Dheda, H. Simon Schaaf, Matteo Zignol, Dick van Soolingen, Paul Jensen, and Jaime Bayona. 2010. ‘Multidrug-resistant and Extensively Drug-resistant Tuberculosis: A Threat to Global Control of Tuberculosis’. The Lancet 375, no. 9728: 1830–43. http://dx.doi.org/10.1016/S0140-6736(10)60410-2.
Gautier, Lara, Andrew Harmer, Fabrizio Tediosi, and Eduardo Missoni. 2014. ‘Reforming the World Health Organization: What influence do the BRICS Wield?’ Contemporary Politics 20, no. 2: 163–81. http://dx.doi.org/10.1080/13569775.2014.907987.
Guénel, Annick. 1999. ‘The Creation of the First Overseas Pasteur Institute, or the Beginning of Albert Calmette’s Pastorian Career’. Medical History 43, no. 1: 1–25. PMCID: PMC1044108.
Hardy, Anne. 1993. ‘Cholera, Quarantine and the English Preventive System, 1850-1895’. Medical History 37 no. 3: 250–69. PMCID: PMC1036746.
Harmer, Andrew, and Kent Buse. 2014. ‘The BRICS: A Paradigm Shift in Global Health?’ Contemporary Politics 20, no. 2: 127–45. http://dx.doi.org/10.1080/13569775.2014.907988.
Harmer, Andrew, Yina Xiao, Eduardo Missoni, and Fabrizio Tediosi. 2013. ‘“BRICS without Straw”? A Systematic Literature Review of Newly Emerging Economies’ Influence in Global Health’. Globalization and Health no. 9: 15. http://dx.doi.org/10.1186/1744-8603-9-15.
Heinrich, Larissa. 2008. The Afterlife of Images: Translating the Pathological Body Between China and the West, Body, Commodity, Text. Durham, NC: Duke University Press.
Hulme, David. 2010. ‘Lessons from the Making of the MDGs: Human Development Meets Results-based Management in an Unfair World’. IDS Bulletin 41, no. 1: 15–25. http://dx.doi.org/10.1111/j.1759-5436.2010.00099.x.
IOM (Institute of Medicine). 2011a. The Emerging Threat of Drug-resistant Tuberculosis in Southern Africa: Global and Local Challenges and Solutions: Summary of a Joint Workshop. Washington, DC: The National Academies Press.
IOM. 2011b. The New Profile of Drug-resistant Tuberculosis in Russia: A Global and Local Perspective: Summary of a Joint Workshop. Washington, DC: The National Academies Press.
IOM. 2012. Facing the Reality of Drug-resistant Tuberculosis in India: Challenges and Potential Solutions: Summary of a Joint Workshop. Washington, DC: The National Academies Press.
IOM. 2014. The Global Crisis of Drug-resistant Tuberculosis and Leadership of China and the BRICS: Challenges and Opportunities: Summary of a Joint Workshop. Washington, DC: The National Academies Press.
Jamison, Dean T., Lawrence H. Summers, George Alleyne, Kenneth J. Arrow, Seth Berkley, Agnes Binagwaho, Flavia Bustreo, David Evans, Richard G. A. Feachem, Julio Frenk, Gargee Ghosh, Sue J. Goldie, Yan Guo, Sanjeev Gupta, Richard Horton, Margaret E. Kruk, Adel Mahmoud, Linah K. Mohohlo, Mthuli Ncube, Ariel Pablos-Mendez, Reddy K. Srinath, Helen Saxenian, Agnes Soucat, Karene H. Ulltveit-Moe, and Gavin Yamey. 2013. ‘Global Health 2035: A World Converging within a Generation’. Lancet 382, no. 9908: 1898–1955. http://dx.doi.org/10.1016/S0140-6736(13)62105-4.
Kaddar, Miloud, Julie Milstien, and Sarah Schmitt. 2014. ‘Impact of BRICS’ Investment in Vaccine Development on the Global Vaccine Market’. Bulletin of the World Health Organization 92, no. 6: 436–46. http://dx.doi.org/10.2471/BLT.13.133298.
Karim, Salim S. Abdool, Gavin J. Churchyard, Quarraisha Abdool Karim, and Stephen D. Lawn. 2009. ‘HIV Infection and Tuberculosis in South Africa: An Urgent Need to Escalate the Public Health Response’. Lancet 374, no. 9693: 921–33. http://dx.doi.org/10.1016/S0140-6736(09)60916-8.
Keshavjee, Salmaan. 2014. Blind Spot: How Neoliberalism Infiltrated Global Health. Oakland: University of California Press.
Lakoff, Andrew. 2010. ‘Two Regimes of Global Health’. Humanity: An International Journal of Human Rights, Humanitarianism, and Development 1, no. 1: 59–79. http://dx.doi.org/10.1353/hum.2010.0001.
Lakoff, Andrew, and Stephen J. Collier. 2008. Biosecurity Interventions: Global Health & Security in Question. New York: Columbia University Press.
Lancet. 2009. ‘Health in South Africa’. Lancet, Global Health Series. Accessed 4 February 2015. http://www.thelancet.com/series/health-in-south-africa.
Lancet. 2011a. ‘Health in Brazil’. Lancet, Global Health Series. Accessed 4 February 2015. http://www.thelancet.com/series/health-in-brazil.
Lancet. 2011b. ‘India: Towards Universal Health Coverage’. Lancet, Global Health Series. Accessed 4 February 2015. http://www.thelancet.com/series/india-towards-universal-health-coverage.
Lancet. 2012. ‘China’. Lancet 379, no 9818. Accessed 4 February 2015. http://www.thelancet.com/journals/lancet/issue/vol379no9818/PIIS0140-6736(12)X6009-4.
Lancet. 2013. ‘Health in Europe’. Lancet, Global Health Series. Accessed 4 February 2015. http://www.thelancet.com/series/health-in-europe.
Lancet. 2014. ‘BRICS Seek Value for Money as Health-care Costs Rise’. Bulletin of the World Health Organization 92, no. 6: 392–93. http://dx.doi.org/10.2471/BLT.14.020614.
Marten, Robert, Diane McIntyre, Claudia Travassos, Sergey Shishkin, Wang Longde, Srinath Reddy, and Jeanette Vega. 2014. ‘An Assessment of Progress towards Universal Health Coverage in Brazil, Russia, India, China, and South Africa (BRICS)’. The Lancet 384, no. 9960: 2164–71. http://dx.doi.org/10.1016/S0140-6736(14)60075-1.
Monnais, Laurence. 2006. ‘Preventive Medicine and the French “Mission civilisatrice”: Uses of the BCG Vaccine in Colonial Vietnam between the Two World Wars’. International Journal of Asia Pacific Studies 2, no. 1: 40–66.
O'Neill, Jim. 2001. Building Better Global Economic BRICs. Global Economics Paper No. 66. New York: Goldman Sachs. http://www.goldmansachs.com/our-thinking/archive/archive-pdfs/build-better-brics.pdf.
Rao, Krishna D., Varduhi Petrosyan, Edson Correia Araujo, and Diane McIntyre. 2014. ‘Progress towards Universal Health Coverage in BRICS: Translating Economic Growth into Better Health’. Bulletin of the World Health Organization 92, no. 6: 429–35. http://dx.doi.org/10.2471/BLT.13.127951.
Redfield, Peter. 2013. Life in Crisis: The Ethical Journey of Doctors Without Borders. Berkeley: University of California Press.
Stiglitz, Joseph E. 2002. Globalization and its Discontents. New York: W.W. Norton.
UN Sixty-fourth General Assembly. 1981. ‘Global Strategy for Health for All by the Year 2000’. Resolution 36/43. Geneva: United Nations.
Valeska, Huber. 2006. ‘The Unification of the Globe by Disease? The International Sanitary Conferences on Cholera, 1851–1894’. The Historical Journal 49, no. 2: 453–76. http://dx.doi.org/10.1017/S0018246X06005280.
Wang, L., H. Zhang, Y. Ruan, D. P. Chin, Y. Xia, S. Cheng, M. Chen, Y. Zhao, S. Jiang, X. Du, G. He, J. Li, S. Wang, W. Chen, C. Xu, F. Huang, X. Liu, and Y. Wang. 2014. ‘Tuberculosis Prevalence in China, 1990-2010: A Longitudinal Analysis of National Survey Data’. The Lancet 383, no. 9934: 2057–64. http://dx.doi.org/10.1016/S0140-6736(13)62639-2.
Watt, Nicola F., Eduardo J. Gomez, and Martin McKee. 2014. ‘Global Health in Foreign Policy- and Foreign Policy in Health? Evidence from the BRICS’. Health Policy and Planning 29, no. 6: 763–73. http://dx.doi.org/10.1093/heapol/czt063.
Wells, William A., Colin Fan Ge, Nitin Patel, Teresa Oh, Elizabeth Bardiner, and Michael E. Kimerling. 2011. ‘Size and Usage Patterns of Private TB Drug Markets in the High Burden Countries’. PLoS One 6, no. 5. http://dx.doi.org/10.1371/journal.pone.0018964.
WHO (World Health Organization). 1978. ‘Declaration of Alma-Ata’. International Conference on Primary Health Care, Alma-Ata, USSR, 6–12 September. Geneva: World Health Organization.
WHO. 2014. Global Tuberculosis Report. Geneva: World Health Organization. http://www.who.int/tb/publications/global_report/en/.
World Bank. 1993. World Development Report: Investing in Health. http://files.dcp2.org/pdf/WorldDevelopmentReport1993.pdf.
The World Bank Group. 2015. Data. Accessed 4 February 2015. http://data.worldbank.org/