Ambivalent visibility
Chronic illness and image in young adulthood
—
(click on images to view in slideshow mode)
This photo essay represents a collaboration with a group of adolescents and young adults who have cystic fibrosis, a fatal chronic disease. Through fieldwork in Berlin, Germany, we explored how young people – who often do not readily appear to be sick – integrate therapy into their daily lives and manage the visibility of their illness. The story we present below follows Tanja (a pseudonym), a young woman we first met in 2007 at an outpatient clinic, and re-encountered several times over five years. All images were taken during the first year of research by Johannes Rascher, and the text of this essay was written by Stefan Reinsch.
It was a warm summer day in Berlin. Tanja and I met at a photography exhibit in the city centre. She is one of a number of the young adults with cystic fibrosis (CF) whom we followed over time. CF is a rare genetic disease that causes frequent respiratory infections, leading to progressive scarring of the lung tissue. Most people with CF will require a lung transplant at some point in their lives; those who do not receive a transplant often die from suffocation. There is currently no cure for CF, but its progression can by slowed. In Germany, the life expectancy of someone with CF is around thirty-eight years, a number that has been rising over the last decades. Responsible for this increase is not a single new drug, but a more complex and demanding therapeutic regimen, which involves approximately two hours of inhalation and chest physiotherapy every day, and up to seven different oral medications (image 2).
At the entrance to the exhibit, Tanja flashed her disability card and asked for free entry for both herself and me as her ‘accompanying person’. The young man at the desk looked at Tanja with hesitation, his eyes moving between her and the card she held in her hand. He seemed to be assessing whether she was attempting to elicit a benefit to which she is not entitled. Tanja is an attractive young woman in her early twenties. She speaks quickly and confidently. The way she presents herself troubles categorizations like healthy/ill and able/disabled, and the squaring of illness and unattractiveness (Hall 1997). Tanja doesn’t fit the stereotypical image of someone who is ill or disabled, and therefore requires someone to accompany her. Yet, the card she showed the man at the desk defines her in exactly this way, rendering her in some ways unintelligible. This unintelligibility is a part of the burden of living each day as a young person with a fatal chronic illness.
The difficulty in ‘sorting out’ Tanja (Bowker and Star 1999) reveals her double status as someone who is at once ill and apparently healthy. At least for the time being, Tanja’s illness is made invisible by a set of therapeutic practices. CF therapy has traditionally taken place in hospitals. But, increasingly, the space of therapy is becoming fluid, as procedures like inhalation, chest physiotherapy, and the delivery of intravenous (IV) antibiotics occur in young people’s homes. For this to occur, certain technical innovations were essential – such as replacing the standard and somewhat clumsy hospital infusion pump with a smaller pump that resembles a compressible ball. Patients can slip this smaller pump into a trouser pocket, running the IV line under their shirtsleeves. Moving therapy out of the hospital means greater freedom for young people living with CF, but it also requires them to integrate therapy into the practices of everyday life, particularly in the home.
Of all the adolescents and young adults I followed, Tanja seemed to be especially open in the way she managed her condition at home. In Tanja’s apartment, a handful of pills lay on the kitchen table. I recognized them as the pancreatic enzymes many young people with CF have to take with every meal so that the body can absorb nutrients. On a nearby shelf, there were boxes of vitamins, anti-inflammatory drugs, and antibiotics. Another box of antibiotics was in the fridge, next to the cheese. Beside a bookshelf was Tanja’s nebulizer, which is a handheld device the size of a small bottle. Through a mouthpiece on the top of the device, Tanja inhales hypertonic saline for up to thirty minutes twice a day in order to dilute the mucus that builds up in her lungs.
On one of the many occasions when Tanja’s physiotherapist visited in the middle of the afternoon, the two of them began by catching up on the latest news and events: patients who had gotten better lately or taken a turn for the worse, and plans for holidays. Only after socializing did Tanja lie down on the couch to begin chest physiotherapy. This therapy involves chest compression and decompression, which mobilizes the mucus in the lungs that can then be coughed up slowly (images 4 and 5). As she underwent this therapy, Tanja’s face became red. The room was silent except for her repeated coughing. These moments of coughing were a stark contrast to the casual social encounter that began the thirty-minute-long session; suddenly, Tanja’s illness was starkly visible. After one seemingly endless minute of exertion, Tanja spat the mucus into a small sealable container and the chatting continued.
For young people living with CF today, there is a constant blurring of lines between therapy and everyday life, medicine and social relationships. Tanja described to me how the dramatic intensity of life with CF can lead to close relationships. Patients fall in and out of love, and sometimes marry. Patients and medical staff go to concerts or on vacations together. One doctor remembered being called on the phone in the middle of the night by a patient who had gotten lost on the highway while hitchhiking. As one adjusts the focus, things that are kept apart at first glance turn out to be highly entangled.
These kinds of entanglements have implications for the research process. At the beginning of this project, I was warned by the staff at the CF clinic that they have seen several of their younger doctors become emotionally attached to patients who later died. During the first year of research, three of the fifteen patients I followed died. But Johannes and I found that the emotional attachments we formed with some of the young adults we followed were fundamental to our photo-ethnography – and in some ways difficult to avoid. We were similar in both age and interests to many of our young collaborators; they, in turn, were often enthusiastic about reflecting on the ambivalence of their visibility in the context of our work together (Schaffer 2008).
 Image 6. The more therapy they do, the better they look. But the better they look, the higher the expectations are.
Image 6. The more therapy they do, the better they look. But the better they look, the higher the expectations are.That same night that her physiotherapist visited, Tanja came out of her room before bed to put a gastric tube through her nose. She connected it to a bag of high-caloric food that will be ingested automatically while she sleeps. These extra calories are essential to meeting the increased energy demands experienced by people with CF, whose bodies are in a constant inflammatory state as a result of fighting chronic respiratory infections and generally have to work harder to breathe. The gastric tube is not a comfortable procedure; in fact, Tanja only knows of only a few other people who do it. ‘I also usually do not show this to anyone’, she laughs. Doing but not showing is one of the tactics that enable her to look ‘normal’ most of the time. Another tactic she employs is the quick cover-up, like stuffing pills directly into a sandwich instead of taking them with liquids during a meal. She also disguises her medical equipment to the best of her ability: when she needs IV antibiotics, she makes the cotton gauze that covers the IV line on her forearm a little thicker, transforming it into a ‘sweatband’ so that the line isn’t as visible. Tanja also takes cortisone before going to nightclubs, where the cigarette smoke could trigger her bronchial hyperreagibility and lead to the constriction of her airways. These kinds of strategies are precarious, and can fail at exactly the wrong moment. But most of the time they work out quite well.
The next morning, after Tanja used her inhalation machine for half an hour while reading a book, we drove by the office were she had worked until recently. She recalled, ‘At work I had to justify myself whenever I was late – that I just did my inhalations and wasn’t lazy. It’s difficult to explain every time – even some people who work with you don’t seem to understand’. Tanja remembered a colleague who had told her about how one of his acquaintances had gotten a renal transplant, and how horrible that idea was to him. ‘I was struck with disbelief’, she said, shaking her head. ‘I told him I might need a lung transplant in the not so distant future. He didn’t get it – perhaps I still look too good?’
The more therapy young people like Tanja do, the better they look. But the better they look, the higher people’s expectations are regarding their level of functioning. As one of Tanja’s friends, who is still working, told me during an interview, ‘I consider doing my therapy, in the way that it now fits into my life, as a disadvantage, because you don’t belong to any group. You are not part of the ill ones … but neither are you part of the healthy ones. That makes it difficult, because you have to justify yourself wherever you try to integrate yourself [into either group]. You are not part of any group, and you have to excuse yourself for what you don’t have – illness or health’.
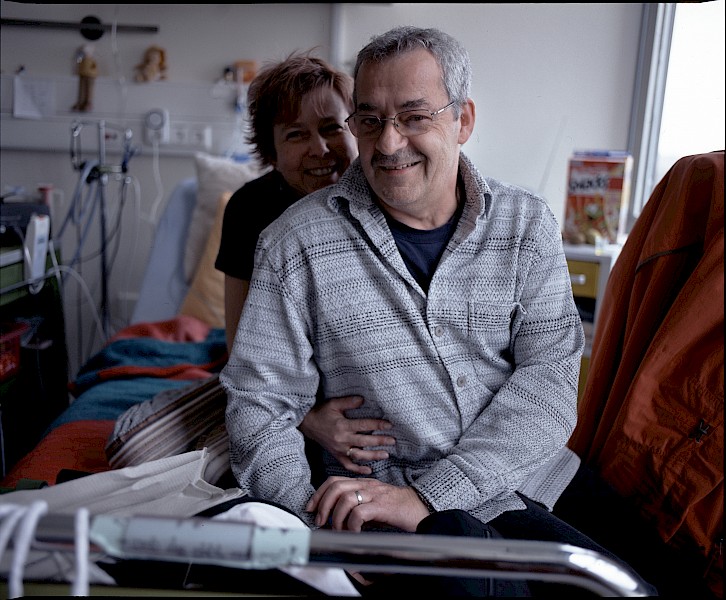 Image 7. The visibility of their illness is also a resource that can be used to gain support and care.
Image 7. The visibility of their illness is also a resource that can be used to gain support and care.With the help of a very complex and demanding therapeutic regimen, people with CF are able to make the symptoms of their illness invisible, thus allowing them to acquire a new – albeit temporary – healthy self. They become ‘immigrants to health’, to turn around Susan Sontag’s (1978) phrase. Acknowledging the burden of therapy they face, and claiming the kinds of social support to which they are entitled as ‘disabled’ people, may come with the loss of a sense of belonging in the world of the able bodied. This was a kind of temporary citizenship that many young people deeply desired.
The visibility of their illness is ambivalent: while it excludes them from the group of the healthy ones, it is also a resource that can be used to gain support and care. Yet, this ambivalence can only be navigated to a certain extent. The double status of someone with CF – at once inherently ill and apparently healthy – results in their unintelligibility, as most outsiders try to sort them into one group or the other.
About the authors
Stefan Reinsch is a medical doctor and anthropologist working at the Department of Pediatric Pneumology and Immunology, Charité–University Hospital, Berlin, Germany. In 2013–15 he was a postdoctoral researcher at CERMES3, Paris, where he investigated the entanglements of clinical and scientific work in the negotiations around the diagnosis of ‘at-risk mental state’ in French- and German-speaking psychiatry. This essay draws on his PhD research about the strategies young people with cystic fibrosis use as they integrate their therapy into daily life.
Johannes Rascher is a photographer from Hamburg, Germany. Some of Johannes’s work can be found on http://jrascher.tumblr.com.
References
Bowker, Geoffrey C., and Susan Leigh Star. 1999. Sorting Things Out: Classification and Its Consequences. Cambridge, MA: MIT: Cambridge.
Hall, Stuart. 1997. Representation: Cultural Representations and Signifying Practices. London: Sage: London.
Schaffer, Johanna. 2008. Ambivalenzen der Sichtbarkeit. Bielefeld: Transkript.
Sontag, Susan. 1978. Illness as Metaphor. New York: Farrar, Straus & Giroux.




