From superstition to folk medicine
The transition from a religious to a medical concept
—
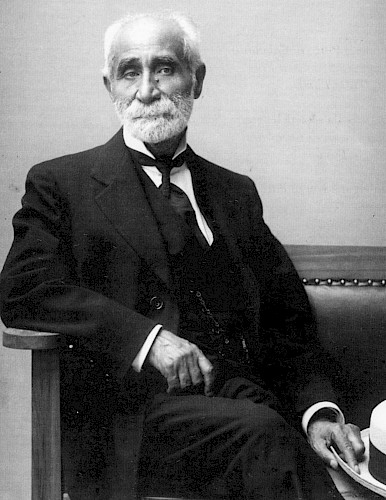
Giuseppe Pitrè, source: Calandra Italian American Institute http://qcpages.qc.cuny.edu/calandra/intrepid-giuseppe-pitrè-and-his-collection-sicilian-folk-tales
Twenty years after (1996–2016)
Between 1981 and 2005, I taught a course on the history of anthropology at my university. Although I am both an anthropologist and a doctor, I have always approached this course from the perspective of a historian of science specializing in anthropology, medicine, and psychiatry. I followed George Stocking’s (1968) advice concerning historiographic presentism in the history of science and sharing Verena Stolcke’s (1993) critical position on the lack of rigor in many histories of anthropology. Methodologically, I chose to distinguish between the history of anthropology as a ‘discipline’, the history of anthropology as a ‘profession’ (Comelles and Prat 1992, 40–42) – in the sense in which Eliot Freidson (1988) used this word – and the history of ‘ethnography’ as a fieldwork practice and resulting literary genre distinct from both ‘geography’ and ‘history’.
The term ‘ethnography’ was coined in Germany at the end of the eighteenth century (Vermeulen 1995), at the same time that the German physician Ludwig Finke (1795) proposed the synonymous term ‘anthropography’ to designate ‘medical topographies’, one of the ethnographic genres written by medical doctors. While I have not explored the reasons why ‘ethnography’ won out over ‘anthropography’, I would like to point out here that both concepts emerged after centuries of the writing and publication of ‘ethnographic-like’ narratives (Comelles 1998; Elsner and Rubies 1999). Today historians have no problem categorizing as ‘ethnography’ or ‘ethnology’ those texts written before the invention of these concepts (see for example Momigliano 2000). We see them not as the product of simple curiosity on the part of their authors, but as instruments for the production of knowledge in certain professions, especially by physicians, clerics, and jurists.
By the mid-1980s, I had found that recognizing the existence of ethnography avant la lettre and taking it seriously as something central in the production of medical knowledge was an attractive line of inquiry. At that time my double identity as both doctor and anthropologist was highly unusual, and medical anthropology was only beginning to be recognized as a distinct field of study. For many anthropologists, it was spurious because it was seen as merely applied. Some senior anthropologists went so far as to claim, without blinking, that it wasn’t even anthropology. Documenting my view of ‘ethnography’ as a professional practice of doctors prior to the development of professional anthropology allowed me to examine its meaning and its implications for both medical practice and what we now call the ‘process of medicalization’. It also allowed me, with some irony by my side, to explain that doctors played a crucial role in the development of anthropology from the eighteenth to the twentieth century, not just in debates on nineteenth-century evolutionism but because they were fully in command of the conventions of what I call ‘neo-Hippocratic ethnography’, inspired by criteria already present in the Hippocratic treatises. These ethnographies, treated as ethnographic sources, have been one of my objects of study for the past three decades (see Comelles 1996, 1997, 1998, 2000; Comelles and Perdiguero-Gil 2014). Working with these sources has allowed me to document their continuity through time since antiquity and their influence on certain ‘medical’ narrative genres, principally ‘medical topographies’; writings classified as ‘medical folklore’; treatises on superstitions, errors, and ‘commonly presumed truths’ that proliferated between the sixteenth century and the end of the nineteenth century; and travel writing of an ethnographic character produced by doctors, one of the best examples of which is Anton Tchekhov’s report of prison conditions on Sakhalin, an island off the eastern coast of Siberia, published in 1895.
In 1992, after a decade of working on this topic, and in order to prepare my course on the history of anthropology, I was invited, together with a colleague and friend, Angel Martínez-Hernáez, to write a book, an article, and a book chapter on the relationships between medicine, psychiatry, and anthropology (Comelles and Martínez-Hernáez 1993; Martínez-Hernáez and Comelles 1994; Martínez Hernaéz, Orobitg, and Comelles 2000). A decade later, Martínez-Hernáez (2008) would complete this task in a detailed analysis of the role of medicine in anthropology’s theoretical agenda. Our main contribution was to demonstrate how biomedicine reduced ethnography to a subaltern practice and narrative genre in the twentieth century at the same time that professional anthropology turned the study of medicine into a subaltern research genre.
The genealogy of ideas we established led me to do more systematic research. Initially, I planned a longue durée study of the transhistoric, professional, and political meanings of ethnography for doctors and missionaries, and another, more specific project that produced the present article (Comelles 1996, 1997). What occupies my attention in this piece, which focuses on the period between the late nineteenth century and the mid-twentieth century, is the process through which ‘folk medicine’ became one of the foundations of present-day medical anthropology following its ‘medical invention’ as a concept in the nineteenth century. I had observed that classic notions such as ‘superstition’ had been displaced by the invention of the concept of ‘popular’ or ‘folk’ medicine as a modern medical concept that was necessary for achieving the aims of the process of medicalization.
My point of departure was my relationship with colleagues in Perugia: Tullio Seppilli (1983), and Paolo Bartoli and Paola Falteri (1987), who introduced me to Italian medical folklore and the role it had played in the development of Italian medical anthropology. The library of Università degli Studi di Perugia has in its collection a wealth of sources that allowed me to prepare a first draft that I presented in two colloquia, one in Santiago de Compostela and the other in Granada. Seppilli suggested that I publish it in Italian because he thought my analysis of the invention of folk medicine shed new light on the role of Italian doctors in the medicalization of peasants following the Risorgimento.[note 1] My argument was that ‘folk medicine’ existed as a concept and object of medical study with medical significance since the work of Giuseppe Pitrè (1986). He explicitly offered a methodology for the development of a specific field of study, established the need for recognition of its practical efficacy and made evident the professional commitment of its practitioners to the people who were their objects of study. His methodology is the foundation of an empirical medical anthropology that emerged from medicine itself with a clearly applied aim, and this fitted well with my hypothesis on the role of ethnography in the construction of medical knowledge.
Not long after, Giordana Charuty (1997) and Nicoletta Diasio (1999), unaware of my article, read the same materials as I had and reached similar conclusions, confirming my work independently. In Italy my article became an indispensable source on folk medicine and how neo-Hippocratic ethnography, in dialogue with folklore studies, allowed for the development of a Sicilian medical kulturkreis (cultural field). None of the three of us could fully explain why Pitrè’s influence was limited to Latin countries and especially to Spain and Italy, where doctors continued to do research on medical folklore until the fifties. The folklorist Alfonso De Nino (1891), who was not a doctor, argued that folk medicine was necessary in Italy because there was no medical alternative for impoverished peasants, and the doctors of his time agreed with him. In southern Europe, as medicine became established in rural areas and in the marginal districts of European cities, medical folklore as described by the medical folklorists disappeared (Comelles and Perdiguero-Gil 2014). Today it exists only as cultural archaeology, but the idea of folk medicine as complex local knowledge about processes of health, illness, and care is an undeniable reality in all countries. The pluralism of a wide range of highly varied resources – including biomedicine – corresponds to the foundational concept of folk medicine as a specific object of study, as defined by Giuseppe Pitrè.
About the author
Josep M. Comelles, MD, PhD (Barcelona, 1949), is Professor Emeritus of the Medical Anthropology Research Center of the Universitat Rovira i Virgili in Tarragona (URV). He has worked as a medical anthropologist and historian of science on public policies, health institutions, medical pluralism, and folk medicine. Susan DiGiacomo is a full professor in medical anthropology at the URV; she translated ‘Twenty Years After’, and reviewed the translation. Mary Savage is a translator with the Servei Linguistic of the URV, who translated ‘From Superstition to Folk Medicine’, the article that follows.
References
Bartoli, Paolo, and Paola Falteri. 1987. ‘La medicina popolare in Umbria dalla fine dell’800 ad oggi: permanenze e transformazioni’. In Sanità e Società: Emilia-Romagna, Toscana, Marche, Umbria, Lazio Secoli XVI–XX, edited by Alessandro Pastore and Paolo Sorcinelli, 167–208. Casamassima: Electa.
Charuty, Giordana. 1997. ‘L’invention de la médecine populaire’. Gradhiva 22: 45–57.
Comelles, Josep M. 1996. ‘Da superstizione a medicina popolare: La transizione da un concetto religioso a un concetto medico’. AM. Rivista della Società Italiana di Antropologia Mèdica 1–2: 57–87.
Comelles, Josep M. 1997. ‘De las supersticiones a la medicina popular: La transición de un concepto médico a un concepto religioso’. In Medicina Popular e Antropoloxia da saude, edited by Xose M. González Reboredo, 247–80. Santiago de Compostela: Consello da Cultura Galega.
Comelles, Josep M. 1998. ‘From Ethnography to Clinical Practice in the Construction of the Contemporary State’. In Democracy and Ethnography: Constructing Identities in Multicultural Liberal States, edited by Carol J. Greenhouse, 233–53. Albany: State University of New York Press.
Comelles, Josep M. 2000. ‘The Role of Local Knowledge in Medical Practice: A Trans-historical Perspective’. Culture, Medicine and Psychiatry 24, no. 1: 41–75.
Comelles, Josep M., and Joan Prat. 1992. ‘El Estado de las Antropologías. Antropologías, folclores y nacionalismos en el Estado Español’. Antropologia 3 (October): 35–61.
Comelles, Josep M., and Angel Martínez-Hernáez. 1993. Enfermedad, cultura y sociedad: Un ensayo sobre las relaciones entre la antropología social y la medicina. Madrid: EUDEMA.
Comelles, Josep M., and Enrique Perdiguero-Gil. 2014. ‘El folklore médico en la nueva agenda de la antropología médica y de la historia de la medicina’. In Antropología médica en la Europa meridional 30 años de debate sobre pluralismo asistencial, edited by José M. Uribe Oyarbide and Enrique Perdiguero-Gil, 11–51. Tarragona: Publicacions URV.
De Nino, Alfonso. 1891. Usi et Costumi Abruzzesi descriti da... Volume Quinto Malattie e Rimedi. Florence: Tipografia di G. Barbera.
Diasio, Nicoletta. 1999. La science impure: anthropologie et médecine en France, Grande-Bretagne, Italie, Pays-Bas. Paris: Presses universitaires de France.
Finke, Ludwig L. 1795. Versuch einer allgemeinen medicinisch-praktischen Geographie, worin der historische Theil der einheimischen Völker und Staaten Arzeneykunde vorgetragen wird, 3 vols. Leipzig: Weidmannschen Buchhandlung.
Freidson, Eliot. (1970) 1988. Profession of Medicine: A Study of the Sociology of Applied Knowledge. Chicago: University of Chicago Press.
Elsner, Jan, and Joan-Pau Rubiés, eds. 1999. Voyages and Visions: Towards a Cultural History of Travel. London: Reaktion Books.
Martínez-Hernáez, Ángel. 2008. Antropología médica: Teorías sobre la cultura, el poder y la enfermedad. Barcelona: Anthropos.
Martínez-Hernáez, Ángel, and Josep M. Comelles. 1994. ‘La medicina popular ¿Los límites culturales del modelo médico?’ Revista de Dialectología y Tradiciones Populares 39, no. 2: 109–36.
Martínez-Hernáez, Ángel, Gemma Orobitg, and Josep M. Comelles. 2000. ‘Antropología y Psiquiatría: Una genealogía sobre la cultura, el saber y la alteridad’. In Psiquiatria transcultural, edited by Emilio González and Josep M. Comelles, 117–243. Madrid: Asociación Española de Neuropsiquiatría.
Momigliano, Arnaldo. 2000. La Sabiduría de Los Bárbaros: Los Límites de la Helenización. México: Fondo de Cultura Económica.
Pitrè, Giuseppe. 1896. Medicina popolare siciliana. Turin: C. Clausen.
Seppilli, Tullio. 1983. ‘La medicina popolare in Italia: Avvio ad una nuova fase della ricerca e del dibattito’. La Ricerca Folklorica 8: 3–7.
Stocking, George W. 1968. Race, Culture, and Evolution: Essays in the History of Anthropology, with a New Preface. Chicago: University of Chicago Press.
Stolcke, Verena. 1993. ‘De padres, filiaciones y malas memorias: ¿Qué historias de qué antropologías?’ In Después de Malinowski, edited by Joan Bestard, 147–98. La Laguna: Asociación Canaria de Antropólogos-FAAEE.
Tchekhov, Anton. (1895) 1971. L’ile de Sakhaline: Notes de voyage. París: Gallimard.
Vermeulen, Hans F. 1995. ‘Origins and Institutionalization of Ethnography and Ethnology in Europe and the US, 1771–1845’. In Fieldwork and Footnotes, edited by Hans F. Vermeulen and Arturo Alvarez-Roldán, 39–59. London: Routledge.
From superstition to folk medicine:
The transition from a religious to a medical concept
To Paolo Bartoli, Tullio Seppilli, and Paola Falteri
In Alejandro Guichot y Sierra’s ([1922] 1984) Historia del Folklore, ‘folk medicine’ – rendered in Spanish as medicina popular – appears in only four pre-1900 books referring to popular beliefs about and practices for the prevention or treatment of illnesses.[note 2] Instead, we find references to ‘superstition’, ‘error’, ‘uses and customs’, ‘concerns’, and ‘prejudices’. The term ‘folk medicine’ is also largely absent from the popular medical publications that Guichot bypassed in his history.[note 3] Attention to popular therapeutic or preventive practices is not exclusive to these two genres; they are also referred to in treatises on practical medicine and medicinal botany, instructions for prescriptions and pharmacology books, theological texts and records of pastoral visits, and the medical writings known as ‘medical topographies’. They contain ethnographic accounts, some first-hand, some based on secondary sources, others plagiarized or translated, many repeatedly republished.[note 4] We may entertain reasonable doubts about their reliability not only because of the conditions in which observations were made, but also because the authors’ aims and the meanings they attributed to them have little to do with present-day ethnology or anthropology (Comelles 1998).
This article is an attempt to uncover the original meanings of concepts like ‘superstition’ and ‘folk medicine’.[note 5] Doing so will enable us to understand the contradictions that emerge from the uncritical way they are interpreted today [in 1996] by anthropologists. We need to examine the context in which the Spanish and Italian term ‘medicina popular’ (folk-medicine in English) was coined at the end of the nineteenth century in southern Europe,[note 6] and ask why the notion of ‘superstition’ survives in twentieth-century European folklore. When professional anthropology identified ‘folk medicine’ as a specific field of study in the 1950s and 1960s (Comelles and Martínez-Hernáez 1993, 40–46), why did they simply accept Ackerknecht’s (1984) terminology rather than subjecting it to critical analysis?[note 7]
Only Italian anthropology endeavoured to explore this question. The work of Cirese (1978) and Bronzini (1983) on Italian positivist medical folklore[note 8] represents a step in this direction, although they seem to be more interested in what it meant in the context of the Italian bourgeoisie’s ideological project than in uncovering its specific nature. I believe this reductionism prevents them from identifying a fundamental aspect of the origin of the concept of ‘popular medicine’ as the basis of modern ‘medical folklore’: its interest for medical practice, which differentiates it from other fields of study in anthropology. Bartoli (1985) and Bartoli and Falteri (1987) take this up, linking studies of ‘popular medicine’ to the development of modern health care in the Italian unitary state. Their work connects the relationships between ‘popular’ and ufficiale medicine to the role of physicians as organic intellectuals shaping the dominant values of the bourgeoisie concerning the understanding, interpretation, and management of popular beliefs and practices relative to illness (Bartoli and Falteri 1989). Those who used the concept of ‘popular medicine’ were, on the whole, physicians. Their main interest lay not only in making a contribution to folklore or anthropology, but in identifying a space of transactions between popular knowledge and medicine.
My hypothesis is that the construction of ‘popular medicine’ in southern Europe is the result of three intellectual operations: the strategic need to mark the cultural limits of the medical model, the tactical need to establish precise boundaries between what was religious (especially Roman Catholic) heritage and what belonged to medicine, and what was required to fully medicalise European peasant societies.
Of superstitions, errors, and prejudices
The master of superstition is the people; and in all superstition wise men follow fools;
and arguments are fitted to practice, in a reversed order.
– Francis Bacon, Essays, Civil and Moral
When Aquinas turned to the study of ‘superstitions’ (Aquino 1955, 223–44), an old term of classical origin commented on by Isidoro de Sevilla (Del Río 1611, 11–13), he relied on an empirical classification criterion influenced by Aristotelianism.[note 9] For Aquinas, the problem lay in defining the distance between dogma, practices, and popular knowledge. He set out to establish boundaries as precise as possible that would allow the guardians of orthodoxy – confessors, preachers, and inquisitors – to identify and classify ‘superstitions’ and ‘idolatry’. Caro Baroja (1967, I:30–31) argues that once the theological debate was over and the Church had developed specific practices – inquisitorial or penitential – these were no longer grounded in theology but in legal and clinical practice.[note 10] One of the classical authors writing about the techniques of confession said: ‘The confessor who, in addition to paternal charity, needs both the knowledge of the judge and the skill of the physician [and has to] acquire the physician’s abilities’ (Gaume 1864, 64).
Parish priests, preachers, confessors, and inquisitors – jurists and men of law rather than speculative theologians – were inclined toward the rational examination of events and testimonies.[note 11] In their interactions with accused or penitent individuals they had to bridge the gap between organic discourses and specific cases, acting as mediators between sacred texts and the people.[note 12] These adjustments were not exclusive to either religion or law. Studies on the relationship between physicians, patients, and their social networks in specific cultural contexts reveal the complex development of syncretic languages that articulate and combine the ‘popular’ and the ‘learned’, the ‘rational’, the ‘nonrational’, and subjectivity (Good 1994). Exploring the techniques these culture brokers used to secure their social position is no easy task, and requires attention to the dialectical relation between mediators and the people in order to understand how subjective experiences are recovered and how they shape popular knowledge.
When Luther and Calvin attacked superstitions, miracles, relics, and saints, they believed – correctly – that they undermined biblical teachings, suspecting that the Church’s strategic interests facilitated collusion in the construction of these beliefs. Catholic scholasticism adopted a less intransigent position concerning these practices. The scholastics, aware of the significance of relationships between hegemonic and subaltern discourses and practices, did not treat them as antithetical because they knew that these subaltern practices allowed the Church bureaucracy to maintain its hegemony. The rejection of ‘superstitions’ by Calvin and Luther came at the cost of destroying the saints’ cults that offered believers comfort, protection, healing, and safety, and on which the Church’s hegemony was constructed (Delumeau 1989; Comelles 1995, 1993). The theological purity of the reformers prevented them from seeing, initially, how fundamental these practices had been in establishing the intellectual hegemony of religion. The paradox of the Reformation is that although it aimed to purify Christianity of its nonbiblical accretions, it soon had to compromise over certain popular practices and rituals associated with individual and collective appeals to semi divine figures for protection from misfortune and intercession with God on their behalf.
However, the Council of Trent – the counter-reform performed by the Roman Catholic Church[note 13] –proposed no such radical break, sensing that this would dismantle the centralized Church bureaucracy and promote its fragmentation into local structures. For this reason it accepted certain superstitious practices, attempted to regain control over others, and encouraged the faithful to seek healing and protection not through the veneration of saints but through devotion to the Virgin Mary (Woodward 1990). It thus guaranteed the persistence of mediation in health and illness based on saints, virgins, relics, and sanctuaries, and enabled the continuity of transactions between the faithful and the clergy, who were charged with the task of keeping compromises between theological discourse and popular practices and beliefs within bounds (Brown 1981). While they had to preach dogma, they also needed to interpret its limits (Comelles 1996c). They could take a hard line, but often they were guided by local knowledge and participation in local society, their personal commitment situated on the boundary between their dual status as members of the Church and as members of the community who must also understand their neighbours.[note 14] It is not possible to draw a sharp line separating licit practices from superstitious ones, since the boundary must adapt to local cultural reality if hegemony is to be maintained. For this reason the notion of superstition must be built on ethnographic practice drawing from religion and not medicine.
The compromises the Trent intellectuals made with subaltern religious practices led to three attitudes. First, they led to one of credulity – or perhaps cynicism – represented by Del Río’s (1611, 472) treatise on magic, which claims genuine belief in the interventions of demons or similar beings in the origins of superstition and bolsters an argument against ‘vain observances’ with ethnographic data:
For example, someone makes an offering of alms he has received, believing it to be more efficacious for this reason. Someone believes that a cross which he has bought or had made and paid for with money he has received as alms is more holy or efficacious as a result. People make offerings of wax or other substances to the saints, mixing into it the hair of a sick person or sick animal. They tie knots so that their cow’s milk may not fail.
The second attitude is represented by the Jesuits’ effort to establish a precise catalogue of cases that could be used in the teaching of law to define the boundaries between licit and illicit. According to Tullio Seppilli (personal communication), the Church morally disapproved of ‘superstitious practices’ but believed in their efficacy, whereas medical doctors were indifferent to their moral dimension and believed them to be ineffective. The Church’s ambiguity reflects its awareness of the blurred, changing boundaries between ‘faith’ and ‘superstition’. These boundaries required circumstantial modifications depending on the Church’s political position at any given historic moment. Sometimes it was convenient for it to condemn healing using natural methods even in a context in which technical medicine did not provide an effective cure and too closely resembled the practices of folk healers and charlatans. It was a way of placing medicine at the edge of what was licit, and a way of controlling physicians who dared to challenge the Church.[note 15]
The third attitude, rationalist or enlightened, shared by the Church doctors and some clerics, aimed to recover what could be useful in ‘superstitions’, such as certain empirical therapies, and to reject what was quackery or blind credulity. Monks like Feijóo (1757) in Spain criticized ‘errors’ and ‘superstitions’ at the same time that physicians such as Buchan (1785) and Tissot (1776) tried to popularize scholastic medicine. According to Caro Baroja (1967, II:326), not only the clergy but also the physicians were experiencing an ideological transition that would lead them to suspend unquestioning belief in everything. This suspension of belief required regulated formal education for the population.[note 16] Barreiro ([1885] 1973, 29) wrote that it was:‘A difficult task but one worthy of the greatest attention for all those men who, devoting their lives to the education of the masses and enlightenment, must thoroughly know, in order to combat those harmful, certain superstitions and beliefs that are still deeply rooted in our peasants’ hearts’.
Nevertheless, relations between clerics and doctors have always been ambivalent and contradictory, oscillating between periods of condemnation and of compromise. As Ware (1849, 34) wrote: ‘now it is very obvious that an Enlightened physician may do much to promote religion, morals and the cause of education. He may, with his example and that of his family, aid in raising the standard of mental and moral cultivation’. In 1875, Samuel Gross, in his valedictory address to the graduating class of the Jefferson Medical College in Philadelphia, urged his classmates to acknowledge their technical limitations and not regard themselves as an alternative to priests or ministers: ‘Many persons imagine that the physician is omnipotent, and therefore, capable of performing miracles forgetting that it is appointed unto all men once to die. Of the many cases of disease and accident which daily fall under his supervision there are always some which must inevitably be mortal, or in which the only balm in Gilead is temporary relief for suffering or a brief prolongation of life’ (Gross 1875, 8).
For this reason, the priest was not the doctor’s enemy but his ally: ‘In the country, only with the priest can you hope for useful and agreeable relations. He will give you topographical information, moral notations and domestic details about his parish. He is frequently the one who holds the secret of deciding to operate on a patient. In your absence he can oversee your prescriptions, read them, explain them, correspond with you and help you in advancing hygiene and vaccination’ (Munaret 1840, 21). From the Enlightenment onwards, some doctors and apothecaries denounced the inhibition of the state in order to fight against the ‘plague’ of quackery: ‘in our public squares, in the fairs and at the shrines, the blind man, the degenerate minstrel of our times, flying the flag that represents the most stupid crimes and miracles, hawks and sells among his detestable verses books of receipts for curing all class of ailment without the necessary approval of the Health committees’ (Barreiro 1973, 29).
Those who engaged in ‘stupefying and cheating the people with miraculous verses must not be tolerated, and much less so the sale of such a class of pamphlets, and also the advocating of certain theories and the public practices of quack doctors that frequently cause considerable harm’ (Barreiro 1973, 54). In Galicia, a remote and impoverished area in northwestern Spain, one such text was the widely distributed Libro de San Cipriano (Great Book of St. Cyprian), a compendium of instructions for curing diseases, occult practices, and prayers. Barriero noted that:
copying to the letter various chapters of the famous book of St. Cyprian, will denote the degree of instruction that with such masters and under such Spanish monarchs did reach this abandoned and neglected Galician people at the end of the nineteenth century; requiring for our part, not only a vigorous protest against the centralizing governments and laws that senselessly stifle with our intelligence the most fertile seeds of the prosperity of the State, and weaken it and dishonour it before the learned world with the violent death that all Galicia’s liberal aspirations suffer. (Barreiro 1973, 69)
To counter these ideas, doctors wrote books of popularization. The Galician doctor Rodríguez López (1974, 12) placed great store by the power of the written word to identify and discredit superstitious health beliefs:
The aim of this booklet is none other than to collect superstitions so that one day they might serve our curiosity for the historic. At the same time, I propose to show all those swindlers, readers of the cards, healers, etc., that we know those practices and those incantations that they hide so and in whose mystery they forge the virtue they attribute to them in order to advance their fraudulent industry. My prime and most cruel enemies are those who still have faith in the superstitions I point to. Let all superstition be known, let it be seen from whence they come, that it be known why some have interests in supporting them, and celebrate the absurdities they contain; these were also reasons that have guided my pen in tracing the lines of this book I present to you, modest for it is mine, and incomplete because given the short time I disposed of for its writing, many data will surely be missing.
He also called for educational reforms to combat ‘superstition’:
For this reason I believe that one of the main causes of superstition in Galicia is the lack of attention by teachers and priests, the two authorities most respected in rural areas, to these beliefs. They should destroy them, analysing them error by error and enlightening the people in the truths that quell their worries. But this does not happen. On the contrary, I have never heard that the priests prohibit telling children stories of goblins, witches, imps; etc. The parents, and especially the grandparents, take pleasure in contemplating the attention and enthusiasm with which the innocent creatures listen to these stories, which they refer to as certainties. (Rodríguez López 1974, 74)
For Rodríguez López, collecting health superstitions was a consequence of his medical practice, in rural Galicia, and his hope was that in the future, his book would help to reduce them to mere ‘historical curiosities’:
For some time now my curiosity has led me to commit to memory or note down the superstitions that reached my ears or that I observed in the villages where I have carried out my profession or my affairs; but it is possible that it would not have occurred to me to perform a special study of the superstitious beliefs of the Galicians had the question not been proposed for a literary-musical event. It is known that many of the things we consider as superstitions today have not always been so and, on the contrary, were taken as articles of faith, as incomplete truths. This booklet has no other purpose than to collect superstitions so that at some future date they might serve as a historical curiosity. (1974, 12)
Although Rodríguez López, unlike Barreiro, did not write his book as a polemic, his criticism of priests’ attitudes toward popular superstition provoked a violent reaction from the bishop of Lugo. He had crossed a fine line, identifying certain practices endorsed by the Church as superstitions. His case is evidence of a crisis in the old compromise between physicians and clerics, and the rising hegemony of positivist medicine allied with the secularizing politics of liberalism. By the end of the nineteenth century, healing had become a fundamental objective of a medical model in which all resources, including deceit and lies, were valid:
Often in hospitals and in ordinary practice, to respond to the requests of sick persons who demand to be treated, the physician has to prescribe things that, like pills made of breadcrumbs, have no effect on their state of health. And by contrast, as an effect of the workings of their imaginations some tell of improvements. And this sensation is real, and it is proportional to the trust of the patient in many cases, and imposes on the physician the duty to intervene even in incurable illnesses for which his remedies are ineffective. The mission of science is not to deaden the hope in the heart of sufferers and persuade them they are irretrievably lost. Dumas fils tells us that when God said that lying was a sin, He made an exception for physicians and allowed them to lie as many times in a day as ill people they saw. The physician must in certain cases take advantage of the credulity of those who call upon him. (Grellety cited in Bonniot 1879, IV).
For positivist physicians enlisted into the struggle against religious obscurantism, belief in miracles and apparitions upheld by the Church was steeped in magic and superstition. Doctors rejected miracles, explaining illness and cure by reference to nature or human intervention. Miracles belonged in the same category as ‘suggestion’ or ‘mesmerism’, and doctors urged that:
haste must be made in demolishing the work of prejudices and ignorance. The sources of superstition are like sources of epidemics. We are obliged to accept that miraculous cures are true cures, but they are presented as the effect of heavenly intervention and are surrounded by miracles and apparitions. They are prudent lies, perhaps even useful; but although they are beneficial, they are lies, and that is enough for them to be rejected. (Grellety cited in Bonniot 1879, III)
Bonniot, a Jesuit, replied that:
what physicians do not accept is the supernatural… . The rationalist physician accepts the facts, but their horror of the miracle leads them to interpret these facts in their own way, striving to find natural causes and accepting only the healings that they can explain, such that the historical truth spreads insofar as their mind acquires either more knowledge or more capacity for penetration. In the end, physicians turn to faith, to which they attribute surprising therapeutic virtue that seems to be absent from their remedies. But the conception they have of faith is that it is an abnormal state, characterized by a struggle between the will that dictates and reason that resists. Hence there is a struggle in the nervous system, which is the essential agent of healing. (Bonniot 1879, II)
Although Bonniot wanted to clarify how superstitious practice works, his argument is based on an individualized relationship between healer and patient that is very close to the medical model:
What physicians call a prudent or merciful lie is not a question of science but of medical practice: it is not a question of demonstrating, but of providing relief, and if possible, healing. From this point of view, the prudent lie is permitted and it is a duty: but what physicians call a merciful lie not only alleviates but also cures at Lourdes, and does so in illnesses over which the physicians’ real lies have no more power than their remedies. Hence it is not the merciful lie that worries the physicians. (Bonniot 1879, V)
His aim was to construct a clear, precise boundary separating science from religion:
His aim was to construct a clear, precise boundary separating science from religion:
Branding as lies the events that inspire a pilgrimage is to abuse the word. The witnesses may have misunderstood, but the problem lies in knowing whether the object of those ingenuous accounts is as real as the unquestionable sincerity of their narrators. The response has a bearing on rationalism. And this is because if it is affirmative it brings the odious supernatural to hand. Hence efforts are made to naturalize things and look for nervous shocks to explain the cures, and hallucinations to explain the apparitions. (Bonniot 1879, VI)
By the late nineteenth century, the vocabulary had changed. Bonniot (1879, VII) spoke not of superstition but of psychopathology even as he defended the centrality of the miracle in faith:
The war against pilgrimages is a war of factions that must be situated. Lourdes is not an article of our faith. The army of cultured disbelief directs its efforts to another fundamental point for religion. Christian religion is based on miraculous events; they are there at its birth, they accompany it in its progress and its secular existence. To suppress not such and such a miracle, but the miracle in history is to suppress religion, which cannot exist without the miracle. Physicians accept the historical reality of the miracle, but they separate from it the supernatural elements, the most sacred, the worthiest of respect, which they convert into disorders of the mind; there is no revelation without hallucination or neurosis. Even the most moderate embrace this blasphemy: their respect for religion is no more than politesse.
In a secularized society, the Church had no choice but to accept positivism and the systematic use of ethnographic and clinical enquiry. For centuries, missionaries accumulated vast ethnographic and clinical archives documenting états seconds, trances, nervous attacks, and delirium from every corner of the world. This reordering of the conception of superstition did not solve the problem of the meaning of popular practices and beliefs in relation to the prevention, care, and cure of diseases. Indeed, this problem re-emerged when the European states deployed new health policies and sent legions of rural physicians into the field to confront it. The interaction of these practitioners with the local communities they served was based on a practice whose objective was to eradicate local ‘superstitious’ practices. However:
investigating certain ridiculous or absurd popular remedies one seems to find at the bottom a truth that leaves one astounded… . Does this mean that all popular medicine is a miracle of wisdom? Far from it, but physicians would be well advised to study it deeply and with a certain respect, because when you least expect it, it will jump up and bite you. And this happens more often than you might imagine. (Rubio y Galí cited in Black [1889] 1982, 315–16)
Rubio y Galí, a physician in Seville, wrote this in a letter to his friend the folklorist Machado y Álvarez in response to his request for information on popular health practices to complete the Spanish translation of Black’s (1883) book Folk-Medicine: A Chapter in the History of Culture. Popular wisdom intuitively shapes a space of knowledge that requires specific attention because it falls outside the notion of ‘superstition’ conceived either as a swindle by the rationalists or as ‘vain observance’ by the theologians. At the end of the nineteenth century, Rodríguez López and Rubio y Galí looked to popular medicine to retrieve practices that tied in with their own.
The birth of popular medicine
Many u ponder a la trarseenfermedad encuentra una dicina popular y especiginalese se han ss inasarmchair anthropologists were physicians. They were interested in superstitions in their religious context, but rarely studied folk medicine.[note 17] The first attempt to do so was the British lawyer George W. Black’s Folk-Medicine.[note 18] ‘Folk medicine’, as Black (1883, i) defined it, ‘comprehends charms, incantations, and traditional habits and customs related to the preservation of health and cure of disease, practiced now or formerly at home and abroad’. For Black, folk medicine was an interesting object of study for debating theoretical questions in anthropology. Starting from his observation of the syncretism of medical practice in rural Scotland, he used the notion of ‘survivals’ to explore the mentality of Scottish peasants who held fast to the old practices. As a secondary aim he attempted to test Spencer’s hypothesis on the primitive psyche, investigate the oneiric or epileptic origin of illnesses, and study popular conceptions of the aetiology of illnesses grounded in magic, religion, and natural thought. But he was sceptical about the specificity of folk medicine as an area for research: ‘A separate theory of Folk-Medicine is impossible, for Folk-Medicine has been built up out of very strange and varied materials; but it is perhaps not altogether vain to hope that illustrations of man’s intellectual history will be found by study of collections of classified facts, and the investigation of spells and amulets, of superstitions and witcheries, may not be unworthy of systematic analysis’ (Black 1883, 220).
Black was not a physician, unlike Mantegazza (1892, XIII), one of the most prominent figures in Italian anthropology, who wrote:
Of all the superstitions that exist, medical superstitions are the most interesting ones to study, not only because of their great importance in the health and customs of a people, but also because a psychological analysis of them is among the things that are the most curious and rich in meaning… . A medical superstition is a marvelous confection composed of all the ingredients of psychic cuisine… . I have said that popular medicine is the patrimony of ignorance and fear that children inherit from their parents which, linked to the whims of fashion, fantasy and the mysteries of charlatanism, is transmitted from generation to generation as one of the most sacred legacies.[note 19]
His account has the kind of interpretive density and attention to the native’s point of view that we currently associate with ethnography:[note 20]
Once, when I was calling on a woman who was a patient of mine in Nogoya del Entrerios [Argentina], I was asked if I had a remedy for the evil eye. I modestly replied that, as a doctor, I had to know how to treat all sorts of diseases. As I was speaking I looked hard at her face and saw that she had the brightest eyes that I had ever seen and realized why she had asked me such a strange question. The patient did not hesitate to tell me how, one day, somebody had put a curse on her and that ever since she had been producing beetles, spiders and locks of hair from her genitals. At first I thought it was a joke of dubious taste; but a few days later, while I was studying the disease and the patient, I realized that she innocently believed that insects and hair were coming from her body when, in fact, they were falling into the chamber pot by chance. (Mantegazza 1892, XVI)[note 21]
Mantegazza initially thinks that the woman is putting him on; it is only with the passage of time and careful observation that he comes to understand her. In the context of a clinical encounter that favours enquiry, his commitment to his patient allows him to make sense of her distress. He identified three dimensions in ‘superstition’: a ‘human’ dimension that refers to psychobiology, an ‘ethnic’ dimension related to nature and race, and a ‘scholastic’ or ‘doctrinarian’ dimension related to the penetration of modern clinics and medicine into Italian rural society.
Each medical school, each new prophet of pathology, does not restrict his influence to within the walls of the university or the hospital; its propagation and diffusion ends in the hands of the ignorant who, far away from the seminars, the clinics or the libraries, listen to them with relish and zealously glean each word, however incomprehensible, and then reconstruct them and adapt them to their ignorance and to their level of intelligence… . It is thus that after so many centuries our commoners still have medical superstitions, that can be found in the pages of Averroes and Avicenna. Every day we hear the words ‘inflammation’, ‘crisis’ and ‘temperament’ woven into whatever awkward and absurd expression. Who knows how many superstitions will emerge among the common people from the doctrine of microbes; and when it is adopted and modified by the work of scientific destruction the bacilli will act in a fantastical or magical manner in the minds of the ignorant classes. (Mantegazza 1892, XIII)
As an anarchist, Mantegazza had no interest in the religious aspects of superstition. Instead, his perspective on these beliefs and practices was medical: the positivist gaze of the general practitioner. During the period in which he worked, the end of the nineteenth century, folk medical practices – characterized by some authors as superstitious – were being written about in all sorts of popularizing publications offering practical help to their readers. At the same time, however, physicians and folklorists were also taking an interest in them, publishing them in collections of curiosities (Bartoli and Falteri 1987, 168). u ponder a la trarseenfermedad encuentra una dicina popular y especiginalese se han ss inas
La medicina delle nostre donne, published in 1892 by the Italian rural physician Zanetti,[note 22] should be seen as one of the first intensive case studies of popular medicine in Europe.
And having been a doctor in rural areas, on returning to practice in the city, wherever I went I quietly collected my material and kept it for better times. I had the idea of choosing from among my rather opulent treasure everything referring to the medicine practiced by the people, and ordering it to make a historical and comparative study of the superstitions of our women, whether they be ignorant or educated… . I decided on this for the simple reason that it is women, more conservative than men, who hang on to the old theories and take longer to rid themselves of false beliefs and prejudices and also because it is women who in one way or another always try to find a way of relieving the suffering of others. (Zanetti [1892] 1978, V)[note 23]
In Zanetti’s ([1892] 1978, 3–4) book we can observe the transition away from the old concept of ‘superstition’ and toward the new concept of ‘folk medicine’: ‘Both a prescription from the most illustrious clinician and a remedy suggested by the most naïve of the common women will be accepted in the same way, but on most occasions, the latter will be blindly preferred to the former. But where do our women get their knowledge from and what is the science of their secrets, their remedies and their so-called witchcraft?’ (Zanetti [1892] 1978, 3–4)[note 24]
Zanetti also tried to explain the syncretism he found between folk beliefs and scholastic medicine:
Among the people … because of their lack of intellectual development, there are few if any who know science; they hold onto positive notions, but they do not create them. For this reason their medical knowledge is not something they have invented; with luck they merely remember it. The precepts they pass on to others are things they have heard from the mouth of a man trained in the art [translator’s note: a doctor], who knows how long ago and originating in who knows what scientific theory. They prescribe things that may be attributable to Greek or Arab medicine, or to the Salerno school, or perhaps to later ones. But simply because something resonates unconsciously in their memory, they propound it, they advise it, they defend it. Nevertheless, when modern science reaches them, it may well be … that new theories will make our women forget the old. (Zanetti [1892] 1978, 5)[note 25]
Zanetti was a physician as well as a folklorist, and this set him apart from Pitrè, who was both a physician and a professional folklorist. However, Zanetti was very sensitive in his approach to the women who practiced popular medicine, for the reason that ‘disease will always be a terrible, unknown quantity for the patient, and the instinct of self-preservation will mean that, unthinkingly, any help will be gratefully welcomed, wherever it might come from, in the struggle against the mysterious force of evil’ (Zanetti 1978, 3).[note 26] He carefully refrained from discrediting them as other authors did, considering that in the great majority of cases they were senza ombra de ciurmeria (without any taint of quackery) because they acted from a need to help others and to provide loving care that was intimately associated with their femininity. Although it might be tempting to see their knowledge as irrational and superstitious, he believed that his close examination of the popular tradition showed the opposite (Zanetti [1892] 1978, 4).
Zanetti observed how available resources were mobilized in moments of crisis, independently of logical considerations, attentive to how contradictions emerged in practice, how people decided which treatments to use, and the complex relationships between physicians, folk healers and witches:
Once the real doctor has left, if the impression he has made on the judgment of the male or female healer is good, if his words have had a certain assonance with the erroneous technical terms picked up here and there by the aspiring consultant, if the advice given has some sort of relationship with other superstitious practices, if the prescribed potion is made up of well-known herbs, then the moral support of the mysterious individual is assured. But if the doctor has used language that was not appropriate for the intelligence of the person before him, if he has advised the use of well-known medicines or if he has gone against a silly treatment which has already been initiated, he can be sure that the patient will not be treated according to his prescriptions, but according to those of the so-called male or female healer. (Zanetti [1892] 1978, 12)[note 27]
We can find similar accounts in the writings of other nineteenth-century physicians (De Nino 1891). The precision and systematic nature of their observations contribute to our knowledge of forms of medical practice that, while not hegemonic, were still heavily in demand.
Those who are ignorant of the nature of the diseases that they begin to treat advance blindly, and begin by making a decoction or an infusion of three, five, seven or more herbs, always an odd number, the individual action of which is known to be effective in several diseases, although they do not know if the patient is suffering from these; and after making various signs of the cross over the potion and muttering a few Hail Marys or Our Fathers, they make the patient swallow it down. If the result is negative, they increase the number of completely different herbs to nineteen or thirty-five. (Zanetti [1892] 1978, 13)[note 28]
Zanetti was aware that this could also be applied to his medical colleagues’ prescriptions and to the pharmacists’ commercial strategies. But he did not accept the role played by the experience of the physician, the medicone (healer), and the mammanna (midwife) in shaping positive knowledge of how to treat illness, since this would lead to questioning medical practice. Bartoli and Falteri (1987, 175) suggest that Zanetti obtained his data through conversations with women in the context of a consultation but he never spoke of what he did himself as a doctor. There is no description of his own practice.
Zanetti’s book expresses the intellectual tension between his status as a physician and as a folklorist.[note 29] As a folklorist, he used the local nosology of Umbrian peasants to structure his text from an emic perspective (Falteri 1989, 160), distancing himself from the etic perspective of positivist folklore in his descriptions of the conceptions of the body and anatomy using local categories. His first-person narrative adds weight to the reliability, vividness, and veracity of his text, but sets him apart from a medical narrative that at that time sought to remove any trace of personal commitment or subjectivity. As a general practitioner, Zanetti struggled with the difficulties that physicians had in accepting that the ethnographic gaze was not limited to folklore studies or to anthropology but was also an integral part of medicine (Comelles 1995). The limited circulation of his work reduced it to the status of a local curiosity that has only recently been rediscovered and appreciated.
The credit for establishing ‘popular medicine’ as a specific field of research in medicine, and secondarily in anthropology, should go to Pitrè’s (1896) Medicina popolare siciliana,[note 30] whose aim was to show:
The ethnic and demo-psychological [folkloric] importance of popular medical traditions is unquestionable; but at the same time we must remember its importance for the history of therapeutics: that part of the remedies that retains and that may be of a scientific nature… . Popular beliefs and practices should not be despised only because they come from uncultured people. Their empiricism sometimes has a happy outcome when scientific medicine at times fails… . And how many times, renouncing rational means have we had to observe the marvelous effect of certain old wives’ remedies that were not noted in any therapeutic treatise. (Pitrè 1896, XXIII–XXV)
The book circulated widely throughout Europe and became a reference point for further studies[note 31] because Pitrè developed a specific methodology for describing and classifying folk medicine.[note 32]
There have been few collectors of medical folklore in Italy, and they have limited themselves to collecting common remedies for some common illnesses. Therapeutics has always been preferred and within it, Materia Medica [pharmacology]. But it occurred to no one that therapeutics is part of the pathology, as pathology is part of Medicine. The remedy contends against the illness, which contends against health, which represents the normal state and physiological condition. (Pitrè 1896, VIII)
Following scientific nosography, he applied this method to the description of Sicilian ‘folk illnesses’:
If there is a genre that requires a specialist researcher, it is the field of medicine. Any moderately well-educated person may study mythology, traditional dress… . But it would be difficult, in my opinion, to study medical practices and beliefs if one is not a physician. The reason is that in the field of medicine it is hard for non-doctors to distinguish what is considered error from what is science, the practices of today from those of times past, what once was and what is now superstition. This is why there is confusion in the medical texts of non-physicians between scientific remedies treated as old wives’ tales, and frivolous remedies taken for things that have come directly from the scientific laboratory. (Pitrè 1896, VII)
Above all, he wrote, ‘without an orderly system of classification we cannot conceive of productive data collection by the folklorist. The same applies to doctors, who – and all are aware of it – cannot regard with disdain what they find in humble families, the fruit of their experience, even though it is full of error’(Pitrè 1896, IX).[note 33] However, classificatory rigor was no simple matter because there was disagreement among doctors regarding the principle on which classification should be based:
One controversial point is how to classify illnesses. There are two procedures: one by regions of the body, the other by the nature of the illness. Both are currently full of defects. The first poses problems in illnesses of which we do not know the pathogenesis; pathogenetic theory has brought disorder to topographical pathology. As for the second, recent discoveries place the classifications in doubt. If this is valid for scientists it is no less so for the common people. (Pitrè 1896, XII)
Pitrè placed great value on his years of experience as a general practitioner, which allowed him privileged entry into the homes, lives, experiences, and even thoughts of rural people:
For this reason, I believe that my thirty years of medical practice have served a purpose and have placed me in the advantageous situation of knowing what the common man thinks, what he does when affected by illness and what should be considered a recent importation into the formless mass of events that make up the families’ medical heritage… . My first notes date back to 1870, and not a day has passed without my collecting some data, opinion, remedy, etc. (Pitrè 1896, VIII)[note 34]
Like Black, Mantegazza, Zanetti, and Rodríguez López, Pitrè (1896, XXII) was aware that folk medicine was a ‘survival’ in the growing hegemony of biomedicine, ‘a whole composed of curious and diverse facts, which in their totality appear as an aberration of the human spirit, and in particular are relics of civilization and of disappeared peoples’. As a professional folklorist he was deeply attentive to the local language and its power to evoke experience:
I always give the Sicilian dialect name or the special name from the islands for pathological or physiological events. I illustrate them with words, proverbs, formulas and whatever else might shed light on the thoughts of the people in relation to these events. Nothing is superfluous and nothing is neglected. Even a meaningless phrase is a living document of a practice. The phrase itself is the memory itself, a relic of a physical and moral life from which it was born and of which it was part. These are apparently modest phrases, sometimes too modest, but how many of them can give rise to moments of hope or might reflect life’s passions? (Pitrè, 1896, XIII–XIV)
These writers were ethnographers and not anthropologists, who were then more inclined to producing theoretical syntheses based on data collected by others. Because the ethnographic experience of rural physicians was constructed on the basis of clinical encounters inside the homes of their patients, it may be appropriate to describe Pitrè’s methodology as ‘clinical ethnography’.
Pitre’s book begins with a description of the local specialists: the ciurmadore (a sacred healer), the physician-surgeon, the dealer in secrets, the barber, the conciaossi. The second part consists of local categories of the body and anatomy, moral criteria, special signs and symptoms, physiology, and hygiene. The third part is devoted to his observations of nature and the causes of folk illnesses, procedures for learning about them, and how to judge their duration, prognosis, and the likelihood of curing them. In the final section he describes the most important illnesses, supernatural or spontaneous, induced or acquired (Pitrè 1896, X).
The suitability of some categories will seem to be debatable both to physicians and non-physicians: the former will keep up appearances by claiming to find scientific doctrines treated in a more modest way, while the latter will imagine that the language and scientific rigor are so lofty as to be beyond their grasp. But all this material cannot remain in disarray, and for it to be classified the criteria of the treatise writers cannot be disregarded… . The problem is that it is often impossible to distinguish, in the terms of a simple housewife, anatomy from physiology and physiognomy; nor is it possible to distinguish the boundaries of one from those of the other. What to us are the most nonsensical things are strangely proximate to the common man and to our eyes form an obscure, unrecognizable mass. Hence, how to compare the prognoses, the omens, the prophecies and the judgments… . These classifications do not exist in nature. We make them ourselves’. (Pitrè 1896, XI)
The limits of clinical ethnography
Zanetti and Pitrè created a new ethnographic genre, one I call ‘clinical ethnography’, based on observations in the homes of their patients. This allows me to distinguish it from conventional folklore studies of beliefs and superstitions that included information about health, illness, and care, or from the books of medical popularization. I call it ‘clinical ethnography’ because it is grounded in a methodology, a technique of observation and a narrative based on medical nosography in a very specific setting. Pitrè created this genre in a major theoretical and methodological departure from the historico-cultural schemas used by the folklorists of his time, situating it within the frame of clinical and experimental medicine. It is for this reason that the term ‘medical folklore’, even though it is the standard label of choice for classifying studies of folklore related to health and illness, would be an inappropriate way to describe his work, whose meaning is in and for medicine.
This distancing of ‘clinical ethnography’ from ‘medical folklore’ explains why in Europe, where Pitrè is considered a major figure in the history of medicine, his Medicina popolare siciliana is considered to be just one more regional monograph, and its theoretical, epistemological, and methodological contributions largely ignored. In their histories of folklore, Guichot (1922) and Amades (1980)[note 35] summarize and explain the most widely used schemes for the classification of folklore data. In these, folk medicine is not a specific field, but is either subsumed under superstitions and magical beliefs or found scattered through several different categories. A century after they were first published, neither Zanetti’s nor Pitrè’s books have been reprinted, and the scarce attention paid to them by anthropologists until after World War II shows that they are ambiguously situated on the borders of both folklore and medicine. For folklorists who are not doctors, the methodological link between popular medicine and the medical gaze leaves them feeling incompetent: ‘in view of the different conditions in which that masterpiece [Pitrè’s book] and this feeble monograph … are conceived, how could I justify the present weak, malnourished article and shield it from criticism? My medical knowledge is completely non-existent’ (Pérez Vidal [1945] 2007, 30–31).
The Catalan folklorist Joan Amades (1980, 930) worried about the possible effect of publishing his book on Catalan popular medicine: ‘the present chapter is of a scientific nature and we believe it is unlikely to end up in the hands of simple people who might make use of the practices contained within it; but nonetheless we hesitate to include the formulas that, if used, can cause real harm’.
Pitrè’s influence was felt mainly among the physician-folklorists. In Spain, Lis Quibén, Castillo de Lucas, Erkoreka, and a few others (Pujadas, Comelles, and Prat 1980) used his work, often without direct reference to him, and remained faithful to Tylorian evolutionism. The Galician folklorist Fermín Bouza Brey, in his prologue to the physician Victor Lis Quibén’s book La medicina popular en Galicia, stated that ‘superstition is a ridiculous, fanatical science about religious matters and about the different procedures that the common people use to cure their illnesses’ (Lis Quibén 1949, 15), ideas that chime with those of Amades on folk medicine: ‘the science that concerns itself with collecting and studying popular tradition and with investigating and cataloguing the knowledge of the people and establishing the culture of the ignorant, the illiterate and those who have only a basic education’ (Amades [1969] 1980, 1263). At the end of the twentieth century, at a time when medical anthropology as a specialized field of study was fully developed, the Basque physician and historian Erkoreka (1985, 36) wrote:
other remedies and concepts come from scientific medicine that, once they cease to be accepted with the introduction of new ideas and techniques, are gradually set aside and abandoned, in some cases remaining in popular medicine as silent witnesses to the historical evolution of medicine. In this vein, in the same way as the archaeologist arranges the remains excavated from a site according to strata, assigning a particular age to each one of them, so with some medical practices, fossilized and conserved by the people, can we also order them and assign them an exact age that allows us to place them in a specific moment in the history of medicine.
This persistence of Tylorism in the work of Mantegazza and Erkoreka explains why the notion of ‘survivals’ was still helping to legitimize biomedicine in the late twentieth century to the discredit of popular practices.
The critique of nineteenth-century social and cultural evolutionism by twentieth-century professional anthropology explains why anthropologists did not take up Pitrè’s methodology. The divergence of these two paths has been examined elsewhere (Comelles and Martínez Hernáez 1993). Professional anthropologists were not interested in the applied dimension of clinical ethnography, and even less so in its relationship to European folklore, which situated it far from their academic and professional interests.
For twentieth-century European medicine, clinical ethnography as a qualitative research methodology was residual and marginal, useful only for describing and classifying the folk medical traditions of the subaltern peasant classes in southern Europe and Latin America (Comelles 1995), and gradually fewer and fewer of these documents were produced. Medicine marginalized ethnographic descriptions and replaced them with more politically sanitized instruments such as health statistics and epidemiology. Both techniques divorce the causes of illness from their historical context, reducing them to individual idiosyncrasy based on concepts of hereditary degeneracy or ‘contagionism’ (Comelles 1995a, 1996b).
Medicine rejected ethnography because of its capacity to produce vivid accounts of reality, to present naturalistic descriptions that readers can identify with in the same way that the novels of Charles Dickens awakened readers to the misery and poverty present in nineteenth-century society. The social and political commitment of the authors of such accounts was uncomfortable for a profession that had become not only socially respectable but also socially powerful.
For Pitrè and Zanetti, their dual identities as folklorists and clinical ethnographers were complementary. Folklore and clinical ethnography formed part of the same genre of positivist ethnography although they had different aims. Folklore was a discourse on identity and cultural history, while clinical ethnography sought to establish the cultural limits of medical practice. However, using the clinical relationship in order to observe led to the development of relations of profound trust and respect with those observed after long periods in the field, and required a high level of participation on the ethnographer’s part in local moral worlds. The subjectivity resulting from such shared experience in the clinical relation was shot through with contradictions derived from friendship with and mutual respect for those who could not simply be dismissed as ignorant, and this, at a time when the contemporary medical model was becoming established, was and remains an anomaly. As the therapeutic efficacy of medicine increased, folk medicine lost its value and ceased to be regarded as efficacious. Observation was reduced to the collection of signs and symptoms, without regard for the domestic drama surrounding the ill person and in the absence of a personal commitment to the sick: ‘Gathering any data that came into my hands related to this question and enunciated from it, maintaining the purity with which they were gathered, avoiding their mystification and generally distancing myself from criticism and censure of superstitions, in the understanding that this is, in the first instance, the responsibility of the Church, even when Church and Medicine always work together in harmony to combat them’ (Lis Quibén 1949, XIII).
The resulting text has as its only purpose to record data, occasionally also to condemn failures such as those related to the role of the Church. Lis Quibén was not only a conservative but a Francoist writing down observations made before the Spanish Civil War, and for this reason he implies that the Church shares with medicine an obligation to root out error. After the war, he was unable to comprehend a medicalization already perceptible even in the most isolated populations.
Above all, clinical ethnography produced local patterns of culture characteristic of places like Sicily and Galicia that are the inverse of the ‘universal’ scientific pattern represented by biomedicine: particularism was contrasted with universalism, collectivism with individualism, culture with nature and biology, magic and superstition with science, altruism with mercantilism, and finally, inefficacy with efficacy. For this reason, clinical ethnography persistently ignored the degree of medicalization present among the rural populations it described. It focused on the differences separating rural areas from the metropole, not on what they shared. Nevertheless, the double identity of clinical ethnographers was not without effect on the way they practiced medicine. Their professional commitment to their patients in combination with their commitment to ethnography took the form of a willingness to transform local patterns of health, disease and access to medical care.
As the process of medicalization advanced in rural Europe, however, clinical ethnography declined in importance, becoming a pursuit limited to doctors motivated by enough curiosity and interest to continue patiently recording their observations event by event, day by day, and to bring these observations together into orderly accounts, though more in the spirit of archaeology than as a practical exercise. Once universal compulsory education had enlightened the benighted rural world and a national health care system gave them access to biomedicine, what sense was there in clinical ethnography? What need was there for ethnographers?
References
Ackerknecht, Erwin H. 1985. Medicina y antropologia social: Estudios varios. Madrid: Akal. Originally published as Medicine and Ethnology: Selected Essays (Stuttgart: Hans Huber), 1971.
Amades, Joan. (1969) 1980. Folklore de Catalunya, vol. 3. Barcelona: Editorial Selecta.
Aquino, Santo Tomás de. 1955. Suma teológica, tomo IX. Madrid: Biblioteca de Autores Cristianos.
Bacon, Francis. 1909. Essays, Civil and Moral. New York: Collier & Son. Available online through Harvard Classics at http://www.bartleby.com/3/1/.
Balaguer, Emilio, Rosa Ballester, Josep Bernabeu, and Enrique Perdiguero. 1990. ‘La utilización de fuentes antropológicas en la historiografía médica española contemporánea’. Dynamis 10: 193–208.
Balaguer, Emilio, Rosa Ballester, Josep Bernabeu, and Enrique Perdiguero. 1991. ‘Fuentes históricas de la antropología médica en España’. In Actas del lX Congreso Nacional de Historia de la Medicina, vol. 1, edited by Francesc Bujosa Homar, Consuelo Miqueo, Asunción Fernández-Doctor, and Àlvar Martínez Vidal, 107–15. Zaragoza: Ayuntamiento de Zaragoza.
Barreiro, Bernardo. (1883) 1973. Brujos y Astrólogos de la Inquisición de Galicia y el Famoso Libro de San Cipriano. Madrid: Akal.
Bartoli, Paolo. 1985. ‘Farmaci e sacramenti. Organizzazione sanitaria e parroci di campagna nella seconda mettà dell’Ottocento’. Sanità, Scienza e Storia 2: 121–40.
Bartoli, Paolo, and Paola Falteri. 1987. ‘La medicina popolare in Umbria dalla fine dell’800 ad oggi: Permanenze e transformazioni’. In Sanità e Società. Emilia-Romagna, Toscana, Marche, Umbria, Lazio Secoli XVI–XX, edited by Alessandro Pastore and Paolo Sorcinelli, 167–208. Udine: Casamassima.
Bartoli, Paolo, and Paola Falteri. 1989. ‘La medicina popolare e la costruzione del sistema sanitario pubblico nello stato unitario italiano’. In Le Tradizioni popolari in Italia: Medicine e Magie, edited by Tullio Seppilli, 22–30. Perugia: Electa.
Black, William G. 1883. Folk-Medicine: A Chapter in the History of Culture. London: Eliot Stock for the Folk-lore Society.
Black, William G. 1982. Medicina popular: Un capítulo en la historia de la cultura. Translated by Antonio Machado y Alvarez, with addenda by Emilio Olabarría and Federico Rubio y Gali. Barcelona: Altafulla. Facsimile from the 1889 edition.
Bonniot, Joseph de. 1879. Le miracle et les sciences médicales: Hallucinations, apparitions, extase, fausse extase. Paris: Didier.
Boorde, Andrew. (1547) 2010. The Breuiary of Healthe, for All Maner of Sicknesses and Diseases the Which May Be in Man Or Woman, Doth Followe Expressyng the Obscure Termes of Greke, Araby, Latyn, and Barbary, in Englishe. London: Thomas Este.
Bourke, John G. 1892. Apache Medicine-Men. New York: Dover Publications.
Bronzini, Giovanni B. 1983. ‘Antropologia e medicina popolare. Note sugli studi dei positivisti italiani’. La Ricerca Folklorica 8: 13–17. http://dx.doi.org/10.2307/1479530.
Brown, Peter. 1981. The Cult of the Saints: Its Rise and Function in Latin Christianity. Chicago: University of Chicago Press.
Buchan, Jorge. 1785. Medicina doméstica ó tratado completo del método de precaver y curar las enfermedades. Madrid: Imprenta de D. Antonio de Sancha. Originally published as Domestic medicine (Balfour, Auld and Smellie: Edinburgh), 1769.
Caro Baroja, Julio. 1967. Vidas mágicas e Inquisición,2 vols. Madrid: Ediciones Taurus.
Castillo de Lucas, Antonio. 1958. Folkmedicina: medicina popular, folklore médico, etnomedicina, demoiatria etnoiátrica. Barcelona: Dossat.
Cirese, Alberto M. 1978. ‘Zanetti e la medicina popolare: Questioni di ieri e di oggi’. In La Medicina delle nostre donne: Studio folk-lorico, con una lettera di Paolo Mantegazza, con un saggio di Alberto Cirese, edited by Zeno Zanetti and Maria R. Trabalza, 11–35. Foligno: Ediclio.
Ciruelo, Pedro. 1561. Reprobación de las supersticiones y hechicerías. Libro muy útil para los buenos cristianos. Medina del Campo: En casa de Guillermo de Millis.
Comelles, Josep M. 1993. ‘Milagros, santos, vírgenes y medicos: La institucionalización del milagro en la Europa cristiana’. In Antropologia de la salud y de la medicina, edited by Oriol Romani and Josep M. Comelles, 166–92. La Laguna: VI Congreso de Antropología FAAEE/ACA.
Comelles, Josep M. 1994. ‘El papel del sistema de salud en la configuración de la demanda de servicios’. In El usuario como determinante de la oferta de servicios sanitarios, 29–41. Madrid: Comunidad de Madrid.
Comelles, Josep M. 1995a. ‘Antropologia, psiquiatria i medicina: de les topografies mèdiques al constructivisme’. L’Avenç. Revista d’Història 195: 46–50.
Comelles, Josep M. 1995b. ‘Miracles, supersticions i remeis: Els límits culturals de la pràctica mèdica i religiosa’. Revista d’Etnologia de Catalunya 6: 48–57.
Comelles, Josep M. 1996a. ‘Da superstizione a medicina popolare. La transizione da un concetto religioso a un concetto medico’. AM Rivista della Società Italiana di Antropologia Mèdica 1–2: 57–87.
Comelles, Josep M. 1996b. ‘De la práctica etnográfica a la práctica clínica en la construcción del estado contemporáneo en España’. In De la construcción de la historia a la práctica de la antropología en España, edited by Encarnación Aguilar-Criado, 133–51. Zaragoza: IAA-FAAEE.
Comelles, Josep M. 1996c. ‘Fe, carismas y milagros. El poder de curar y la sacralización de la práctica médica contemporánea’. In Creer y curar. La medicina popular, edited by Jose A. González Alcantud and Salvador Rodriguez Becerra, 301–36. Granada: Diputación Provincial.
Comelles, Josep M. 1997. ‘De las supersticiones a la medicina popular. La transición de un concepto médico a un concepto religioso’. In Medicina popular e antropoloxia da saude, edited by Xose M. González Reboredo, 247–80. Santiago de Compostela: Consello da Cultura Galega.
Comelles, Josep M. 1998. ‘From Ethnography to Clinical Practice in the Construction of the Contemporary State’. In Democracy and Ethnography: Constructing Identities in Multicultural Liberal States, edited by Carol J. Greenhouse, 233–53. Albany: State University of New York Press.
Comelles, Josep M., and Angel Martínez-Hernáez. 1993. Enfermedad, cultura y sociedad: Un ensayo sobre las relaciones entre la antropología social y la medicina. Madrid: EUDEMA.
Coronedi Berti, C. 1877. ‘Appunti di medicina popolare Bolognese’. Rivista di Letteratura Popolare 1: 12.
De Nino, Antonio. 1891. Usi et costumi abruzzesi descriti da A. de Niro Volume Quinto: Malattie e rimedi. Florence: Tipografia di G. Barbera.
Delumeau, Jean. 1989. Rassurer et Protéger. Paris: Fayard.
Delumeau, Jean. 1992. La confesión y el perdón: Las dificultades de la confesión, siglos XIII a XVIII. Madrid: Alianza. Originally published as L’Aveu et le pardon Les difficultés de la confession (XIIIe-XVIIIe siècle) (Paris: Fayard), 1990.
Erkoreka, Anton. 1985. Análisis de la medicina popular vasca. Bilbao: Instituto Labayru-Etniker.
Feijóo, Fray Benito. 1757. Theatro critico universal, o discursos varios en todo género de materias, para desengaño de errores comunes. Tomo segundo. Madrid: En la oficina de Domingo Fernández de Arrojo.
Fissell, Mary. 1992. ‘Readers, Texts and Contexts: Vernacular Medical Works in Early Modern England’. In The Popularization of Medicine 1650–1850, edited by Roy Porter, 72–96. London and New York: Routledge.
Gaume, El Abate J. 1864. Manual de los confesores. Barcelona: Imprenta de Pablo Riera. Originally published as Manuel des confesseurs (Paris: Gaume Frères- Libraires Editeurs), 1842.
Good, Byron. 1994. Medicine, rationality and experience. Cambridge University Press.
Gross, Samuel D. 1875. The Glory and the Hardships of the Medical Life; Being the Valedictory Address Delivered at the Philadelphia Academy of Music, March 11, 1875, before the Trustees, Faculty, and Students of the Jefferson Medical Collegem at its Forty-Ninth Annual Commencement. Philadelphia: P. Madeira, Surgical Instrument Maker.
Guichot y Sierra, Alejandro. (1922) 1984. Noticia Histórica Del Folklore. Facsimile of first edition. Sevilla: Junta de Andalucía, Consejería de cultura.
Hoffman, Walter James. 1889. ‘Folk-Medicine of the Pennsylvania Germans’. Proceedings of the American Philosophical Society 26: 329–52. http://www.jstor.org/stable/982955.
Höfler, M. 1893. Volksmedizin und Aberglaube in Oberbayerns Gegenwart und Vergangenheit.Munich: Neue Ausgabe.
Lis Quibén, V. 1949. La medicina popular en Galicia. Pontevedra: Gráficas Torres.
Mantegazza, Paolo. 1870. Rio de la Plata e Tenerife, viaggi e studi. Milan: Gaetano Brigola, Editore.
Mantegazza, Paolo. 1892. ‘La psicologia delle superstizioni (Lettera al Dott. Zeno Zanetti)’. In La medicina delle nostre donne, edited by Zeno Zanetti, XI–XIX. Città di Castello: S. Lappi, Tipógrafo e Editore.
Martínez Hernáez, Angel, and Josep M. Comelles. 1994. ‘La medicina popular: ¿Los límites culturales del modelo médico?’ Revista de Dialectología y Tradiciones Populares 49, no. 2: 109–36.
Munaret, Le docteur. 1840. Du médecin des villes et du campagne: moeurs et science. Paris: Germer Baillieres, Libraire Editeur.
Paul, Jacques. 1988. La Iglesia y la cultura en Occidente (Siglos IX–XII),vol. 1, La santificación del orden temporal y espiritual. Barcelona: Editorial Labor. Originally published as L'Eglise et la culture en Occident, IXe-XIIe siècles: L'éveil évangélique et les mentalités religieuses (Paris: P.U.F), 1986.
Pérez Vidal, José. (1945) 2007. Contribución al estudio de la medicina popular canaria. Santa Cruz de Tenerife: Ediciones IDEA.
Pitrè, Giuseppe. 1896. Medicina popolare siciliana. Turin: Carlo Clausen.
Porter, Roy, ed. 1992. The Popularization of Medicine, 1650–1850. London: Routledge.
Prats, Llorenç. 1989. ‘Aportaciones de las topografias médicas al conocimiento etnográfico de los Países Catalanes’. Boletin de Historia de la Antropología 1: 3–6.
Pujadas, Joan J., Josep M. Comelles, and Joan Prat. 1980. ‘Una Bibliografía comentada sobre Antropología Médica’. In La Antropología Médica En España., edited by Michael Kenny and Jesús de Miguel, 323–53. Barcelona: Anagrama.
Río, Martin del. 1611. Les Controverses et Recherches Magiques de .... Divisées en six livres, auquels sont exactement et doctement consultées les sciences curieuses, les vanitez & les superstitions de toute la Magie, avecques la manière de procéder en Justice contre les Magiciens. Paris: Chez Jean Petit-Pas.
Ruizes de Fontecha, Juan-Alonso de los. 1606. Diez previlegios para mugeres preñadas compuestos por el DoctorJuan Alonso de los Ruyeses y Fontecha natural de la Villa de Daymiel, Cathedrático de Vísperas en la Facultad de Medizina de la Universidad de Alcalá. Con un diccionario médico. Alcalá de Henares: Luys Martinez Grande.
Seppilli, Tullio, ed. 1989. Le tradizioni popolari in Italia: Medicine e Magie. Milan: Electa.
Tissot, Samuel Auguste. 1776. Tratado de las enfermedades mas frecuentes de las gentes del campo. Madrid: Imprenta Pedro Marín (4th ed.).
Tylor, Edward B. 1977. Cultura primitiva. Madrid: Ayuso. Originally published in English as Primitive Culture: Researches into the Development of Mythology, Philosophy, Religion, Art, and Custom, in two volumes (London: John Murray), 1871.
Ware, John. 1849. Duties and Qualifications of Physicians: An Introductory Lecture. Oxford: John Henry Parker.
Woodward, Kennett L. 1990. Making Saints: How the Catholic Church Determines Who Becomes a Saint, Who Doesn’t and Why. New York: Simon & Schuster.
Zanetti, Zeno. 1892. La medicina delle nostre donne: Studio folklorico. Città di Castello: S. Lapi Tipografo Editore.
Endnotes
1 Back
The Risorgimento (resurgence) was the nineteenth-century movement to politically unify the Italian states.
2 Back
This article was part of a research project on the history of ethnographic techniques. Documentary research was carried out in the Reial Acadèmia de Medicina de Barcelona, and in the John Blocker Rare Books Collection of the Moody Library in Galveston, Texas. The article builds on previous arguments (Comelles 1995; Comelles and Martínez-Hernáez 1993; Martínez-Hernáez and Comelles 1994), and personal suggestions and comments from Enrique Perdiguero-Gil and Eduardo Menédez, but above all it is the result of the discovery of Italian positivist medical folklore through the work of Tullio Seppilli, Paolo Bartoli, and Paola Falteri. The original manuscript of this article in Spanish was first published in Italian translation (Comelles 1996a) by Paolo Bartoli. A Spanish version was published a year later, in Medicina popular e antropoloxia da saude, edited by Xose M. González Reboredo (Comelles 1997). I have revised this last version for the present English translation, done by Mary Savage and Susan DiGiacomo (Universitat Rovira I Virgili), moving or rewriting some paragraphs, adding new ones, deleting others, and correcting errors, punctuation, verb tenses, and any other oversights that might have posed problems in the translation. Where necessary I have added clarification for readers unfamiliar with southern Europe.
3 Back
These publications began to appear after the Renaissance; they contain practical advice, folk remedies, Hippocratic and Galenic medicines, and pharmaceutical preparations, and were written in vernacular languages. They include works such as the Breviary of Health (Boorde 1547), the tesoros de los pobres (treasures of the poor; popularizing books of remedies), and books on ‘domestic medicine’ (Porter 1992). In his history of folklore, Guichot ([1922] 1984) translated all the book titles into Spanish, but most of the material he quoted from them is incompletely referenced.
4 Back
These documents have been largely neglected although some scholars have drawn attention to them (Porter 1992), and to their ethnographic importance; see Balaguer et al. 1990; Balaguer et al. 1991; and Prats 1989. Their circulation in early modern England has been studied by Fissell (1992).
5 Back
The term ‘survival’ was Tylor’s response to the connotations surrounding the term ‘superstition’ (Tylor 1977). An extensive discussion of these two concepts can be found in Cirese 1978, 19.
6 Back
The German Volksmedizin became ‘folk medicine’ in English. In Romance languages it was translated as medicina popular (Spanish), medicina popolare (Italian), and médecine populaire (French).
7 Back
Ackerknecht (1985, 7–8) distinguishes between ‘primitive medicine’, ‘ethnomedicine’, and ‘folk medicine’, preferring ‘ethnomedicine’ to ‘primitive medicine’ as a way to characterize the medical practices of aboriginal societies and limiting ‘folk medicine’ (popular or traditional medicine) to the medical traditions of historical societies, which consisted of a syncretic fusion of primitive medicine, Galenism, and medical technology.
8 Back
I identify as ‘medical folklore’ the texts written by medical doctors.
9 Back
Caro Baroja (1967, I:46) points out his strongly rationalist approach to describing the mechanisms by which superstition and idolatry are produced.
10 Back
Gaume (1864) devotes a chapter of his confessors’ manual to the ‘skill of the physician’ and uses metaphorical language to refer to medical practice. Delumeau (1992, 9–44) proposes a psychological interpretation of confession that can be superimposed on the idea of the physician as pacifier of social tensions.
11 Back
This led to increasingly harsher sentences for Jews and Lutherans tried for superstitious practices (Caro Baroja 1967).
12 Back
Paul (1988, 63–87) describes Charlemagne’s early efforts to supply parish priests with texts that would establish orthodoxy in order to prevent oral transmission giving rise to free interpretations.
13 Back
Onwards as the Church, as Italian and Spanish languages write Church (Chiesa or Iglesia) with a capital letter.
14 Back
It is important to note the distance between parish priests and Church intellectuals such as the Spanish monk Benito Jerónimo Feijóo (1757), one of the leading critics of error and folk superstition during the Spanish Enlightenment.
15 Back
The attitude of the physicians was contradictory. They were quick to denounce quackery (Ciruelo 1561), but many shared the beliefs and practices of folk healers. In his gynaecological treatise, Ruizes de Fontecha (1606), a professor at the University of Alcalá, devoted an entire chapter to techniques for discovering the sex of the foetus, and included the evil eye in a chapter on childhood illnesses.
16 Back
Feijóo (1757) inveighed against the medical ‘errors’ that he attributed to routine, ignorance, and superstition, but at the same time he defended the need for miracles as proof of faith. For a critical analysis of his work, see Caro Baroja (1967, II:305–39).
17 Back
American ethnographers coined the terms ‘medicine man’ and ‘medicine woman’ to describe aboriginal healers. They did not consider medicine to be a specific research topic; see, for example, Bourke 1892.
18 Back
Machado y Álvarez translated the book into Spanish as Medicina popular (Black [1889] 1982). He avoided the term ‘supersticiones médicas’, used by Olabarría in 1885 in a previous paper included in Machado’s translation of Black.
19 Back
‘Le superstizioni mediche sono fra tutte, forse le più interessanti a studiarsi; non solo per la importanza grandissima che hanno sulla salute e sui costumi di un popolo, ma anche perché la loro analisi psicologica e fra le più curiose e feconde. . . . Una superstizione medica e un mirifico pasticcio, en cui entrano tutti quanti gli intringoli della cucina psichica. Io dicevo che la medicina popolare e il patrimonio di ignoranza e paura che i figli ereditano dai padri, e che arricchito dai capricci della moda, dalle bizzarrie della fantasia e dai misteri del ciarlatanismo, si trasmette di generazioni in generazioni come una delle eredità più sacre’.
20 Back
In his foreword to Zanetti’s book, Mantegazza (1870) included ethnographic examples from his travel notes from Río de la Plata and Tenerife published in 1870.
21 Back
‘Una volta, chiamato al letto di una ammalata a Nogoya dell’Entrerios [Argentina], fui interrogato se sapessi curare il mal de occhio; al che risposi modestamente che essendo medico doveva saper trattare qualunque malattia. Io intanto, fissandola in volto, vedevo gli occhi più lucidi del mondo e accettava una spiegazione a quella singolare domanda. L' inferma, non tardo a raccontare come un tale le aveva gettato una mala sorte, e da quel girono in poi, essa emetteva dai genitali, coleotteri, ragni e ciocche di capelli. Mi credetti zimbello di una burla di cattivo gusto; ma dopo pochi giorni, studiando la malattia e la malata, trovai qu' essa ingenuamente credeva, che le uscissero dall' corpo gl' insetti e i capelli che cadevano per caso nel vaso da note’.
22 Back
In 1890 Zanetti sent his manuscript to the Società Italiana di Antropologia, Etnologia e Psicologia to participate in a folklore competition. It was excluded because it was limited to medicine and did not take into account popular beliefs in other domains of life (Cirese 1978, 14). Despite the support of Pitrè and Mantegazza, it would remain forgotten until it was republished in Zanetti 1978, with critical addenda. See also Bartoli and Falteri 1987 and Bartoli 1989.
23 Back
‘e andato in condotta nelle campagne, tornato medico nella mia città dappertutto ho raccolto silenziosamente il mio materiale e serbatolo per tempi migliori. . . . Ebbi in idea di scegliere dal mio tesoro abbastanza opulento, tutto ciò che riguardasse la medicina praticata dal popolo, e ordinarlo a scopo di uno studio storico e comparato delle superstizioni possedute dalle nostre donne ignoranti e colte. . . . Io lo prescelsi per il solo fatto che e la donna, più conservatrice che l’uomo, più tardi di questo che dimentica le antiche teorie, più tardi si spoglia delle false credenze e dei pregiudichi, e inoltri perché è la donna che si studia sempre di recare, in qualche modo, un sollievo a coloro che soffrono’.
24 Back
‘Saranno egualmente accolti, tanto la ricetta del clinico il più illustre, quanto il rimedio consigliato dalla più ingenua femminuccia del volgo, ed anzi, il più delle volte, questo sarà cecamente preferito a quella. Ma d'onde viene alle nostre donne e quale e la scienza dei loro segreti, dei loro rimedi, delle loro cosi dette stregonerie?’
25 Back
‘Il popolo . . . per le sue condizioni di mancato sviluppo intellettuale, non ci apparisce giammai scienziato, giacche in fatto di nozione positive esso conserva, ma non crea. Quindi e che la sua scienza medica esso non può averla inventata, ma ricordata soltanto. I precetti che esso insegna ad altri, deve averli certamente ascoltati dalla bocca di un uomo dell’arte, chi sa in qual epoca e durante il dominio de chi sa quali teorie scientifiche. Egli vi dara prescrizioni che potrebbero attribuirsi alla scuola greca, sia alla scuola araba, sia a quella salernitana, sia alle scuole posteriori: ma è per il solo fatto che quelle risonano inconsciamente nella sua memoria, che esso le detta, le consiglia, le difende; così, quando la scienza moderna sarà più diffusa, possiamo esser certi che anche questa sarà rammentata dal popolo e che le nuove teorie faranno alle nostre femminucce, dimenticare le antiche’.
26 Back
‘Il morbo sarà sempre una incognita spaventosa per il malato, e che l'istinto della propria conservazione farà sempre accogliere senza discuterlo, qualunque aiuto e da qualunque braccio prestato, nella lotta contro la potenza misteriosa del male’.
27 Back
‘Uscito il medico vero, se l’impressione prodotta da questo sul giudice maschio o femmina, fu buona; se le sue parole ebbero una certa assonanza coi termini tecnici errati appresi qua è la dal pretenzioso consulente, se la pratica manuale consigliata avrà una qualche relazione con altre pratiche superstiziose, se la pozione ordinata sia composta di erbe ben note, si è sicuri dell’appoggio morale dell’individuo misterioso. ma se il medico avrà usato un linguaggio poco alla portata della intelligenza che si trovava a lui presente, se avrà consigliato medicine conosciute o si sarà opposto ad una pratica sciocca già iniziata, può essere certo che il suo infermo non sarà trattato secondo le sue prescrizioni, ma secondo quelle del così detto medicone o della medicona’ (Zanetti 1892, 12).
28 Back
‘Ignari della natura dei morbi ch'essi prendono a curare procedono a tentoni, e cominciano dal fare una decozione o un infuso de tre, cinque, sette o più erbe, sempre in numero disparo, di quelle la cui azioni individuale e conosciuta da essi efficace nelle varie malattie delle quali e concerto se il malato sia affetto o no; e dopo aver trinciato sopra alle pozioni parecchi segni di croce e borbottato qualche Ave o qualche Pater, la danno a trangugiare. . . . Se il risultato fu nullo, aumentano il numero delle erbe e lo portano a diciannove, a trenta cinque, di qualità sempre differente’.
29 Back
Like Zanetti, Lis Quibén (1949) in Spain and Pitrè (1896) in Italy were reluctant to write about their own medical practices. Even when physicians did occasionally reveal their practices, these writings were not ethnographic, but took the form of a presentation on the moral and scientific qualities and the duties of the practicing physician (Comelles 1994). Recently the Basque Erkoreka (1985) also referred to this tension.
30 Back
According to Pitrè (1896, 464), Coronedi Berti (1877) also used the term ‘popular medicine’. Zanetti began his research around 1886, and Pitrè gathered his material between the end of the 1870s and his death in 1913.
31 Back
Pitrè was a friend of Lombroso and Mantegazza, and read his British, French, and German colleagues. For more on his influence in Spain, see the writings of physicians Castillo de Lucas (1958), Lis Quibén (1949), and Erkoreka (1985), and folklorists Pérez Vidal ([1945] 2007) and Amades (1980).
32 Back
Pitrè refers to the peasants’ popular practices, never to the urban middle and upper classes, which were considered to be medicalized. He does not speak of the influence of priests, nuns, physicians, or nurses in shaping these practices.
33 Back
‘senza una classificazione ordinata no si saprebbe concepire una raccolta buona per folkloristi non meno que per medici, i quale – nessuno se lo dissimula – non devono dispreziare quel que trovano nelle famiglie popolari, fruto di esperienza per quanto pieno di pregiudizzii’.
34 Back
Pitrè’s strategy could be comparable to that of the North American ethnographers of his time who made up for their lack of training through systematic observation and classification with very long periods in the field.
35 Back
Written in the 1950s, it contains a major study of popular medicine in Catalonia.