Inside/outside
Contours of men’s everyday health care and masculinities in Denmark
—
The notion of a ‘crisis in men’s health’ has been developing in Western societies for the past thirty years. In these settings, men have been shown to be at greater risk than women of developing all major diseases, and to be more likely than women to die from leading causes of death, yet they are reluctant to seek medical advice (European Commission 2011). In Denmark, research has demonstrated the ways in which men ‘distance’ themselves from physical and emotional health needs, and there are ongoing concerns about whether health-promotion messages are reaching men (Christensen et al. 2012; Christensen et al. 2006). These trends are frequently explained with reference to traditional patterns of masculinity in Western societies, which are understood to include engagement in high levels of risk taking, the dismissal of health problems, and a perception that caring for one’s body and health and expressing emotions are feminine (Courtenay 2000). In these settings, the ‘doing’ of masculinity is generally looked upon as the undoing of men’s health. Such explanations may, however, mask more complex and changing pictures of men’s health care and masculinities.
This photo essay draws from a study that sought to make strange the familiar terrain of health care and masculinities in Denmark, allowing other framings to emerge. The participants were fourteen men between thirty-five and sixty-nine years of age, and most were experiencing health problems for which they were receiving ongoing or intermittent biomedical care. Participants were invited to take up to ten photographs of any activity, object, event, or individual that they deemed relevant to their everyday health care practices. The photographs were taken with the men’s smartphones and emailed to me once the task was completed. The images brought into focus particular aspects of men’s everyday lived experiences and health care practices, which served as the starting point for dialogue during subsequent in-depth interviews.
Here, I present Stefan’s (a pseudonym) photographs, with a brief outline of his story. Two months before our first meeting, Stefan, a sixty-nine-year-old gay man living in Copenhagen, had undergone a radical prostatectomy, following a diagnosis of prostate cancer. Unlike the other men who participated in my study, when he emailed me his images Stefan also provided captions for each one. To preserve the original flow of his story, the images with captions are presented in the sequence in which they were sent and later discussed.
Of all the participants, Stefan was perhaps the most enthusiastic about telling his story both visually and verbally. However, all of the images produced by participants reflect the intersubjective nature of men’s everyday health care practices and the demedicalized ways in which they pursued well-being in different spaces with multiple social, symbolic, and relational meanings and significances. Therapeutic landscapes, McLean (2007, 320) suggests, consist of ‘intersubjective relationships between a person’s internal experiential spaces and external physical ones, and a third reciprocal relational space’ (italics in original). Thus, therapeutic landscapes extend beyond the physical features of natural and built environments to their social and symbolic aspects, and to their relational significance for the experiencing subject (Williams 2002; Gesler 2003). The concept of therapeutic landscapes directs our attention to the profoundly relational nature of health care practices, and to the ways in which health care settings are continually produced by changing social and institutional relationships (Williams 2002, 145).
In this study, men’s care practices existed in manifold relations with the spaces they occupied, the objects within these spaces, and the people with whom they engaged in these spaces. This underscores that human experience and consciousness take on material and spatial form in multiple sites, and points to how spaces can be embodied (Low and Lawrence-Zúñiga 2003). Importantly, these care practices also reflect the intertwining of traditional patterns of masculinities with what I term ‘caring masculinities’.
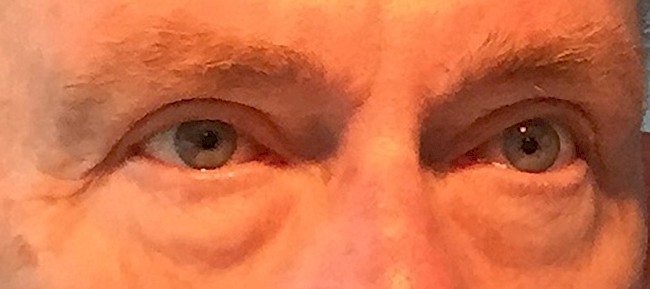
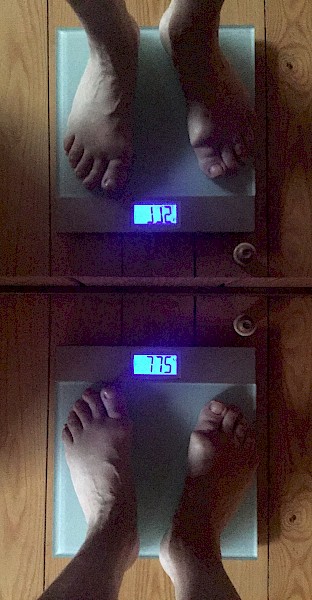
A multitude of health-related activities take place in the privacy of one’s home, often connected with intimate bodily experiences and daily routines. Stefan began his day by looking himself in the eyes (photograph 1), an activity that he described as a ‘tool’ for assessing how to care for himself that day: ‘Should I call the doctor, should I take some vitamins, or should I call some friends, go and see a movie? I do whatever I think would be helpful to ease the day’. This self-assessment was complemented by the daily monitoring of bowel movements and stools (photograph 2). As Stefan put it, his eyes reflect his ‘state of mind’, while his digestion is ‘the mirror of the body’. Stefan also monitored his weight on a daily basis (photograph 3), with written records going back several years. An awareness of his weight, he explained, enables him to adjust his diet if necessary and to attain an aesthetically pleasing and attractive body.
Following the radical prostatectomy Stefan experienced urinary incontinence (photograph 4), which meant that his daily activities had to be organized around intimate bodily contingencies. To manage the rupture between his presurgery and postsurgery body, Stefan acquired new knowledge about his body and unfamiliar technologies (incontinence pads), as well as skills commonly associated with caring for the out-of-control bodies of infants and menstruating women. As he said, ‘I’ve never had a diaper in my hand before. I didn’t know what’s up and down, and then at the age of sixty-nine I have to wear that! It’s a totally new situation and it has changed me’.
Photographs of other routine health-related activities foregrounded Stefan’s social life, including the preparation of healthy, beautiful meals (photograph 5) that could be shared with others. The consumption of alcohol (photograph 6) in tranquil and group settings was understood by Stefan to generate and support relaxation and sociality, which he associated with emotional well-being due to their ‘positive impact on [his] psychological state of mind’.
Stefan articulated a connection between natural environments, health care, and healing. He described his summerhouse by the sea (photograph 7) as a ‘sacred place’ that was imbued with experiences of nurture and memories of an active social life. The yearly flowering of daffodils planted in the garden many years ago by a deceased partner connected him to the loss of loved ones, the currents of ageing, and his own fluctuating physical vulnerabilities. Particularly the immersion in seascapes where ‘time doesn’t matter’ (photograph 8) produced for Stefan a deeply felt sense of timelessness and a healing connection with the universe.
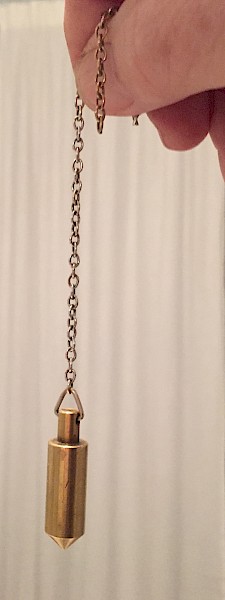
Stefan complemented his biomedical care from the public health care system with alternative approaches offered in the private sector (photograph 9). This resulted sometimes in tensions between different knowledge practices (photograph 10). Despite the frequent association of nonbiomedical therapies with women’s health care (Nissen 2011), Stefan understood his active engagement with a range of health care options as an integral part of caring for himself.
The exploration of Stefan’s visual and verbal narratives of events (Pink 2007) revealed multifaceted health care practices in different spatial contexts that revolved around the body and self, whilst also demonstrating the ongoing production of diverse therapeutic landscapes. Stefan’s embodied care practices were grounded in self-knowledge and self-discipline, and his body’s interior performance was routinely exteriorized and made accessible to personal interpretation, understanding, and action. The ways in which Stefan crafted and made sense of different practices, while enacting, embodying, and resisting biomedical ideals of health care, bodies, and masculinities, point to an intertwining of a ‘caring masculinity’ with practices of autonomy, control, and aesthetic ideas about male bodies. The intersubjective nature of Stefan’s everyday health care practices and the demedicalized pursuit of well-being highlight the many meanings and significances in/of therapeutic sites, and draw attention to the complex interplay between space/place, health care, and gender.
About the author
Nina Nissen, PhD, is Associate Professor at the Department of Public Health, University of Southern Denmark. Her research interests include the diversity and diversification of medical knowledge and therapeutic practices, and the interplay between health care, gender (and other social differences), and personal and social change. Her methodological interests include the creation of synergies between medical and visual anthropologies.
References
Christensen, Anne Illemann, Ola Ekholm, Michael Davisen, and Knud Juel. 2012. Sundhed og Sygelighed i Danmark 2010 - og Udviklingen Siden 1987. Copenhagen: Statens Institut for Folkesundhed, Syddansk Universitet. http://www.si-folkesundhed.dk/upload/susy_2010_til_hjemmeside.pdf
Christensen, Kaare, Christian Graugaard, Hans Bonde, Jørn Wulff Helge, and Svend Aage Madsen. 2006. Kend Din Krop, Mand. Copenhagen: Lindhardt og Ringho.
Courtenay, Will H. 2000. ‘Constructions of Masculinity and Their Influence on Men's Well-being: A Theory of Gender and Health’. Social Science & Medicine 50, no. 10: 1385–1401. https://doi.org/10.1016/s0277-9536(99)00390-1.
European Commission. 2011. The State of Men’s Health in Europe. Brussels: European Commission. http://ec.europa.eu/health//sites/health/files/population_groups/docs/men_health_report_en.pdf.
Gesler, Wilbert. 2003. Healing Places. Lanham, MD: Rowman & Littlefield.
Low, Setha M., and Denise Lawrence-Zúñiga. 2003. The Anthropology of Space and Place: Locating Culture. Blackwell Readers in Anthropology 4. Malden, MA: Blackwell.
McLean, Athena. 2007. ‘The Therapeutic Landscape of Dementia Care: Contours of Intersubjective Spaces for Sustaining the Person’. In Therapeutic Landscapes, edited by Allison Williams, 315–32. Aldershot: Ashgate Publishing Limited.
Nissen, Nina. 2011. ‘Challenging Perspectives: Women, Complementary and Alternative Medicine, and Social Change’. Interface: A Journal for and about Social Movements 3, no. 2: 187–212. http://www.interfacejournal.net/wordpress/wp-content/uploads/2011/12/Interface-3-2-Nissen.pdf.
Pink, Sarah. 2007. Doing Visual Ethnography. 2nd ed. London: Sage.
Williams, Allison. 2002. ‘Changing Geographies of Care: Employing the Concept of Therapeutic Landscapes as a Framework in Examining Home Space’. Social Science & Medicine 55, no. 1: 141–54. https://doi.org/10.1016/S0277-9536(01)00209-X.