‘When language skews narratives’
Critical medical humanitarianism after Beirut, Paris, and Baghdad
—
Abstract
On 12 November 2015, Bourj al-Barajneh – a small, impoverished suburb and former Palestinian refugee camp located in Beirut – was targeted by members of ISIS with a double suicide bombing. The incident claimed the lives of forty-three people and injured more than two hundred (Barnard and Saad 2015). While few media outlets in Europe and the United States provided in-depth coverage of the incident, the events in Paris the very next day, claiming more than 120 lives with multiple bombings throughout the city, brought the attention of the entire world to France, even while Baghdad suffered ISIS-led bombings that same day (Almasy, Meilhan, and Bitterman 2015; Associated Press 2015).[note 1] From expressions of solidarity from celebrities on Twitter to the changing of individual Facebook profile pictures to the French flag, worldwide popular attention drifted towards Europe from the Middle East (Shenton 2015; see figure 1).[note 2] Though the events in Beirut, Paris, and Baghdad all caused significant destruction and loss of life, only Paris captured the interest of major Western media outlets. The disproportionate emphasis on Paris in news coverage implicitly indicates the normalcy of violence in the Middle East; as a result, commentary attempting to balance the perspectives on the ISIS-led bombings focuses on the forgotten nature of the bombings in Beirut and Baghdad (see Barnard 2015).
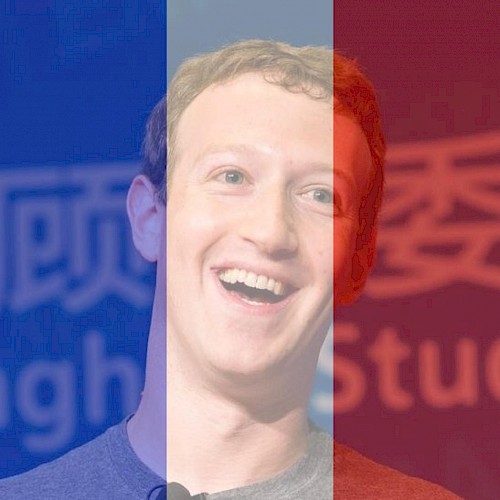 Figure 1. The profile picture of Mark Zuckerberg, founder of Facebook, superimposing the French flag in a sign of solidarity after the Paris bombings. Source: Wendling 2015
Figure 1. The profile picture of Mark Zuckerberg, founder of Facebook, superimposing the French flag in a sign of solidarity after the Paris bombings. Source: Wendling 2015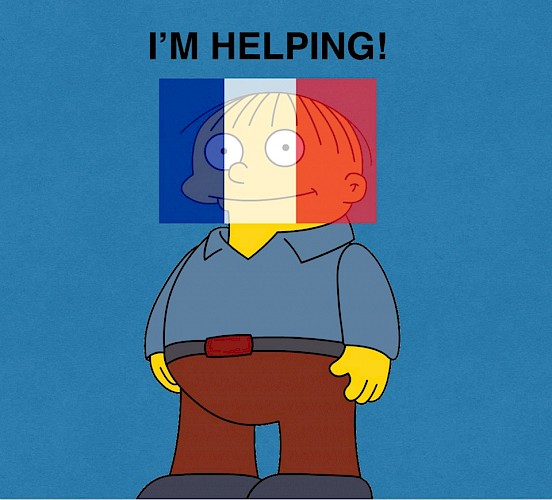 Figure 2. A picture of Ralph Wiggum, a character on the television show *The Simpsons*, with the French flag superimposed. This image was distributed through sites like Reddit as a criticism of the ‘slacktivism’ of Facebook users who, as a sign of solidarity, added the French flag to their profile pictures using a filter provided by Facebook. Source: https://www.justpo.st/post/46780.
Figure 2. A picture of Ralph Wiggum, a character on the television show *The Simpsons*, with the French flag superimposed. This image was distributed through sites like Reddit as a criticism of the ‘slacktivism’ of Facebook users who, as a sign of solidarity, added the French flag to their profile pictures using a filter provided by Facebook. Source: https://www.justpo.st/post/46780.As health professionals, we struggle with how to respond to such events in a ‘global community’ stitched together by social and broadcast media, even when coverage is balanced. We write as health professionals who have trained and worked in Lebanon and who wish to navigate between the call to action and the diffusion of responsibility that can both unfold through media coverage of violence. What would taking responsibility for responding to a bombing in Paris, Lebanon, or Iraq look like in the context of medical education? We believe that responding positively requires a framework for how to analyze and integrate such global events into how we approach medical education.
Structural violence and media coverage: A Lebanese perspective
Using social media to decry the double standard employed by Western media in coverage of ISIS-led violence, people living in or involved in Lebanon were able to generate an alternative discourse (see for example Fares 2015). Nadine Ajaka (2015) writes in The Atlantic: ‘When language skews narratives, and institutional giants like Facebook encourage flag filters in solidarity with one tragedy but not others, it’s difficult to make the argument that the media landscape we all stumble through is anything approaching equitable—or to avoid the impression that white victims are being humanized in a way Arab victims aren’t’.
Media coverage of violence in Lebanon (or lack thereof) points to a larger characterization of the archetypal Arab body in modern geopolitical discourse, or, more bluntly, how the specter of orientalism continues to haunt the discussion of who is worthy of discussion, whose victimization is important, and who deserves the charity of the non-Arab world (see Said 1979; Fassin 2011; Ticktin 2011; Good et al. 2014). The normalization of suffering in the Middle East, embodied in differential news coverage, is important beyond the cultural and symbolic meaning of the brown body. From a medical perspective, the fact that violence is seen as an unremarkable, everyday occurrence in mediated representations of the region is horrifying because it simplifies an otherwise rich conversation about the global nature of inequality. Media coverage in times of violence is one of the variables in a matrix of influences that affects Lebanese, Palestinian, and Syrian people, determining the projects global donors choose to fund, the actions of international aid workers, and ultimately the health outcomes of individuals living in places like Bourj al-Barajneh (see Krauss 2014).
The nature of violence and suffering within Lebanon has multiple faces, based on characteristics as varied as religion, socioeconomic status, and citizenship (Kukrety and Al Jamal 2016; McManus 2017). For example, Palestinians are barred from holding jobs in professional sectors (Chaaban et al. 2010).[note 3] Coupled with a highly privatized, neoliberal marketplace for access to medical care, Palestinians face a significant economic hurdle to accessing adequate primary health care and needed surgical interventions (Kronfol and Bashshur 1989; Sibai and Sen 2006; Premkumar, Raad, and Haidar 2016; Feldman 2017). Confessionalism within Lebanon allows for disproportionate Maronite control within the government despite being a minority population in a democratic political system.[note 4] All sects in Lebanon share a long, ambivalent history with the Syrian people that influences health outreach in the ongoing Syrian refugee crisis (see Parkinson and Behrouzan 2015; Traboulsi 2007). The concept of who can get health care, which clinic or hospital can be visited, and who can access private insurance is highly dependent on confessional and socioeconomic status. How large-scale violence impacts a highly divided, marginalized area reflects back inadequacies not only in sociostructural support services but also pre-existing fractures within the health-care system itself (Farmer 2011).
Within Lebanon, the confessional governmental system and the refugee question have both framed the context in which individuals impacted by the ISIS bombing have sought access to care and attempted to rebuild their lives. In major Western news outlets, attention to these important elements of the backstory was severely curtailed. In an effort to feed the desires of rapid news cycle and the short attention spans of consumers, mass media outlets routinely reduce complex stories to a set of basic points. In Western mass media coverage, these simultaneously reify and naturalize violence within the Arab world, conveying a trope of the Arab body as responsible for positioning itself within a dangerous environment. Violent acts – by ISIS or another group – and their immediate aftermath are reduced to such points within a given news cycle (see Feldman 1994).
It is difficult to quantify whether the brief mention of lives lost in a foreign context in televised or print media, or as a hashtag on social media, ultimately leads to better global engagement with places plagued by ‘acute-on-chronic’ violence such as Lebanon (Farmer 2011). Pippa Norris, Montague Kern, and Marion Just (2003) propose that media coverage is shaped by governments, social groups, individual personal experience, and policy; furthermore, news coverage of events weighs heavily on public opinion and policy, eventually feeding back into the framework leading to perspectives on future and past violent activities. Therefore, a limited contextualization of violence leads to poor public policy, which will, in turn, impact further reporting, all the while contributing to constructing inadequate interventions to help a population in need. As physicians and social science researchers, we are less interested in the anthropological theory behind such criticisms of the media and more in the media’s impact on how medical aid is afforded to those affected by the bombings in Beirut.
The importance of contextualization as it relates to what types of health-care issues are considered important is illustrated via Didier Fassin’s (2011, 2) conceptualization of humanitarianism, which includes two dimensions: ‘on the one hand the generality of human beings who share a similar condition (mankind), and on the other an affective movement drawing humans towards their fellows (humanness). The first dimension forms the basis for a demand for rights and expectation of universality; the second creates the obligation to provide assistance and attention to others’. In other words, exposure to suffering is how individuals in other parts of the world galvanize assistance towards others. The lack of adequate sociohistorical background of a given event, such as the bombings in Beirut, can lead not only to the creation of a dissimilar human condition but also to a lack of connection between individuals both within and outside a given community. Biomedical care is directly influenced by such forces, and in a health-care system such as Lebanon’s – divided both socioeconomically and confessionally – the aftermath of physical violence continues to find itself recycled in the long-term health outcomes of marginalized groups. The way health-care policy is structured and enacted is impacted not only by disease burden and economic theory but also by what diseases are deemed as important from both a biomedical and moral perspective (Basilico et al. 2013; Suri et al. 2013).
A critical humanitarianism: What social medicine can offer
We propose that portrayals of violence in the media are within the scope of interest of medical providers because they impact patient outcomes, such as adherence to certain medications or decreased morbidity rates among those with chronic diseases. What action can a community of health providers with a perspective grounded in social medicine theory do to affect the business of media? We believe there is a way to move from an analysis of the ethical implications of a news cycle to a sustained push for advocacy.
The conventional biomedical approach emphasizes rigorous, quantitative studies in the shaping of clinical practice, though this is a highly contested arena within medical anthropology (Adams 2016). Using literature focused on the anthropology of humanitarianism and structural violence, we have begun to sketch the evidence connecting upstream factors related to media portrayals and downstream factors related to patient outcomes. The causal pathway we are describing is long, requiring an interdisciplinary approach to strengthen this framework.
But what is the starting point? Looking towards education, the philosophers Brad Evans and Henry Giroux (2016) present a series of challenges to tackle the issue of violence:
What are the deeper political, educational, and social conditions that allow a climate of hate, racism, and bigotry to become the dominant discourse of a society or worldview? What role do politicians with their racist and aggressive discourses play in the emerging landscapes violence? How can we use education, among other resources, to prevent politics from being transformed into a pathology? And how might we counter these tragic and terrifying conditions without retreating into security or military mindsets?
Taking a page from Evans and Giroux, we suggest that changing health systems starts with targeted advocacy focused on giving physicians analytical tools during their medical education; such tools should connect social forces with patient outcomes (see Premkumar et al. 2016). This biosocial connection – reiterating that ‘biologic and clinical processes are influenced by society, political economy, history, and culture and are best understood as interactions of biological and social processes’ (Hanna and Kleinman 2014, 17) – can influence values related to research agendas and methodology (see Closser and Finley 2016). To begin the journey connecting media coverage, violence, and patient outcomes we call on the research community to explore the intersection between medical education, social medicine, and health outcomes in regards to violence in the media.
So how do we move forward? We turn to Edward Said’s (2001, 222) words in ‘Orientalism and After’: ‘The marginalization, the ghettoization, the reification of the Arab, through Orientalism and other processes, cannot be answered by simple assertions of ethnic particularity or glories of Arabic, or returning to Islam and all the rest of it. The only way to do it is to get engaged, and to plunge right into the heart of the heart, as it were’.
Plunging into ‘the heart of the heart’ requires a larger conversation about the construction of inequality and the aftermath of violence in marginalized communities. From a biomedical perspective, it requires an acknowledgement that the background in which violence occurs has tangible, immediate, and long-term health outcomes. Above all, it requires the politicization of groups, such as physicians, who continue to serve in clinics and hospitals in areas like Bourj al Barajneh. As we have mentioned in previous work, multidisciplinary education at the premedical and medical level allows for traditional tools in the clinician’s armory to migrate from the clinical encounter to a wider form of advocacy (see Premkumar et al. 2016). Targeted educational efforts by individuals working at the intersections of public health, humanitarianism, and media studies can allow clinical tools, like the social history, to have wider biosocial consequences. All of these aforementioned acts start with a simple acknowledgement that ‘language skews narratives’ in the wider context of discussing violence in places like Paris, Beirut, and Baghdad, especially highlighted again with the summer 2016 attacks in Istanbul, Dhaka, and Baghdad (Tharoor 2016). Indeed, it is the first step in a longer discussion of how researchers, journalists, and caregivers can contribute to a critical humanitarianism designed not only to help those in need but also to build more just and equitable societies.
About the authors
Ashish Premkumar, MD, is a chief resident in the Department of Obstetrics, Gynecology, and Reproductive Sciences at University of California San Francisco. He will begin a maternal-fetal medicine fellowship in the Department of Obstetrics and Gynecology at Northwestern University in Chicago, Illinois. He was a member of the Seven-Year Accelerated Liberal Arts/Medical Education Program at Boston University. During his time in medical school, he completed medical anthropological research focusing on reproductive health perceptions in low-income neighborhoods in Beirut, Lebanon. His research focuses primarily on substance abuse in pregnancy, high-risk pregnancies, humanitarianism and reproductive health care in Lebanon, and physician advocacy.
Kareem Raad, MD, MPH, is a first-year resident in the Department of Family Medicine at Abrazo Central Campus in Phoenix, Arizona. He earned his Master’s in Public Health at the University of California Berkeley in Interdisciplinary Studies and completed his medical degree at the Lebanese American University Chagoury School of Medicine. His prior research focused on medical education, specifically bilingual medical training and teaching physician advocacy through a social medicine approach. He plans to practice primary care both in the United States and Lebanon.
References
Adams, Vincanne, ed. 2016. Metrics: What Counts in Global Health. Durham, NC: Duke University Press.
Akaja, Nadine. 2015. ‘How the Media Covered the Paris and Beirut Attacks – and Why It Matters’. The Atlantic, 17 November. http://www.theatlantic.com/international/archive/2015/11/paris-beirut-media-coverage/416457/.
Al Jazeera. 2015. ‘Fear and Confusion in Paris after Deadly Attacks’. Al Jazeera, 14 November. http://www.aljazeera.com/news/2015/11/reports-shooting-restaurant-central-paris-151113211237312.html.
Almasy, Steve, Pierre Meilhan, and Jim Bitterman. 2015. ‘Paris Massacre: At Least 128 Killed in Gunfire and Blasts, French Officials Say’. CNN, 14 November. http://www.cnn.com/2015/11/13/world/paris-shooting/.
Associated Press. 2015. ‘Iraq: Suicide Bomb and Road Blast Kill 26 in Baghdad’. New York Times, 13 November. https://www.nytimes.com/2015/11/14/world/middleeast/iraq-suicide-bomb-and-road-blast-kill-26-in-baghdad.html.
Barnard, Anne. 2015. ‘Beirut, Also the Site of Deadly Attacks, Feels Forgotten’. New York Times,15 November. https://www.nytimes.com/2015/11/16/world/middleeast/beirut-lebanon-attacks-paris.html.
Barnard, Anne, and Hwaida Saad. 2015. ‘ISIS Claims Responsibility for Blasts That Killed Dozens in Beirut’. New York Times, 12 November. https://www.nytimes.com/2015/11/13/world/middleeast/lebanon-explosions-southern-beirut-hezbollah.html.
Basilico, Matthew, Jonathan Weigel, Anjali Motgi, Jacob Bor, and Salmaan Keshavjee. 2013. ‘Health for All? Competing Theories and Geopolitics’. In Reimagining Global Health: An Introduction, edited by Paul Farmer, Jim Yong Kim, Arthur Kleinman, and Matthew Basilico, 74–110. Berkeley: University of California Press.
Chaaban, Jad, Hala Ghattas, Rima Habib, Sari Hanafi, Nadine Sahyoun, Nisreen Salti, KarinSeyfert, and Nadina Naamani. 2010. Socio-Economic Survey of Palestinian Refugees in Lebanon. Beirut: American University of Beirut. http://unrwa.org/userfiles/2011012074253.pdf.
Closser, Svea, and Erin P. Finley. 2016. ‘A New Reflexivity: Why Anthropology Matters in Contemporary Health Research and Practice, and How to Make It Matter More’. American Anthropologist 118, no. 2: 385–90.
Evans, Brad, and Henry A. Giroux. 2016. ‘The Violence of Forgetting’. New York Times, 20 June. http://www.nytimes.com/2016/06/20/opinion/the-violence-of-forgetting.html.
Fares, Elie. 2015. ‘From Beirut, This Is Paris: In a World That Doesn’t Care about Arab Lives’. State of Mind (blog), 14 November. http://stateofmind13.com/2015/11/14/from-beirut-this-is-paris-in-a-world-that-doesn’t-care-about-arab-lives/.
Farmer, Paul. 2011. Haiti after the Earthquake. New York: Public Affairs.
Fassin, Didier. 2011. Humanitarian Reason: A Moral History of the Present. Berkeley: University of California Press.
Feldman, Allen. 1994. ‘On Cultural Anesthesia: From Desert Storm to Rodney King’. American Ethnologist 21, no. 2: 404–18. https://doi.org/10.1525/ae.1994.21.2.02a00100.
Feldman, Ilana. 2017. ‘Humanitarian Care and the Ends of Life: The Politics of Aging and Dying in a Palestinian Refugee Camp’. Cultural Anthropology 32, no. 1: 42–67. https://doi.org/10.14506/ca32.1.06.
Good, Byron J., Mary-Jo DelVecchio Good, Sharon Abramowitz, Arthur Kleinman, and Catherine Panter-Brick. 2014. ‘Medical Humanitarianism: Research Insights in a Changing Field of Practice’. Social Science & Medicine 120: 311–16. https://doi.org/10.1016/j.socscimed.2014.09.027.
Hanna, Bridget, and Arthur Kleinman. 2014. ‘Unpacking Global Health: Theory and Critique’. In Reimagining Global Health: An Introduction, edited by Paul Farmer, Jim Yong Kim, Arthur Kleinman, and Matthew Basilico, 15–32. Berkeley: University of California Press
Krauss, Monika. 2014. The Good Project: Humanitarian Relief NGOs and the Fragmentation of Reason. Chicago: University of Chicago Press.
Kronfol, Nabil M., and Rashid Bashshur. 1989. ‘Lebanon’s Health Care Policy: A Case Study in the Evolution of a Health System under Stress’. Journal of Public Health Policy 10, no. 3: 377–96. https://doi.org/10.2307/3342798.
Kukrety, Nupur, and Sarah Al Jamal. 2016. Poverty, Inequality and Social Protection in Lebanon. Beirut: Issam Fares Institute for Public Policy and International Affairs, American University of Beirut. https://www.aub.edu.lb/ifi/publications/Documents/research_reports/20160426_poverty_inequality.pdf.
McManus, Shea. 2017. ‘The Right to Know: Suffering, Human Rights, and Perplexities of Politics in Lebanon’. American Ethnologist 44, no. 1: 104–117. https://doi.org/10.1111/amet.12429.
Norris, Pippa, Montague Kern, and Marion Just. 2003. ‘Framing Terrorism’. In Framing Terrorism: The News Media, the Government, and the Public, edited by Pippa Norris, Montague Kern, and Marion Just, 3–26. 1st ed. New York: Routledge.
Parkinson, Sarah E., and Orkideh Behrouzan. 2015. ‘Negotiating Health and Life: Syrian Refugees and the Politics of Access in Lebanon’. Social Science & Medicine 146: 324–31. https://doi.org/10.1016/j.socscimed.2015.10.008.
Premkumar, Ashish, Kareem Raad, and Mona H. Haidar. 2016. ‘Rethinking the Social History in the Era of Biolegitimacy: Global Health and Medical Education in the Care of Palestinian and Syrian Refugees in Beirut, Lebanon’. Anthropology & Medicine 23, no. 1: 14–29. https://doi.org/10.1080/13648470.2015.1135785.
Premkumar, Ashish, Karma Salem, Sarah Akhtar, Mary E. Deeb, and Lisa J. Messersmith. 2012. ‘Sectarianism and the “Problem of Overpopulation”: Political Representations of Reproduction in Two Low-Income Neighborhoods of Beirut, Lebanon’. Culture, Health, &Sexuality 14, no. 10: 1139–52. https://doi.org/10.1080/13691058.2012.721137.
Reddit. 2015. ‘I’m Helping!’ Reddit (forum),16 November. https://www.reddit.com/r/funny/comments/3tepel/im_helping/.
Said, Edward W. 1979. Orientalism. New York: Vintage Press.
Said, Edward W. 2001. ‘Orientalism and After’. In Power, Politics, and Culture: Interviews with Edward W. Said, edited by Gauri Viswanathan, 208–232. New York: Vintage Books
Samaha, Nour. 2015. ‘Deadly Suicide Attack Rocks Southern Beirut’. Al Jazeera, 14 November. http://www.aljazeera.com/news/2015/11/multiple-explosions-reported-southern-beirut-151112162331001.html.
Shenton, Zoe. 2015. ‘Celebrities Flock to Twitter to Send Message in Support in Wake of Horrific Paris Atrocities’. Daily Mirror, 14 November. http://www.mirror.co.uk/3am/celebrity-news/celebrities-flock-twitter-send-messages-6830686.
Sibai, Abla-Mehio, and Kasturi Sen. 2006. ‘Can Lebanon Conjure a Public Health Phoenix from the Ashes?’ British Medical Journal 333: 848–49. https://doi.org/10.1136/bmj.38996.466678.68.
Suri, Arjun, Jonathan Weigel, Luke Messac, Marguerite T. Basilico, Matthew Basilico, Bridget Hanna, Salmaan Keshavjee, and Arthur Kleinman. 2013. ‘Values and Global Health’. In Reimagining Global Health: An Introduction, edited by Paul Farmer, Jim Yong Kim, Arthur Kleinman, and Matthew Basilico, 245–86. Berkeley: University of California Press.
Tharoor, Ishan. 2016. ‘The Worst ISIS Attack in Days Is the One the World Probably Cares Least About’. Washington Post, 4 July. https://www.washingtonpost.com/news/worldviews/wp/2016/07/03/the-worst-alleged-isis-attack-in-days-is-the-one-the-world-probably-cares-least-about/.
Ticktin, Miriam. 2011. Casualties of Care: Immigration and the Politics of Humanitarianism in France. Berkeley: University of California Press.
Traboulsi, Fawaaz. 2007. A History of Modern Lebanon. London: Pluto Press.
UNHCR (United Nations Commissioner for Refugees). 2011. States Parties to the 1961 Convention and Its 1967 Protocol. 1 April. http://www.unhcr.org/3b73b0d63.html.
Wendling, Mike. 2015. ‘BBC Trending: Millions Are Sharing Attack Stories That Aren’t about Paris’. BBC, 16 November. http://www.bbc.com/news/blogs-trending-34833134.
Endnotes
1 Back
Evaluation of major news outlets – such as the BBC, CNN, the New York Times and the Washington Post – shows that much of the commentary regarding the bombings in Beirut was limited in both amount of text and depth of coverage. In contrast, the bombings in Paris, covered by Middle Eastern media groups like Al Jazeera, generated more in-depth coverage and contextualization of the bombings themselves (see Al Jazeera 2015; Samaha 2015).
2 Back
As Mike Wendling (2015) of the BBC notes, ‘The hashtag “Pray for Lebanon” . . . was in particular used more than 800,000 times on Twitter. The vast majority of those tweets came not at the time of the bombs in Lebanon, but after the Paris attacks (“Pray for Paris” hashtag has been used more than 10 million times)’. For a critique of the social media response to the Paris bombings, please see figure 2.
3 Back
Lebanon is not a signatory to the 1951 Convention relating to the status of refugees or its 1967 protocol (UNCHR 2011), and thus does not bestow the status of refugee or asylee. This fact has important sociolegal consequences for displaced Palestinians and Syrians.
4 Back
Confessionalism, or the organization of political groups by religious identification, is a core component of government in Lebanon. Based primarily on census data from 1932 and imported into law through the 1943 National Pact, confessionalism has undergone changes over the last seventy years, especially in the wake of the Lebanese Civil War and the accompanying Ta’ef Accords of 1989 (Traboulsi 2007). Yet the use of population size of given sects as a means to justify different positions within the government continues (see Premkumar et al. 2012).