Donor data vacuuming
Audit culture and the use of data in global health partnerships
—
Abstract
The new oil
During Fortune magazine’s annual, invitation-only ‘Brainstorm Tech’ conference in 2016 in Aspen, Colorado, a venture capitalist named Shivon Zilis announced to the crowd of leaders from Fortune 500 companies and top emerging entrepreneurs of the tech world, ‘Data is the new oil’ (quoted in Vanian 2016).[[id1]] This declaration embraces the increasing market value that data holds, not simply as a tool for making corporations more efficient or effective but also as a currency of the global marketplace itself. In postcolonial states marred by centuries of violent extraction economies, this announcement holds particular poignancy and a fair measure of threat. In these states and economies, too, data is capital, but capital of another sort, in the service of global health, development, and aid projects. And in global health in particular, data is capital that is harvested from sites, passed between partners, used to audit and surveil systems, and ultimately deployed to justify and promote subsequent rounds of project making and data gathering. These dynamics, which we call ‘data vacuuming’, are a key feature of contemporary global health projects and partnerships, and yet another way in which those with power in the global health field reinforce their position by controlling health information access, flow, and use. We deploy the vacuuming trope because it captures the sense that anything of value in these impoverished health settings is mined, essentially sucked out. Indeed, as we argue here, ‘data is the new oil’ not only in its neocolonial value and extractive dynamics but in its capacity to grease the wheels of global health partnerships that are often also inequitable.
With the signing of the Alma Ata declaration at the International Conference on Primary Health Care, held in Alma Ata in 1978, countries around the globe committed to ensuring health as a human right, acknowledging that ‘all countries should cooperate in a spirit of partnership and service to ensure primary health care for all people since the attainment of health by people in any one country directly concerns and benefits every other country’ (World Health Organization 1978). This declaration was the first to express the need for urgent universal action by governments, health and development workers, and the world community to protect and promote the health of all people. It was also the first to declare the express importance of primary health care – and of partnerships and solidarity – as core strategies. However, soon after this historic document was signed, and in response to the global economic crisis and subsequent rise of neoliberalism in wealthy nations, the goal of primary health care for all was modified to ‘selective primary health care’ by larger donor nations who felt overwhelmed by the potential financial implications of fully accepting this global mandate. This turn toward selective primary health care prioritized technological ‘silver bullet’-type interventions designed to address specific diseases and deemed practical, financially feasible, measurable, and politically unthreatening (Brown, Cueto, and Fee 2006). Data vacuuming emerges out of this strange trajectory of efforts to build health systems in developing countries over the past few decades after the ideal of Alma Ata was abandoned (Packard 2016). A similar approach continues today, fueled by the push to translate a neoliberal ethos into the health sector, and has evolved into a de facto acceptance of evidence-based medicine and ‘cost-effective’ strategizing.
These trends have coalesced into a heightened reliance on multiplying and increasingly disaggregated health indicators in order to measure project outcomes, which has facilitated support for data vacuuming activities and expanded public–private partnerships. Vincanne Adams (2016) discusses this distorting preoccupation with health metrics, and how it impacts what interventions are funded and delivered in the global South. She looks not only at the cult of metrics but also how this fixation has afforded a small group of nongovernmental organizations (NGOs) enough power to effectively shape health services for millions. She argues that by focusing only on what is quantifiable, there is a devaluation of what cannot be measured, even if the unmeasurable is what is ultimately most important to patients (Adams 2016). Simultaneously, global health is witnessing the evolution of an ‘unruly mélange’ of multilateral and bilateral donors and NGOs, who in addition to strongly influencing health funding priorities, have paved the way for private-sector partners and industry-linked foundations to enter into the international health arena (Buse and Walt 1997). ‘Partnerships’ are established between the host governments and this mélange of actors. But these working relationships, rather than emulating the ideals of the Alma Ata declaration, are anchored by an infusion of financial accountability systems and tools, and enabled through the insatiable provision of data for donors (Adams 2016).
In this article, we seek to understand how the dramatic proliferation of data vacuuming, facilitated under the auspice of ‘partnership’, has fundamentally transformed how routine health data in poor countries is collected, analyzed, prioritized, and used to inform both management and policy. Writing as a team of authors with experiences on multiple sides of global health partnerships in the United States, Mozambique, Nepal, Lesotho, Kenya, and Cote d’Ivoire, we argue that solidarity-based partnership between donor and recipient countries is impossible when evidence production and management is effectively outsourced to external organizations in order to meet the criteria of donor partners.
The global health ‘space’
In the last fifteen years, an increasing number of individuals from the technology field have participated in and influenced global health, which has resulted in both changes to the field and its lexicon. One often-used phrase by this powerful group is ‘global health space’, which is used by global health ‘techies’[note 1] to convey their view of the field as potentially expansive and influential in and across countries and regions, both in terms of positive impact on population-level health and potential opening of markets (Kenworthy this issue). Data is fundamental to this potential. In the Bill & Melinda Gates Foundation resource Global Health Envisioning: Data for Impact, data is highlighted as a critical means to ‘inform better decisions across the global health and development space’ (Bill & Melinda Gates Foundation 2015).
The encroachment of data vacuuming into the global health ‘space’ is in many ways linked to the changing landscape of the health sector in low- and middle-income countries (LMICs) that is defined increasingly by NGO projects substituting for public sector health systems (Smith 2007). Crane (this issue) maintains that the optimistic public face of partnership espoused by donor and NGO partners in fact veils deep Western anxieties surrounding African corruption and mismanagement (see also Okeke this issue; Boum this issue). Pfeiffer (2003) has documented how international aid was being increasingly channeled through NGOs rather than directly to ministries of health and implemented via expatriate technical advisors in resource-constrained settings, a phenomenon he felt was fueled primarily by the neoliberal focus on privatization. Regardless of the main drivers, in recent years, funds flowing to NGOs from bilateral institutions and foundations have been greater than entire local government investments in the health sector, and the planning and management of these NGO projects falls fully outside the span of local government control. According to a recent report, NGOs, along with private foundations, have made the most significant gains in attracting development assistance for health, representing 30.1 percent in 2016 compared with 7.6 percent in 1990 (an astonishing 2,005 percent increase over the twenty-seven year period) (Institute for Health Metrics and Evaluation 2017).
Thus, along with the ‘projectification’ and ‘vertical funding’ of public health has come the burden of enormous data collection demands by donors to demonstrate achievement of short-term and narrowly defined outcomes as well as the ‘cost effectiveness’ of specific interventions (Whyte 2013). The resulting mainstreaming of data vacuuming for specific vertical programs into global health practice has resulted in the creation of a narrow silo of public health practice and an abandonment of support for public sector health systems that provide integrated primary health care services (Pfeiffer 2016). Storeng and Béhague (2014) have argued that the shift toward ‘playing the numbers game’ is influencing much more than the development of, and adherence to, uniform indicators or targets. Rather, it is influencing how medical and public health research is conceptualized, carried out, understood, and disseminated.
The increasing focus on donor-defined and donor-driven data collection and metrics is part of the larger shift toward ‘audit culture’, where donor countries and global initiatives determine funding priorities for recipient countries and where administrators and accountants, rather than programmatic experts, take on the role of measuring and evaluating performance, and as such are funding gatekeepers (Strathern 2000). As Shore and Wright (2015, 24) state, ‘What is new about audit culture is the extent to which measurement and ranking have become institutionalised, extended and above all, financialized’.They also note that language around global health organizational governance has changed to reflect this influence. Words such as ‘assets’, ‘income’, ‘liability’, ‘opportunity costs’, ‘products’, ‘output’, ‘overheads’, ‘revenue’, ‘return on investment’, ‘transparency’, and ‘value for money’ have joined the everyday global health lexicon and convey an assumed sense of objectivity, despite its very real subjectivity (Shore and Wright 2015).
Audit cultures in global health also reinforce hierarchical roles. Those who control financial resources are the donors, such as bilateral or multilateral agencies; those who decide what is being measured are the NGOs, under the influence of specific donors; and those who must measure are the ministries of health, or, when ministry capacity is limited, NGOs (or ‘implementing partners’ as they are aptly referred to in-country), complete this duty. Thus, ‘playing the numbers game’ has reinforced a power dynamic that makes untenable any possibility of equal partnership as conceptualized at Alma Ata. The auditing and infusion of targets and indicators for data vacuuming are now largely defined at a distance, by large global donors who have systematically asserted their power and control via remote surveillance (Greenhalgh 1996; Birn 2009).
This phenomenon occurs in a context of steep resource inequities that fuel data vacuuming practices. NGOs, specifically implementing partners funded by the US President’s Emergency Plan for AIDS Relief (PEPFAR), have clean, expansive offices with multiple functional printers, copiers, faxes and other devices. They are fully staffed, and salaries are large and include benefits, at least for expatriate staff, such as schooling allowances for children and generous housing subsidies (Pfeiffer 2003). Most multilateral and bilateral donors have followed suit and keep up with the salaries and benefits of PEPFAR-funded NGOs on the premise that they need to be competitive in the ‘development staffing market’. By contrast, ministry of health personnel operate in a parallel, underfunded reality, facing limited staffing and budgets that are compounded by shortages of materials and constant resource challenges. In addition to encouraging brain drain, these constraints make them beholden to the priorities of funding agents, be they multilateral or bilateral donors, foundations, or NGOs.
This is not a new phenomenon. During a conversation in 2006 between the Ministry of Health’s head of health information systems in Mozambique and one of the authors of this article, the informant revealed that her technical counterpart, a European man with a graduate degree in computer science, seconded to support her and the program through the German Development Bank, received a salary of €7,000 (equivalent of US$8,800 per month), excluding benefits. In contrast, she, a trained physician, earned a monthly salary of 19 million meticais (equivalent of US$670 per month). This phenomena of ‘technical advisors’ who are embedded to varying degrees within government ministries is not novel; however, the salary differentials between the often expatriate advisors and the local managers have grown dramatically in the last two decades as development assistance for health has expanded (Carr et al. 2010). Similar inequities are reflected in staff housing built by the Finnish Development Agency in the 1990s in a central province of Mozambique. Expatriate personnel lived in a gated community with lawns and a pool, while the housing of locally recruited personnel was located just outside the walls, in a long row of basic two-room houses. The development was known locally by the nickname, ‘Soweto and Pretoria’, after the largely poor and black township, and the mostly rich and white city, in South Africa. These distortions, created by development, have led to the increasing divide between the needs and priorities of these two entities, the global health industry and the local ministries of health, which have facilitated the rise of donor data vacuuming.
Donor data vacuuming in practice
Audit culture and global financing systems
Most poor countries depend on aid from wealthy bilateral and multilateral partners to meet the basic health needs of their citizens. Dependency on aid has been cited as a significant negative side effect of sustained aid to poorer countries (Moyo 2009). Others have argued that international aid prevents country development and sustainable economic growth if administered, intentionally or not, as a long-term strategy that consequently inhibits development, progress, or reform (World Health Organization Maximizing Positive Synergies Collaborative Group 2009; Daschle 2015; Stanford 2015). Stanford (2015) argues that real or perceived aid dependency can extend beyond the economic and financial realms to include the political, when dependency leads to corruption. Often in these cases donor countries devise complex auditing practices including tied-aid strategies, such as vertical funding of specific, donor-prioritized programs, establishing funding conditions, and/or routing funding through intermediaries such as NGOs and multilateral agencies.
Emanating from the paradigm of ‘audit culture’, defined by Shore and Wright (2015, 24) as ‘the process by which the principles and techniques of accountancy and financial management are applied to the governance of people and organisations – and, more importantly, the social and cultural consequences of that translation’, these donors’ mechanisms for ensuring recipient country accountability ultimately hand greater control to the donor country in determining indicators and targets, and the means of aid collection and disbursement. This can fundamentally negate the partnership agreement, and encourage what Shore and Wright (2015, 24) refer to as ‘steering government from a distance’. This further entrenches recipient countries in a cycle of donor dependency beyond their control, as donor agencies are increasingly beholden to their own government’s political structures and domestic constituent priorities, rather than those of the countries they purport to support. This donor culture and the practices it has instituted have facilitated the evolution and growth of donor data vacuuming. In fact, data vacuuming is one amongst a set of practices that legitimize donor-defined indicators, as well as delegitimize the priorities of recipient countries and their citizens.
Data vacuuming expands
A key characteristic of these strategies is the ongoing expansion of new, donor-defined indicators and targets for vacuuming. These may be instituted to measure investments in the health system, such as the enumeration of completed activities, the number of people served in a specific service, the measures of clinical outcomes for patients using the health system, the measures of health system efficiency and quality to describe the functionality of services, and finally population-level measures that reflect the impact of aid on the health of populations of interest. Enhanced monitoring and evaluation systems are deemed important and necessary to discern the most effective strategies in health system design, to ensure health service quality, and to identify underserved populations and service gaps in need of improvement.
Data vacuuming reinforces audit culture by justifying increased governance by and through numbers, algorithms, and audits that drive the development of ‘ever more sophisticated systems of knowledge and power that indicators and rankings provide’ (Shore and Wright 2015, 23). Others have noted that in these audit systems, the more the system fails, the more it succeeds; specifically, the system succeeds in further entrenching the accountability system and values of the donor instead of those of the recipient government (Strathern 2000). Workload for the recipient countries grows in order to meet the increased need for data in ever more disaggregated categories, further justifying the need for donor support. We argue that the development and adoption of these indicators is driven by donors, and are in place primarily to ensure that countries achieve donors’ programmatic priorities, rather than strengthen the health system’s ability to manage itself and ensure broad, evidence-based health care is provided effectively and efficiently.
The idea that measures become the targets at the expense of all else has arisen across studies of audit (Power 1994, 1997; Strathern 2000; Hoskin 1996). For example, the widely applied disability-adjusted life year (DALY) metric attempts to capture the effect of diseases and disabilities on production by quantifying the gap between current health status and an ideal health situation (World Health Organization 2017). Critics have questioned whether the DALY measure is effective for a number of reasons, critiquing: 1) its inability to detect differences in experiencing the same disability across individuals and cultures; 2) its implied use as a community-based measure when it was developed for individual-level understanding; 3) its inability to account for ‘total disability impact’ (whereby the impact of disability on the individual as well as on their partners, children, and communities is captured); and, perhaps most importantly, 4) its failure to take into account cultural and gender-specific health concerns (Laurie 2014; Farmer 2013; Arnesen and Nord 1999). These critiques resonate with our argument that DALYs and other elements of audit culture amplify those health issues that can be measured and omit those that don’t fit (Nichter 2008). Likewise, these globally agreed-upon measures don’t always fit when applied to smaller groups working in smaller, sometimes-fragmented catchment areas. They are, simply, reductive in their approach of what they seek to measure (Adams 2016).
PEPFAR, since its inception in 2003, has had possibly the greatest impact on the expansion of audit culture in donor-recipient nations, specifically those with the highest burden of HIV/AIDS. As of 2017, PEPFAR has contributed more than US$70 billion to ameliorate the effects of HIV/AIDS and eradicate its transmission, and has, until recently, received strong bipartisan support within the US political system (PEPFAR, 2017a). The tremendous amount of money from this initiative provided its power brokers – namely USAID and the Centers for Disease Control and Prevention (CDC), and their implementing agencies (NGOs) – with an immediate and outsized influence on the data used to assess their impact (Pfeiffer et al. 2010). Within the structure of PEPFAR, the majority of funds are provided to NGOs that work with health systems at national, subnational, and health-facility levels. The advent of NGOs funded via PEPFAR as implementing partners has introduced new challenges, including donor coordination and the phenomenon of internal brain drain (Pfeiffer et al. 2008; Sherr et al. 2012).
PEPFAR responds to the United States Congress for continued funding, and thus the interests of US lawmakers (whether or not they are the same as recipient countries) are prioritized. In order to continue receiving acutely needed funding, health managers in recipient countries must continue to meet the data expectations of donors. This capacity building requires the creation of expanded monitoring and evaluation systems that both take up space and influence priorities (Douglas-Jones 2018). For example, between 2010 and 2017, the number of reporting indicators required by PEPFAR of recipient entities decreased from forty to twenty-nine. However, the collection of disaggregated data per indicator skyrocketed. In 2010, an additional thirty-plus data points were needed to comply with disaggregation requirements, including differing age groups by gender (which were not in sync with country-level classifications), HIV status, adherence level, reporting period, treatment status, and project funding (PEPFAR 2017b). By 2017, more than 350 additional data points were required, an amount that varied depending on the types of projects funded (PEPFAR 2009, 2017b).
Impact on practice
The last fifteen years has demonstrated that the vacuuming of increasingly complex data eventually demands external support, which alters global health practices. When the collation, analysis, and use of data remain no longer within the purview of local health workers and managers, the use of data to improve health care delivery dissipates. The target moves from improving health outcomes in poorer countries to meeting the goals and benchmarks set by wealthier countries. Donor data vacuuming also leads to resource vacuuming. If recipient countries are not capable of collecting the data points required, then NGOs will collect the data, for a fee from donors, thus further stripping resources from the recipient country’s health care system.
Data vacuuming can be seen as a means to an end in global health, and master narratives such as the Countdown to 2015 initiative are emblematic of this audit logic. Countdown to 2015 was created by a technical working group of ‘experts in the field’: sixty-nine individuals based in the United States, the United Kingdom, Switzerland, and Australia. Although the strategy was intended for countries of the global South, just four (6 percent) of the experts came from the global South (one each from Brazil, Pakistan, South Africa, and Senegal).[note 2] Countdown to 2015 was a global target-setting framework explicitly created to monitor and hold countries accountable for progress made towards the Millennium Development Goals, through the adoption of performance indicators that were intended to stimulate better and stronger efforts at the country level (Requejo 2015). Nichter (2008, 2) has argued that the use and control of data is intentional and required ‘to perpetuate master narratives that shape how solutions to global health problems are conceptualized’. Thus, the exportation of target and audit culture from wealthier countries to poorer countries, through mechanisms such as Countdown to 2015, affords donors the right to create master narratives for beneficiary nations. This includes narratives about making intermittent progress towards constantly moving targets.
Such narratives justify the donors’ putting first their home countries’ concerns over those of beneficiary nations, and they support donor governments’ prioritization of reporting requirements that align with their own political structures, often at the expense of what is feasible and ultimately best for under-resourced health systems in recipient countries. From the perspective of recipient countries, donors’ reporting needs only grow, with new indicators or increasingly disaggregated metrics, each year more onerous to collect, report, disseminate, and use locally.
Figure 1 shows the average full days per quarter that health managers in one district in Tanzania spent writing reports for both the Ministry of Health and donors in 2006, three years after the advent of PEPFAR. This reporting overload takes up a full third of the clinician manager’s time, time that is no longer spent on clinical care, clinical management, service coordination, and quality assurance, which are so important in environments with insufficient human resources.
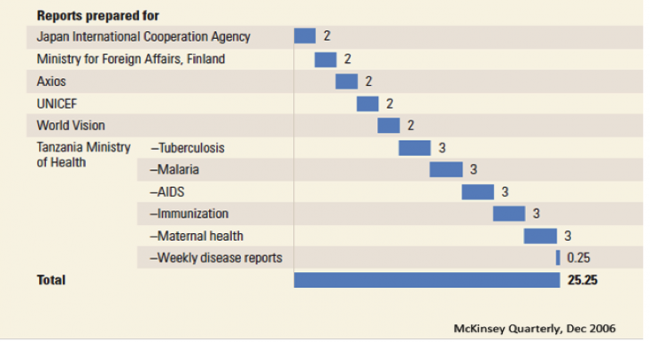 Figure 1. Number of full days per quarter spent writing reports by district medical officer (Morogoro, Tanzania)
Figure 1. Number of full days per quarter spent writing reports by district medical officer (Morogoro, Tanzania)This figure is highly representative of the reporting duties of health facility managers in Tanzania a decade ago, and is similarly representative of the situation in most aid-dependent countries in the region now. However, what has changed in the ten years since, and what these sorts of graphics, produced by McKinsey and other for-profit business consultants, justified, was the transfer of the task of data collection and report writing from the Ministry of Health managers to NGOs (the ‘implementing partners’). This ‘necessary’ transfer of report writing to outside entities fully excludes the health facility staff from any authentic engagement with their data beyond primary documentation, leading to profound changes in how global health is practiced.
As data vacuuming needs increase in number and complexity, the hiring of expatriate advisors, dedicated solely to monitoring and evaluation, is introduced as a practice by external funding agencies to support ministries of health in the revision, updating, and monitoring of their bloated reporting systems, and often carrying out the data collection themselves without participation of ministry of health staff. In many instances, ‘transnational networks’ maintained by NGOs, as described by Appadurai (2000, 17), are delegated to complete these tasks by donors as intermediate technical assistance (ostensibly to ‘build capacity’ in the health workforce to collect these added indicators), or to meet data-driven deliverables that are tied to funding disbursement.
It is also common to see the revision of public sector health forms and registries being carried out by technical working groups composed primarily of bilateral, multilateral, and NGO agency representatives rather than of ministry of health leadership who will ultimately oversee their implementation. These ‘outside’ advisors, with agendas to serve their home governments, wield considerable power and represent donor interests (Redfield 2012). This power imbalance in what should be country-led processes, has produced, in many cases, the veritable silencing of ministry of health employees when key decisions concerning tools and strategies are made. In these selective, technical workgroup meetings, donor representatives are known to make strong cases for their desired strategies, goals, and metrics.
One informant from Mozambique, who has worked for both the Ministry of Health and NGOs, described a particularly tense workgroup meeting where revisions to forms were underway. Over the three-day meeting, the forms steadily grew in length and complexity at the behest of expatriate technical advisors, while the participation of representatives from the Ministry of Health grew steadily more silent. The informant protested the additions, finally taking aside the lead staff person from the ministry in a private conversation, to understand why she wasn’t protesting the forms’ adaptations. The lead replied simply, ‘They are just going to do what they are going to do. It is better not to talk so they can finish’. Another informant who works at the Mozambique Ministry of Health went as far as to call these workgroup meetings ‘donor clubs’ within the Ministry of Health. These institutional practices resonate with those in other countries as well. In Lesotho, monthly health and development ‘partner forums’ were attended by major NGOs, UN agencies, and donors working in Lesotho, but officials from the Ministry of Health and other government agencies were only occasionally invited as guests to join the conversations, which focused on coordinating and streamlining initiatives in the country, including data-gathering practices.
More alarming is the practice – in the name of efficiency and impartiality – of facility-level data collection by external NGO teams, who literally descend on health units and harvest the data required by their donor, with limited to no involvement of health facility staff. In Mozambique, teams will either stay on site and collect data over a series of days or just come out to collect the registry books and bring them back to their NGO offices to harvest in the comfort of air conditioning for a period of days. Industry is stepping forward to meet this new reality, by producing software tools such as Capricity® to vacuum the data into functional datasets for researchers in donor countries. This specific software promises to transform digital photos of registries into databases. This is just one example of the entire industry of donor-driven data collection that sustains and reinforces this unequal partnership under the guise of promoting data for decision making. But the question remains: whose data-driven decision making is being facilitated – that of health managers in poor countries, or the global health industry? Another similar group, AidStream, has also arisen to meet donor reporting needs. AidStream (n.d.) explains on its website that it is not focused on strengthening the health systems of poor countries, rather its niche work meets the needs of NGOs in this donor-driven data collection reality:
We built AidStream because we could see how complex IATI [International Aid Transparency Initiative] was for organisations without dedicated tech support (which is most of you!). We wanted to help achieve IATI’s goals of making aid data open and transparent, and ultimately, improving outcomes and so we decided to make it as easy as possible for aid organisations to publish that very same data.
The use of parallel data systems abound in data vacuuming, with some being managed exclusively for donor agencies or NGOs, and acting as a quality check to the national health information systems. The US government is one entity that supports parallel data system capture via its partner agencies, both for routine health information and population-level surveys. Data is eventually shared with the host government once the data has been cleaned and synthesized into tables and figures, on the auspices that presenting summary results in a finished format will improve data utilization and evidence-based decision making. However, removing engagement with the data during the cleaning and analysis process effectively diminishes the recipient countries’ agency. Their involvement is fundamentally superficial, making it difficult to eventually transfer back the task. It should be noted that data quality, as defined as availability and reliability across health-system levels, has, in many settings, improved dramatically with these donor supports. However, the actual perceived ownership and use of data for decision making in recipient countries continues to lag (Uthman et al. 2015; Owiredu 2017).
A fundamental paradox related to the development of monitoring and evaluation frameworks exists in these unequal partnerships. As we have discussed, a growing number of indicators are tracked in poor countries, often at the imposition of donor agencies. If the driving force behind the adoption of new, more complex indicators is to introduce audit culture in recipient countries, and deny these countries equal say in their selection, what will drive ministries of health to use these data to inform decision making? Without the express ‘buy-in’ and engagement of government structures, data collection and use is outsourced and becomes a de facto donor activity.
Under this practice, data quality only improves from the point of vacuuming, in other words, from the point of the health-facility report (which then travels to electronic reports at the district, provincial, and national level). However, data quality diminishes at the point of entry, namely in ward registries where data availability and accuracy remain poor (Rowe et al. 2009; Rowe et al. 2007; Hazel et al. 2013). In one large seven-year project in central Mozambique, a foundation supported data quality improvement through improved data literacy and use of frontline and district level managers. As part of the study, primary health care data was assessed annually across twenty-seven health facilities in Sofala Province for availability and reliability between 2009 and 2013.[note 3] Over five years, semiannual meetings were held in each district during which district and facility managers spent three days reviewing and explaining their data to one another. With this simple but targeted audit and feedback intervention, data reliability improved dramatically from 54 to 87 percent overall (see figure 2) (Wagenaar et al. 2015).
What this example highlights is that there is no short cut to improve data quality and use at the health-facility level. Auditing practices such as data vacuuming are destructive because they do not engage health workers. Those who are providing services need to be engaged in the design, selection, collection, analysis, and use of data in order for health services to improve. NGOs, donors, and other stakeholders need to prioritize funding for this grassroots work if they want to move beyond audit logic. Finally, engagement and leadership from ministries of health are required and cannot be outsourced if authentic data systems, fed and used by health workers, and capable of tracking both infectious and non-communicable diseases over time, are to be built and sustained. In large part the success of the project in Sofala Province stemmed from the tremendous leadership of the provincial health director and the monitoring and evaluation team, who spent long days and weekends in remote districts, working with their teams and demonstrating their dedication to improving data quality and use at all levels.
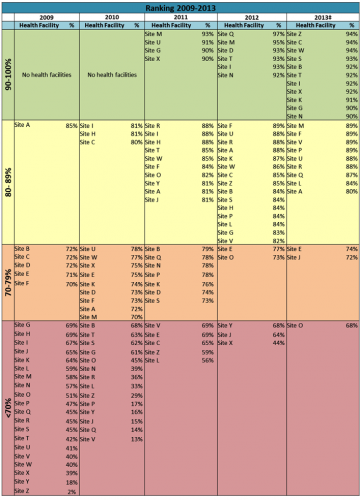 Figure 2. Annual data concordance across twenty-seven health facilities in Sofala Province, 2009–2013 (Gimbel 2016)
Figure 2. Annual data concordance across twenty-seven health facilities in Sofala Province, 2009–2013 (Gimbel 2016)Ministry of health leaders understand that data collected as part of a funding requirement rather than an activity of intrinsic value for health-system strengthening is devoid of meaning to health workers at the frontline. Data vacuuming is an extractive phenomenon that has no relationship to partnership – the egalitarian ideal of collaboration espoused in the Alma Ata Declaration – because unequal power dynamics privilege donor priorities above local ones. This argument exists beyond global health and has been explored in the broader aid field (Bruun Jensen 2013). Ultimately, this lack of true collaboration in the collection of data and its use represents a missed opportunity to jointly build capacity to collect, interpret, and improve data collection, analysis, and application. The Sustainable Development Goals announced in 2015 – and specifically the goal 3.8 to ‘Achieve universal health coverage’ underscores the urgent task of redirecting data gathering and analysis efforts toward local health system strengthening, and challenging the glaring inequalities that currently characterize the data extraction regime by institutions in rich countries (United Nations 2017; Sundewall, Engstrand, and Nordstrom 2018). The increasing sophistication and scale of this vacuuming within the global health space has deepened global disparities and undermined local sovereignty. It is time to turn that sophistication and technology toward building local capacity, strengthening management, and expanding health systems to achieve universal coverage.
About the authors
Sarah Gimbel, PhD, MPH, RN, is Associate Professor in Family Child Nursing and adjunct in Global Health at the University of Washington. She codirects the UW Center for Global Health Nursing and is a technical advisor at Health Alliance International where she specializes in implementation research, focusing on intervention development and testing for strengthening health systems and the evaluation of implementation processes to identify drivers of success.
Baltazar Chilundo, MD, PhD, is Professor in the Faculty of Medicine at the University of Eduardo Mondlane. He has more than fifteen years of experience in the practice and education of public health domains (health systems and community health) of low-income countries. His work focuses on data use and quality, community health workers, HIV/AIDS, malaria, health policy, and primary health care.
Nora Kenworthy, PhD, is Assistant Professor in the School of Nursing and Health Studies at the University of Washington Bothell. Her recent book, Mistreated: The Political Consequences of the Fight Against AIDS in Lesotho (Vanderbilt University Press, 2017), is an examination of the unexpected political costs and missed opportunities for deepening democracy during the global HIV response. Her more recent research examines the industry and emerging cultures of crowdfunding for health care in the United States and abroad.
Celso Inguane is a PhD candidate in sociocultural anthropology at the University of Washington, Seattle. He has broad research interests in medical anthropology and global health, including the politics of knowledge, compliance with biomedical treatment for chronic illnesses, and the strengthening of health systems.
David Citrin, PhD, MPH, is Affiliate Instructor in the departments of Anthropology and Global Health at the University of Washington, where he also codirects the South Asia Center’s Nepal Studies Initiative in the Jackson School of International Studies. He also works as Director of Impact at Possible, a nonprofit organization that partners with the Government of Nepal to strengthen public sector healthcare delivery systems.
Rachel Chapman, PhD, an Associate Professor in the Department of Anthropology at the University of Washington, is a social-cultural applied anthropologist. Her research focus is the political economy of race, gender, and reproduction, especially the impact of transglobal policies on reproductive stratification within and outside the United States.
Kenneth Sherr, PhD, MPH, is Associate Professor of Global Health at the University of Washington, with adjunct appointments in the departments of Epidemiology and Industrial & Systems Engineering. His research focuses on identifying and testing solutions to support service integration into the primary health care framework as a means of improving health system efficiency, coverage, and quality.
James Pfeiffer, PhD, MPH, a medical anthropologist, is a professor in the departments of Global Health and Anthropology at the University of Washington. He is also Executive Director of Health Alliance International, which has programs in Mozambique, Cote d’Ivoire, and Timor Leste. His research examines the intersections between religion, illness, economy, and gender.
References
Adams, Vicanne, ed. 2016. Metrics: What Counts in Global Health. Durham, NC: Duke University Press.
AidStream. n.d. ‘About’. Accessed 6 June 2017. https://aidstream.org/about.
Appadurai, Arjun. 2000. ‘Grassroots Globalization and the Research Imagination’. Public Culture 12 (1): 1–19. https://doi.org/10.1215/08992363-12-1-1.
Arnesen, Trude, and Erik Nord. 1999. ‘The Value of DALY Life: Problems with Ethics and Validity of Disability Adjusted Life Years’. British Medical Journal 319: 1423–25. https://doi.org/10.1136/bmj.319.7222.1423.
Birn, Anne-Emanuelle. 2009. ‘The Stages of International (Global) Health: Histories of Success or Successes of History?’ Global Public Health 4 (1): 50–68. https://www.doi.org/10.1080/17441690802017797.
Brown, Theodore, Marcus Cueto, and Elizabeth Fee. 2006. ‘The World Health Organization and the Transition from “International” to “Global” Public Health’. American Journal of Public Health 96 (1): 62–72. https://doi.org/10.2105%2FAJPH.2004.050831.
Bruun Jensen, Casper, and Brit Ross Winthereik. 2013. Monitoring Movements in Development Aid: Recursive Partnerships and Infrastructures. Cambridge, MA: MIT Press.
Buse, Kent, and Gill Walt. 1997. ‘An Unruly Melange? Coordinating External Resources to the Health Sector: A Review’. Social Science & Medicine 45 (3): 449–63. https://doi.org/10.1016/S0277-9536(96)00365-6.
Carr, Stuart, Ishbel McWha, Malcolm Maclachlan, and Adrian Furnham. 2010. ‘International-local Remuneration Differences across Six Countries: Do They Undermine Poverty Reduction Work?’ International Journal of Psychology 45 (5): 321–40. https://doi.org/10.1080/00207594.2010.491990.
Daschle, Thomas and Bill Frist. 2015. The Case for Strategic Health Diplomacy: A Study of PEPFAR. Washington, DC: Bipartisan Policy Center.
Douglas-Jones, Rachel, and Justin Shaffner. 2018. ‘Capacity Building in Ethnographic Comparison’. The Cambridge Journal of Anthropology 36 (Spring): 1–16.
Farmer, Paul, Jim Yong Kim., Arthur Kleinman, and Matthew Basilico. 2013. ‘Introduction’. In Reimaging Global Health, edited by Paul Farmer, Jim Yong Kim, Arthur Kleinman, and Matthew Basilico, 1–14. Berkeley: University of California Press.
Gimbel, Sarah, Roxanne Hoek, Falume Chale, Catherine Michel, Bradley Wagenaar, Joao Luis Manuel, Lucia Vieira, Elusio Pio, and Kenneth Sherr. 2016. Creating Resilient Country Health Information Systems: A Data Quality Audit Model for Primary Healthcare in Mozambique, 2009–2014. Vancouver: Health Systems Research.
Greenhalgh, Susan. 1996. ‘The Social Construction of Population Science: An Intellectual, Institutional, and Political History of Twentieth-Century Demography’. Comparative Studies in Society and History 38 (2): 26–66.
Hazel, Elizabeth, Jennifer Requejo, Julia David, and Jennifer Bryce. 2013. ‘Measuring Coverage in MNCH: Evaluation of Community-based Treatment of Childhood Illnesses through Household Surveys’. PLoS Medicine10 (5): e1001384. https://doi.org/10.1371/journal.pmed.1001384.
Hoskin, Keith. 1996. ‘The “Awful Idea of Accountability”: Inscribing People into the Measurement of Objects’. In Accountability: Power, Ethos and the Technologies of Managing, edited by Rolland Munor and Jan Mouritsen, 265–82. London: International Thomson Business Press.
Intentional Futures 2015. ‘Global Health Envisioning: Data for Impact’. accessed 4 January 2018. https://intentionalfutures.com/insights/portfolio/global-health/.
Institute for Health Metrics and Evaluation. 2017. Financing Global Health 2016. Seattle, WA: IHME.
Laurie, Emma Whyte. 2014. ‘Who Lives, Who Dies, Who Cares? Valuing Life through the Disability-Adjusted Life Year Measurement’. Transactions 40 (1): 75–87.
Moyo, Dambisa. 2009. Dead Aid: Why Aid Is Not Working and How There Is a Better Way for Africa. New York: Farrar, Strauss, Giroux.
Nichter, Mark. 2008. Global Health: Why Cultural Perceptions, Social Representations and Biolpolitics Matter. Tucson: University of Arizona Press.
Owiredu, Morkor, Nita Bellare, Christine Musanhu, and Taiwo Oyelade. 2017. ‘Building Health System Capacity through Implementation Research: Experience of INSPIREV– Multi-Country Implementation Research Project’. Journal of Acquired Immune Deficiency Syndrome 75 (S2): S240–47.
Packard, Randall. 2016. A History of Global Health: Interventions into the Lives of Other Peoples. Baltimore, MD: Johns Hopkins University Press.
PEPFAR. n.d. ‘About Us’. accessed March 4. https://www.pepfar.gov/about/270968.htm.
PEPFAR. 2009. PEPFAR Next Generation Indicators Reference Guide. Washington, DC: Office of US Global AIDS Coordinator and the Bureau of Public Affairs, US State Department. https://2009-2017.pepfar.gov/documents/organization/206097.pdf.
PEPFAR. 2017a. ‘PEPFAR Funding’. https://www.pepfar.gov/funding/index.htm.
PEPFAR. 2017b. PEPFAR Monitoring, Evaluation and Reporting [MER 2.0] Indicator Reference Guide. Washington, DC: Office of US Global AIDS Coordinator and the Bureau of Public Affairs, US State Department. https://www.pepfar.gov/documents/organization/263233.pdf.
Pfeiffer, James. 2003. ‘International NGOs and Primary Health Care in Mozambique: The Need for a New Model of Collaboration’. Social Science & Medicine. 56 (4): 725–38.
Pfeiffer, James. 2016. ‘Austerity in Africa: Foreign Aid Audit Cultures and Accountability Regimes in the Weakening of Public Sector Health Systems’. Paper presented at the American Anthropological Association, Minneapolis, 16–20 November.
Pfeiffer, James, Wendy Johnson, Meredith Fort, Aaron Shakow, Amy Hagopian, Stephen Gloyd, and Kenneth Gimbel-Sherr. 2008. ‘Strengthening Health Systems in Poor Countries: A Code of Conduct for Nongovernmental Organizations’. American Journal of Public Health 98 (12): 2134–40. https://doi.org/10.2105/AJPH.2007.125989.
Pfeiffer, James, Pablo Montoya, Joao Baptista, Marina Karagianis, Marilia Pugas, Mark Micek, Wendy Johnson, Kenneth Sherr, Sarah Gimbel, Shelagh Baird, Barrot Lambdin, and Stephen Gloyd. 2010. ‘Integration of HIV/AIDS Services into African Primary Health Care: Lessons Learned for Health System Strengthening in Mozambique – A Case Study’. Journal of the International AIDS Society 13 (3). https://doi.org/10.1186/1758-2652-13-3.
Power, Michael. 1994. The Audit Explosion. London: White Dove Press.
Power, Michael. 1997. The Audit Society. London: Oxford University Press.
Redfield, Peter. 2012. ‘The Unbearable Lightness of Expats: Double Binds of Humanitarian Mobility’. Cultural Anthropology 27 (2): 358–82.
Requejo, Jennifer, Cesar Victora, Jennifer Bryce. 2015. Countdown to 2015: A Decade of Tracking Progress for Maternal, Newborn and Child Survival. Washington, DC: UNICEF and WHO.
Rowe, Alexander, S. Patrick Kachur, Steven Yoon, Matthew Lynch, Laurence Slutsker, and Richard Steketee. 2009. ‘Caution Is Required When Using Health Facility-Based Data to Evaluate the Health Impact of Malaria Control Efforts in Africa’. Malaria Journal 8: 209. https://doi.org/10.1186/1475-2875-8-209.
Rowe, Alexander, Richard Steketee, Fred Arnold, Tessa Wardlaw, Suprotik Basu, Nathan Bakyaita, Marcel Lama, Carla Winston, Matthew Lynch, Richard Cibulskis, Kenji Shibuya, Amy Ratcliffe, and Bernard Nahlen, Monitoring Roll Back Malaria, and Group Evaluation Reference. 2007. ‘Viewpoint: Evaluating the Impact of Malaria Control Efforts on Mortality in sub-Saharan Africa’. Tropical Medicine & International Health 12 (12): 1524–39. https://doi.org/10.1111/j.1365-3156.2007.01961.x.
Sherr, Kenneth, Abdul Mussa, Baltazar Chilundo, Sarah Gimbel, James Pfeiffer, Amy Hagopian, and Stephen Gloyd. 2012. ‘Brain Drain and Health Workforce Distortions in Mozambique’. PLoS One 7 (4): e35840. https://doi.org/10.1371/journal.pone.0035840.
Shore, Cris and Susan Wright. 2015. ‘Governing by the Numbers: Audit Culture, Rankings and the New World Order’. Social Anthropology 23 (1): 22–28.
Smith, Daniel Jordan. 2007. A Culture of Corruption. Princeton, NJ: Princeton University Press.
Stanford, Victoria. 2015. ‘Aid Dependency: The Damage of Donation’. This Week in Global Health. https://www.twigh.org/twigh-blog-archives/2015/7/31/aid-dependency-the-damage-of-donation.
Storeng, Katerini, and Dominique Behague. 2014. ‘“Playing the Numbers Game”: Evidence-Based Advocacy and the Technocratic Narrowing of the Safe Motherhood Initiative’. Medical Anthropology Quarterly 28 (2): 260–79. https://doi.org/10.1111/maq.12072.
Strathern, Marilyn. 2000. ‘New Accountabilities’. In Audit Cultures: Anthropological Studies in Accountability, Ethics and the Academy, edited by Marilyn Strathern, 1–18. Oxon, UK: Routledge.
Sundewall, Jesper, Pia Engstrand, and Anders Nordstrom. 2018. ‘Swedish Development Assistance for Health: Critical Questions to Ask Going Forward’. Lancet Global Health 6 (3): e242–43. https://doi.org/10.1016/S2214-109X(18)30037-8.
United Nations. 2017. ‘Sustainable Development Knowledge Platform’, accessed 1 January. https://sustainabledevelopment.un.org.
Uthman, Olalekan, Charles Shey, Wiysonge, Martin Ota, Mark Nicol, Bongani Mayosi. 2015. ‘Increasing the Value of Health Research in the WHO African Region beyond 2015–Reflecting on the Past, Celebrating the Present and Building the Future: A Bibliometric Analysis’. British Medical Journal Open 5 (3): e006340. https://doi.org/10.1136/bmjopen-2014-006340.
Vanian, Jonathan. 2016. ‘Why Data Is the New Oil’. Fortune,12 July.
Wagenaar, Bradley, Sarah Gimbel, Roxanne Hoek, James Pfeiffer, Catherine Michel, Joao Luis Manuel, Fatima Cuembelo, Titos Quembo, Pires Alfonso, Victoria Porthe, Stephen Gloyd, and Kenneth Sherr. 2015. ‘Effects of a Health Information System Data Quality Intervention on concordance in Mozambique: Time-Series Analyses from 2009–2012’. Population Health Metrics 13: 9. https://doi.org/10.1186/s12963-015-0043-3.
Whyte, Susan, Whyte, Michael. 2013. ‘Therapeutic Clientship: Belonging in Uganda’s Mosaic of AIDS Projects’. In When People Come First: Critical Studies in Global Health, edited by Joao Biehl and Adriana Petryna, 140–65. Princeton, NJ: Princeton University.
World Health Organization. 1978. ‘Declaration of Alma Ata’. http://www.who.int/publications/almaata_declaration_en.pdf.
World Health Organization. 2017. ‘Metrics: Disability Adjusted Life Years’. http://www.who.int/healthinfo/global_burden_disease/metrics_daly/en/.
World Health Organization Maximizing Positive Synergies Collaborative Group. 2009. ‘An Assessment of Interactions between Global Health Initiatives and Country Health Systems’. Lancet 373: (9681) 2137–69.
Endnotes
1 Back
We use the term global health ‘techies’ to refer to individuals who previously worked in computers, software, and related technologies and have now moved their efforts to global health. Often times these individuals bring language and paradigms from their former field.
2 Back
Countdown to 2015 was a World Health Organization-sponsored ten-year initiative established in 2005 to stimulate country action by setting and tracking coverage for interventions needed to attain Millennium Development Goals 4 and 5, and, in addition, parts of Millennium Development Goals 1, 6, and 7. See also http://www.un.org/millenniumgoals/.
3 Back
The indicators collected included the number of institutional births, number of first antenatal care visits, number of outpatient visits, and the number of third diphtheria, tetanus toxoids, whole-cell pertussis, hepatitis B, haemophilus influenzae type b (DTP-HepB-Hib) vaccines (note these vaccines are administered as a single pentavalent vaccine) administered by health facility. Concordance of these four indicators was assessed over twelve months across four levels of the health system, using health facility ward registries, health facility paper reports, and electronic reports at the district and provincial levels. We calculated the concordance of data between various data collection instruments. Afterwards, we ranked the facilities from highest to lowest data concordance between 2009 and 2013. For example, in 2013, health facility ‘Z’ had the highest data concordance and health facility ‘O’ had the lowest as noted in the table.