Dealing with highly contagious animal diseases under neoliberal governmentality in Mongolia
—
Abstract
Mongolia is a postcommunist country with fifty-two million animals and more than three million humans, as of 2014.[note 1] One-third of its economic production comes from herding. Under the auspices of the World Organization of Animal Health since 1989, and because of its location between Russia and China and its nomadic traditions, Mongolia is at the heart of global policies regarding the spread of animal diseases (specifically transboundary animal diseases and zoonoses) and concerning the involvement of herders in the surveillance of animals. Human-animal relations in Mongolia are diverse and present different risk factors for the spread of pathogens: there is continuous contact between nomadic herders and domestic herds, between occasional hunters and wild animals, and between domestic and wild animals. The large territory (two-and-one-half times larger than France) is crossed by human and animal movements over a wide area: nomadic migrations, seasonal migrations, and seasonal legal and illegal hunting periods.
I present here the results of ethnographic research conducted in two provinces of Mongolia during the winters and summers of 2014 and 2015. In Ulaanbaatar, I conducted semistructured interviews with political leaders from the Ministry of Agriculture, with the director of the National Veterinary Agency, with former herders who had lost their entire herds following the occurrence of an outbreak or a natural disaster (such as extreme cold or extreme drought), and with nine former herders’ families. In Hentii and Töv provinces, I met thirty nomadic herding families in the steppe who generally practiced an extensive type of herding characterized by low densities of animals per hectare. Such nomadization provides new pastures for herds and allows for a better preservation of the soil.
I studied the management and the surveillance of three animal diseases that were controlled under the Communist government but which have since chronically re-emerged, developed, and spread in different ways over the vast Mongolian territory for two decades: brucellosis (a bacterial disease, endemic and widespread, zoonotic), anthrax (bacterial, localized, zoonotic) and foot-and-mouth disease (viral, localized and pandemic, nonzoonotic) (Ruhlmann 2015b). I chose these three animal diseases because they are different in terms of their nature (bacterial or viral), their mode of propagation and contamination (through contact with soil, faecal substances, blood, or saliva; through ingestion of meat or milk; and through inhalation of air), and their dangerousness for human health or life (nonzoonotic or zoonotic diseases). I wanted to understand if these differences determined, among political leaders and herders, different treatment practices for animal and human populations according to whether they were infected (or suspected of being so) or not.
These three animal diseases are the most important diseases affecting the country, the economy,[note 2] the ecosystem, the animal populations (domestic and wild), and the human populations (nomadic and sedentary) in the eyes of various actors: politicians, private veterinarians, scientists, nongovernmental organizations, and pastoralists. Starting from the role of each of these actors in the ‘surveillance’ of animal diseases and in the ‘control’ of infected animals, and starting from the definition of these two concepts, I discuss how the government includes herders in a form of ‘syndromic surveillance’, defined by expert epidemiologists as a ‘surveillance system that collects and analyses nonspecific health indicators [of a population][note 3] in an automated manner and in almost real-time’, which is also associated with an epidemiological information system,to ensure early detection and rapid response(Perrin et al. 2011, 9; my translation). This article therefore begins by describing how herders are involved in the new governmental policy to surveil animals and pathogens, placed at the forefront of a distributed vigilance.[note 4] This article then focuses on the various medicinal treatments that herders deploy in correlation with animal diseases, in particular, in terms of the conception of illness and misfortune in general. It considers the mobilization of two kinds of local knowledge, inherited from Tibetan Buddhism and shamanism; details the use of substances and medicines, technical gestures, and propitiatory, apotropaic, or curative pronounced formulas; and describes the variety of strategies used to circumvent official veterinary medicine without contradicting the international system of laws regarding animal health. I seek to show that traditional local medicine works with the economic and social situation of herder families, as a preferential or complementary medicine that, if it is not effective, does not hinder official care, and that it responds as well to larger economic and political stakes. In conclusion, this article draws out how herders make different systems – shamanism, Buddhism, postcommunism, liberalism, neoliberalism – compatible with one another because, even under the control of government policy, they perfectly identify and respect their own interests while following or skilfully subverting some measures of state regulation.
Sixteen years ago, in an eastern quarantine area
At the end of the winter of 2001, I was detained in the countryside, at the camp of a nomadic herder family, because of a foot-and-mouth outbreak that had occurred in the four eastern provinces (see map below). At this time during my first nine months of stay in Mongolia, I could not understand that I was ‘in quarantine’ (karantin, borrowed from Russian; horio tseer, in Mongolian) because of an animal disease. Indeed, when such an event occurs, Mongolian families do not speak about it: they fear that misfortune – and the pollution it entails and represents – will spread. One day I saw a dead horse abandoned, lying on the ground, and I could feel that something unusual and unmentionable had happened but I could not identify exactly what. The eldest woman of the camp told me ‘the horse is sleeping’ – another way to express the tabooed words ‘it is dead’ – and she followed with, ‘but do not approach it! It’s nasty!’ – meaning that it could be dangerous or risky. Her daughter hastened to specify: ‘It is tainted!’ (haldvartai).
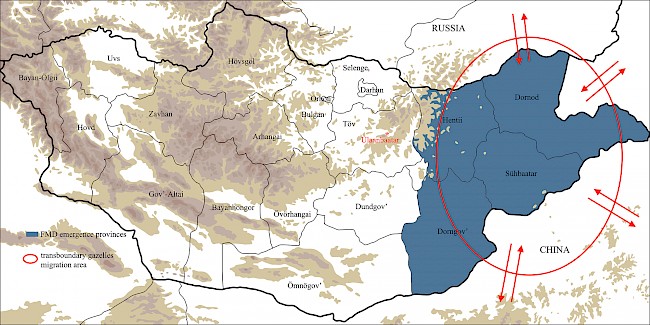 Caption: Area of foot-and-mouth disease emergence and gazelles’ transboundary migration patterns (2000–2014). © Map by Marc Alaux; annotations by Sandrine Ruhlmann based on information obtained during interview with director of National Veterinary Agency (Ulaanbaatar, winter 2014).
Caption: Area of foot-and-mouth disease emergence and gazelles’ transboundary migration patterns (2000–2014). © Map by Marc Alaux; annotations by Sandrine Ruhlmann based on information obtained during interview with director of National Veterinary Agency (Ulaanbaatar, winter 2014).Ten days after this event, I was allowed to take an overnight Jeep to the urban centre of Öndörhaan, where the family of the daughter’s future husband lived. The family was tense and I asked the mistress of the household if something had been improperly done, which could cause an illness. ‘Of course, no!’ she whispered. The next day, she sent me to the military office where I could ask to be permitted to return to Ulaanbaatar city, but she did not explain to me why I could not just go back to Ulaanbaatar directly. ‘Impossible for the moment: karantin’, the sergeant said, which, even if I did not understand everything, made me all the more worried because my visa would expire in four weeks. I went back to the military office every morning for twenty-five days, traveling from the other side of town by foot in minus forty-degree Celsius weather, and each morning he told me to come back the next day. Finally, one day the military authorities allowed me to leave on a flight that was taking about twenty seriously ill hospital patients to the central hospital of Ulaanbaatar.
They did not tell me anything besides the word ‘karantin’, a word that I did not at first understand because I did not make any connection between it and the similar French, English, or Russian words. The context of silence and taboo did not help my understanding. When I finally made the connection, I could not find out what kind of quarantine had occurred. Was there any danger? No one in the family and the neighbourhood would reveal anything to me, and none of these families had televisions or bought any daily newspapers that could inform me. Finally, early in the morning, while on the road to the provincial airport, from where we would fly to Ulaanbaatar city, I saw many cattle carcasses along the way. Before boarding the plane to Ulaanbaatar, another passenger and I had to wait for a long time outside, at dawn, in the wintry cold, and then inside a large building near the airport. Inside, despite the cold, we had to remove our coats, scarves, and hats, and leave our bags in a room where they were gassed, after which we were moved next door to be gassed in another airtight room. Later, the French ambassador explained to me that the aim of these procedures was for us to inhale a disinfectant gas, literally ‘decontaminant gas’ (ariutgalagch hii), commonly called ‘fog’ (manan). During a subsequent visit, more than ten years later, the director of the National Veterinary Agency confirmed that ‘the fog has to disinfect the inside [of the body]’ (manan dotor ariutgah yostoi) (Ulaanbaatar, winter 2014). When the quarantine ended, everything ‘had to be decontaminated: a person’s objects, hair, shoes, hands, face, and also the air they breathed were decontaminated with a sterilizing disinfectant product’ (ariutgalyn bodisoor ariutgah spirt) (director of the National Veterinary Agency, Ulaanbaatar, winter 2014). So, we executed the military orders without questions, without uttering a single word: we inhaled the gas for thirty minutes, while our bags were also gassed. Following the others, I held my tongue, memorizing the slightest gestures of each of the other passengers. One after another, standing in line in the corridor toward the exit, we had to take with our right hand a tray with a small cotton ball bathed in a liquid mixture of milk and alcohol named ‘spirt’ and ‘wash’ (ugah) our hands with it, then apply the liquid to our hands and faces to ‘purify’ (ariutgah) them. And then, a few metres further, we had to take a sugar cube resting on a tray and soak it in a bowl filled with the same ‘disinfectant’ (ariutgagch bodis) and chew, then eat, the soaked piece of sugar to ‘wash’ or ‘purify’ the insides of our bodies. At the end of these procedures, prior to boarding the airplane, we had to walk on a tray filled with a prophylactic powdered lime (shohoi) to finish the disinfection of our shoes. In the airplane, which seemed to be rather poorly constructed, everyone was holding someone on their knees, the plane having a capacity considerably less than the number of passengers. As not all the seats were fixed to the floor, the scared old woman sitting by my side prayed throughout the flight, reciting Buddhist blessing formulas and manipulating her rosary beads as we were gassed again.
Thirteen years later, when I started to study the management of animal diseases in Mongolia, I found that the measures had not changed: quarantine for forty days; partial vaccination of herds; culling of infected or suspected animals; and disinfection of humans, livestock enclosure areas, tools, soil, and vehicles. During interviews conducted from January to March 2014, the director of the National Veterinary Agency confirmed all these ‘measures of extremely contagious animal diseases control’. He was proud of the determination of the military forces and of the perfect execution of ‘decontamination’ (haldvarzüizhüülelt) – in order to be no longer contagious – and ‘disinfection’ (ariutgal) – in order to be no longer impure – both of which are required for exiting the quarantine area during and after an outbreak.
From surveillance to control measures
Two techniques for monitoring animal diseases can be deployed at different moments: surveillance and control. Surveillance may either be permanent and included in public health programs: this is a priori vigilance, such as the vaccination of an entire herd. Or it may be implemented at the onset of the first symptoms or the first case of disease among animal or human populations: this is a posteriori vigilance, such as medicating or vaccinating an infected or noninfected herd. Sometimes, surveillance is urgently implemented when an epidemic has already spread and wreaked havoc, and culling is the only way to prevent wider contamination and stop the outbreak. But eradication is not the solution for preventing the next outbreak. In a priori vigilance, veterinarians and/or herders prevent diseases and anticipate threats, while in a posteriori vigilance they cure and face them. These two types of vigilance are complementary in the system of surveillance (Chateauraynaud and Torny 1999).
In the case of an outbreak of a highly contagious disease, treatments must be combined (medication, vaccination, culling), which is financially and psychologically costlier for both the government and the herders (Zinsstag et al. 2007). This kind of long-term and sustained monitoring that some governments establish, particularly through the use of ‘sentinel animals’, which are considered early warning signals (Keck 2010), develops a ‘generalized vigilance’ (Chateauraynaud and Torny 1999). Compared with surveillance, control is a more radical and massive intervention. It generally involves culling thousands of animals that are infected or suspected of being infected. A government implements a system of ‘disease surveillance’ to track the emergence of symptoms among the people who live in daily contact with domestic animals – herders – whereas it imposes a system of ‘animal control’ to intervene in the lives of animals to end the outbreak.
The two strategies[note 5] – surveillance and control, or in most situations vaccination and culling – are differently considered: the first one is technically unrealizable for complete efficiency and durability in both the short and the long term, but it respects (or does not contradict) natural processes and is generally accepted; the second one is financially costly and morally unacceptable, because it involves extensive state control. Adopting the radical measure of culling combined with partial and random vaccination in crisis situations, the latest solution adopted by the current Mongolian government leads to daily and extensive surveillance by herders who act as sentinels, veterinarians who act as transmitters of information, and NGOs who act as mediators of surveillance (Ruhlmann 2015b).[note 6] In this new form of public health care, the government mobilizes collective action and distributes roles among different actors at different scales, to implement a global security system called ‘biosecurity’ (Collier, Lakoff, and Rabinow 2004; Fallon et al. 2012). Applied to different threats (natural disasters, terrorism, pandemics), this system aims at preventing pathogens from crossing species boundaries, an alarming phenomenon that has preoccupied the World Health Organization and the World Organization for Animal Health since the panzootic of avian influenza in 2005. I propose that this new, contemporary governance be described as neoliberal. By Mongolian neoliberal governance, I mean a development or an attempt to develop indirect techniques of population control (human and animal) in parallel with direct state intervention, according to the terms of Foucault (1994; see also Lemke 2004). Thus, since the end of the twentieth century and the beginning of the twenty-first, the Mongolian government has been using – in addition to its own agents, the state veterinarians – new nongovernmental actors, such as herders and NGOs (which have their own veterinarians), and giving them responsibility for the management of animal diseases, in a constant manner and not only in crisis situations. It is a form of neoliberal governmentality that consists of political strategies to shift responsibility: herders, in other words, families, and to a lesser extent NGOs, become responsible actors within a framework of distributed roles and responsibilities. This delegation to the bottom local level is a kind of neoliberal monitoring and governance.
When a new disease emerges, or an old one re-emerges, some governments urgently adopt different measures for the control of animals, combining sanitary culling and vaccination of herds, such as the British government did when confronted with foot-and-mouth disease (Woods 2004). States work to transform a danger or threat into a measurable and controllable risk with the aim of reducing uncertainties; such means of surveillance and control thus enact a particular form of governmentality, or art of government (Foucault 2004, 111–12; see also Chateauraynaud and Torny 1999; Stirling 2007; Prete 2008; Fish et al. 2011; Giles-Vernick, Traoré, and Bainilago 2015).[note 7] According to Clavendier (2006, 23), vigilance is ‘an avatar’ of the ‘culture of risk’, a concrete way of taking part in this logic of ‘enlightened protection, that is to say conscious, responsible and excepting tangible effect’. The study of governmentality concerning animal diseases in Mongolia seeks to analyse the systems of security, surveillance, and control that are the main contemporary tools and strategies of the Mongolian government in establishing and exerting power over human and animal populations.[note 8]
The Mongolian government has demonstrated its desire to be a member country of the World Organization for Animal Health and its willingness to respect international regulations: it strengthened the animal health system to eradicate foot-and-mouth disease and brucellosis, and it promoted the safeguarding of nomadic herding, improving the rural economy and also foreign trade. More recently, it has also given an active role and responsibility to herders, implementing a contemporary surveillance device that is a combination of a priori and a posteriori vigilance, using herders as ‘responsible sentinels’ (hariutslagatai haruul) and ‘daily observers’ (ödör tutmyn azhiglagch), and placing veterinarians ‘at the head of operations’ (üil azhillagaany tergüün) in case of outbreak and designating them as ‘transmitters of information’ to the central health security cabinet of the government (director of the National Veterinary Agency, Ulaanbaatar, winter 2014). This network of observers, with their distributed responsibilities, has recently been established in a nomadic herding country, and can thus be considered a real-time laboratory for the study of a new way to govern animal diseases. Given this case, I suggest that nomadic herding, by inducing contact between nomadic domestic animals and free migrating wild animals, could make an accelerated entry into the path of the global liberal economy.
Legally, the Mongolian Constitution (1992) states that ‘the livestock of the country is a national wealth and subject to state protection’ and the strategy of Mongolia for the control of animal diseases is based on the ‘law of protection of animal health and genetic pool’, ‘animal and plant quarantine’, and ‘civil protection’. Certain regulations are enforced by the Veterinary and Animal Breeding Agency (VABA), the Government Agency for Specialized Inspection (GASI), and the National Emergency Management Agency (NEMA), such as control procedures of transboundary animal diseases, quarantine, and the movement of animals and animal products. Foot-and-mouth disease outbreaks were recorded in the years 1931–1935, 1941–1948, 1963–1974 and, after twenty-six years of absence, in the years 2000–2002, 2004–2006, 2010, 2013 (Basan, Purevkhuu, and Togoonyam 2013), and 2014–2017 (see the World Animal Health Information System [WAHIS Interface, n.d.] on the website of the World Organization for Animal Health).[note 9] As the director of the National Veterinary Agency told me during the winter of 2014, ‘the disease-reporting system is mandatory for all veterinary staff and livestock owners’. He explained that ‘the first observation of suspected cases is made by herders’, who ‘have to report suspect things in their herd to the veterinarian of the district who is responsible to transmit the information to the central health security cabinet in Ulaanbaatar’. This obligation is registered in article 14.1.5 of the law on ‘animal health and gene protection’ (Basan et al. 2013) and the State Veterinary Services has the obligation to report any outbreak of highly contagious animal diseases within twenty-four hours to the World Organization for Animal Health. But how do herders cope with international and national measures while facing the reality of animal diseases?
Herders as sentinels: The mobilization of local knowledge and know-how
The surveillance of highly contagious animal diseases, viral or bacterial, zoonotic or nonzoonotic, is based nowadays on the ongoing attention of herders. Living in daily contact with their herd, similar to before the Communist collectivization of pastures and herds, nomadic herders today directly care for the health of their animals. But today, they have to perform the new function of sentinels in animal health policy, in tandem with veterinarians who play the role of information transmitters. Abigail Woods (2004) noticed that in 2000 in the United Kingdom, the surveillance policy for foot-and-mouth disease was based on a similar role distribution. In Mongolia, being a ‘responsible sentinel’ (hariutslagatai haruul) involves daily observation based on local knowledge and know-how passed down from generation to generation, which is then combined with a professional veterinary practice that has been inherited from occidental veterinary medicine (veterinarians trained in Moscow during the Communist period, and more recently in European countries and in Mongolia). This local expertise is a combination of folk medicine and formal medicine, with the folk medicine having been borrowed from neighbouring countries, specifically via Tibet from India since the fourteenth century (Bawden 1958, 1961, 1962a, 1962b; Humphrey 1984; Meserve 1993, 1996, 2003).
According to Bawden (1961, 1962b), the folk cure for humans and animals concerns two types of treatments: physical treatments, reserved for disease, and magical rites and remedies, used for many kinds of misfortune including sickness. Two local medicines coexist today among Mongols: a popular medicine closely linked to shamanic curative practices and provided by shamans in some centres in Ulaanbaatar and in the countryside (this method integrates, and has integrated in the past, Buddhist elements); and a more formal medicine derived from the Tibetan tradition, provided by monks in monasteries, who integrated shamanic elements to establish themselves with the Mongolian people. Herders generally do not call a monk or a shaman to come cure sick animals. But when they go to the district centre to ask a veterinarian to diagnose their herd, some also consult a monk in a monastery and/or a shaman. Herders return to their camp with the veterinarian – or bring to the clinic one or two sick animals if they must be operated on – or with treatments and/or recommendations given by the veterinarian and possibly by a monk and/or a shaman. One herder explained that ‘monks and shamans never need to come to the camp to cure sick animals’ because herders can ‘name the disease or describe the symptoms, then the monk reads prayers, divines, and seeks the causes of the disease, or the shaman makes a ritual of reparation to repair, cure, and purify, and they both know what to ask the herder to do when returning to his camp’ (Hentii, summer 2014). Herders pay the veterinarian (in cash), monk (in cash), and/or the shaman (cash, food, or other substitute for money), but they also know what to do themselves. Another herder told me, ‘We know what to give to drink, what to apply to their hair, on the body, what to do depending on where it hurts, because we look at the animals’ behaviour, we know their ordinary behaviour, and it’s easy to see where it hurts’ (Töv, summer 2014). Herders have ‘treatments for external or internal diseases, skin or hair diseases or head, throat, stomach, liver, heart diseases’ (herder, Hentii, summer 2014). They are skilled in treating a variety of bacterial, viral, and parasitic diseases because they all have ‘seen how their parents and grandparents did’ such treatments. According to one herder, the consultations of the monk and the shaman are simply ‘supplementary ways to eradicate the disease’ (Hentii, summer 2015) that add formulas, purifications, and other ingredients to public health interventions.
Herders deploy multiple kinds of treatments simultaneously and without prioritizing any of them. But in language and in practice, when they administer medicines (em), help a veterinarian inject a vaccine (em), or provide a medicinal remedy (em) or a remedy of conjuration-protection (dom), they make ritual gestures and pronounce ‘conjuring-protective formulas such as “em dom, em dom, em dom” that repair [zasah], purify [ariutgah], cure [emneh domnoh], and send away the disease and misfortune’ (herder, Hentii, July 2014).[note 10] After pronouncing conjuration-protective formulas, some herders then sometimes ‘call happiness, prosperity, and fortune’, by whispering the propitiatory formulas ‘om man’ padme hum’ or ‘hurai, hurai, hurai!’
Some healing methods are used with both humans and animals, and with other popular medicines, such as bloodletting and the use of poultices. These curative practices are used for different diseases, such as anthrax, rabies, foot-and-mouth disease, and scabies (Chagdarsürüng 1980; Humphrey 1984; Meserve 1996). It seems that physical treatments (em) are reserved for diseases and protection treatments (dom) for misfortune, but the two types of treatments are generally conjoined. Nowadays they may precede or follow veterinary treatments (medicines, vaccine, surgery), and are preferably deployed first if the disease is in its early stages.
Those both physical and protective treatments fall under a set of technical gestures of surgical procedures and medicinal remedies enumerated and described by several herders in Hentii and Töv provinces (winter 2014, summer 2014 and summer 2015):[note 11]
(1) to soak with or to apply (shavah) urine, rancid butter, hot milk, or mud ‘to cure arthritis, arthrosis and lumbago’;
(2) to wrap (booh) with a bandage (boolt, oroolt), ‘to envelop with warm food or fabrics to bring down a fever’;
(3) to rub down(tsorgih) with a warm copper or silver object or a mixture of tea and salt ‘to treat inflammation’;
(4) to scratch (maazhih) with a fabric soaked with an infusion of bitter plants or with fermented mare’s milk ‘to treat purulent pimples or udder diseases’, or with warm sand ‘to cure nerve diseases’, or with dung ashes ‘to treat parasites’;
(5) to cauterize (töönöh) by applying a warm poultice (töönüür) containing one of many substances: crumbled dried cow or sheep dung, tobacco, or dung ash, ‘that disinfect’; medicinal plants and tea; hot water and soot; hot salt; buttermilk and/or butter and soot; a hot porridge of dairy products; or a mud cataplasm, ‘applied on a wound with stink or blood’ or ‘on a swollen or painful limb’;
(6) to press (darah) ‘to get out the stink or a worm’;
(7) to induce bloodletting/bleeding (hatgah) with a hot ‘thorn’ (hatguur), such as needle, awl, or knife, ‘to cure fever, liver diseases or limping’ or ‘to heal the whirling disease’ (called ergüü meaning literally ‘idiot, inconsistent’). The veterinarian of an NGO also mentioned ‘bloodletting with leeches’ (hanuur horhoitai hanalga) ‘to cure the head, heart, liver, and kidneys’;
(8) to force the swallowing (zalgih) of a warm infusion (hand) ‘to cure a flu or a sore throat’; the infusion may be made of dung ashes (argalyn üns) and of medicinal plants (emiin urgamal), such as wild yellow leek, but also warm urine or hot milk, hot fermented or distilled yoghurt, or any dairy product;
(9) to penetrate (örömdöh) consisting of putting ‘a curative substance such as salt or butter in the nostrils or the mouth, or ashes in a pierced limb such as hoof, ‘to disinfect or purify a wound’ or ‘to help wound healing’;
(10) to fumigate or smoke (utah) with the smoke (utaa) of medicinal plants ‘to cure cough, cold or flu’, with dried dung (argalyn utaa) ‘when an animal is too thin’;
(11) to scare (ürgeeh) spirits ‘to simultaneously remove evil spirits and cure the disease’ by shouting or firing a shot with a shotgun;
(12) to make a libation (tsatsah) ‘to purify pollution and to beckon happiness’ ;
(13) to make offerings (to give; ögöh) ‘to satisfy good spirits, to make merit [meritorious actions] and to beckon happiness’.
Herders and veterinarians have indicated that most of these treatments are used in both animal and human medicines.
The treatment of the whirling disease (ergüü) affecting goats is an example of the combination of em and dom practices. A herder in Hentii recounted how this is done:
When affected, goats behave like drunk men, turning themselves around. A competent herder or a veterinarian has to make a notch behind the head … at the base of the head, to remove the cyst before it becomes too hard … To cauterize the wound, he has to make a warm poultice of black tea, rancid butter, and dried crumbled cheese and to wrap the limb to maintain the poultice. He has to make a new warm poultice several times until goats are healed. Then he must purify the animals, the enclosures, sometimes the tools, and of course himself, with a fumigation of juniper incense, not the smoke of dried dung but of juniper, [which is among other things] an antiseptic plant, repeating each time three times ‘em dom, em dom, em dom’. It is better to do it after [treating the wound], but all herders do not always do it, but I prefer doing it to be surer the disease goes far away. (summer 2014)
Another herder, also in Hentii, gave an example of how to treat ‘parasites under the skin’:
Sometimes, in the fall, fattened cattle have insect larvae beneath the skin, on the vertebral column. We see larvae because they make small bumps on the back. They never penetrate the flesh, they are under the skin. So, we press the skin to remove larvae, then apply a Russian disinfectant and healing cream, or a warm horse fat, or a warm cataplasm made of rancid butter and acid yogurt. Then we purify the animal by turning all around the body, the head or the trouble with the smoke of medicinal plants, generally juniper placed on dried burning dung, or by placing a branch, stems, or leaves of a plant on all parts of the animal body, while repeating three times ‘em dom, em dom, em dom’. The smoke cures because it is breathed, and it purifies and makes the illness go. (summer 2014)
A herder in Hentii explained that herders ‘don’t make any specific food offerings or milk libations because they offer some food to the monastery if needed and because they dedicate one libation with milk each morning to the spirits of nature [gazryn ezed], except in the case of serious or contagious diseases’ (summer 2015). The entities gazryn ezed, or hangai delhii, to which some herders petition, are the spirits of nature, such as mountains, rivers, and lakes. The same herder continued, saying that, in the case of highly contagious diseases, they ‘ask to hangai delhii to remove the disease from the herd and family and they make food offerings and libations by the sick animal’s body and all around the enclosure and the camp to call happiness… . And when they hear that a disease has emerged near the camp, they ask that the disease doesn’t come to them and their herd, [that it] stops there, far away’ (summer 2015).
Comparing herders’ practices related to diseases such as pest, plague, scabies, anthrax, foot-and-mouth disease, and pox, and diverse ailments such as eruptions, swelling, limping, cysts, tumours, etc., I noticed that herders used almost indifferently a variety of substances, separately, successively, or simultaneously, to cure different diseases, to disinfect and cicatrize affected limbs, and to purify or remove the illness. These included, but were not limited to, tea, urine, rancid or bitter fermented dairy products, distilled dairy products, flour of wheat or millet, meat or bone broth,[note 12] and wild plants,[note 13] and more rarely salt, sodium, sulphur, sand, silt, rifle powder, dried dung ashes or smoke, tobacco, soot, burnt bone smoke, sometimes even car exhaust, metal (copper, silver, brass), and tar.
According to Ruth Meserve’s (1996) study of manuscripts on traditional veterinary medicine and nomadic herders’ understanding of and attitude toward disease, external observation is used to identify the majority of disease symptoms and make diagnoses, but descriptions of internal diseases are vague, with the exception of stomach aches and intestinal problems. It seems that infectious diseases were less understood in the past and most often treated by conjuration treatments (dom)[note 14] (Meserve 1996, 336).
In fact, some herders ‘make dom’ (dom hiih) apart from any therapeutic procedure (em) to protect their herds from various external threats, such as attacks by wolves and/or diseases carried by wolves or foxes such as rabies. And some of them describe practices that do not concern a disease at all: while some dom or em dom cure (domnoh, emneh domnoh), others protect (hamgalah). For example, herders tie a thread around (booh) a fire clamp or sewing scissors, or they thread a rib bone to a radius or ulna bone to create the feeling that a man is overseeing the camp and pointing his shotgun, or they place a small amount of earth on top of the enclosure’s posts ‘to protect the herd from wild dogs, wolves or foxes that could eat them or give them rabies and to protect family from bad things [muu züil]’ (herder, Töv, winter 2014). In the same way, to protect family and herd from ‘the devil, evil things or evil tongues’, herders fasten two saws together to form a frightening open mouth, so that the ‘teeth of the saws frighten the evil spirits’ (herder, Hentii, winter 2014). When the herd spends the night in the pasture, the herders put in a glass that is placed upside down on a piece of furniture a number of sheep droppings equal to the number of animals in the herd, so that the herd is protected. Thus, ‘nothing bad will come to them [animals], the wolves for example, [and] they [animals] will not get lost and will return to the camp’ (herder, Hentii, summer 2015). During the night of the ‘closing day’ (bitüünii ödör) [of the year], the eldest man of the camp must fire his gun once into the air to ‘remove misfortune and diseases’ (herder, Hentii, summer 2015), and to prevent humans or animals from getting sick.
Nomadic herders’ conception of diseases and the emergence of pathogens
In Mongolia, misfortune (dispersal of fortune, zolgüi, zovlon) occurs after someone has done something bad or in the wrong way, such as having a bad thought or saying bad words against someone, wishing someone harm, burying the dead in the wrong manner, or other acts like exiting the yurt in the opposite direction of circulation or striking the threshold of the door. More recently, accumulating too much wealth (via intensive exploitation of the subsoil, or extraction of oil, gas, copper, gold, or coal by major foreign industrial groups) has been added to the list of causes of misfortune. It is as misfortune and/or as pollution that many Mongolian families view natural disasters or catastrophes, and illness or death of humans or animals (Empson 2012; Ruhlmann 2015a). Misfortune involves the action of spirits grouped under the generic expression of ‘bad spirits’ (muu süns). There are different angry or avenging spirits, such as masters of the land (gazryn ezed) who populate the landscape and become angry because of the bad actions of humans. Evil spirits (ad, ad chötgör, albin, albin chötgör), and souls of the dead that were not reborn, sometimes simply called ‘souls’(süns), more specifically called ‘bad souls’ (muu süns), ‘wandering souls’ (hergiin süns), or ‘starving souls’ (ölön süns), are frustrated and wander near their family members to take revenge (Hamayon 2009; Ruhlmann 2013, 2015a). A few Buddhist herders mentioned the ‘White oldest’ (Tsagaan övgön), a master of the land (earth and rivers) who is localized in the mountains and who has ‘the capacity to spread disasters such as extreme weather events, famine and diseases’ (herder, Hentii, winter 2014; see also Hamayon 1990, 710–12). The landscape, nature, and natural elements (rivers, mountains, stones, rocks, grass, plants and flowers, soil, etc.) are more or less ‘animated’ at times by spirits who can be or become angry.
Diseases affect the ‘body’ (biye) composed of flesh and bones and the ‘vital breath’ (am) of humans and animals; they consequently concern humans and animals, but not in the same way because ‘animals don’t have a soul, whereas human beings have one’ (herder, Hentii, summer 2014).[note 15] Diseases can cause the exit of the human soul (süns) from the body and allow it to enact its desire for revenge; in this way, diseases can counter the rebirth of the human soul.
In any case, diseases can cross species: pathogens, such as bacteria, viruses, or parasites, can be transmitted from herd to herd – a domestic species can contaminate another one or a wild species and vice versa – or from herd to herders. Diseases are pollution (buzar; see also Douglas 1966) and contagious (haldvart): they contaminate the soil, the water, the air, etc. They are living, autonomous, and mobile particles, which may exist in a state of sleep, latent in the soil, and re-emerge one or two years later. They populate the landscape, just as spiritual entities animate some of its elements.
Since they see the transmission of diseases as hazardous, herders are concerned with curing infected animals rather than culling them, because for them animals are a valuable possession that cannot be lost without unfortunate consequences.[note 16] Herders explained that culling animals by gunfire ‘brings misfortune’; killing animals and not eating them is ‘inappropriate’, ‘a sign and a cause of misfortune’; and killing animals rather than slaughtering them for food ‘brings misfortune’. When an animal, even an infected one, is culled – in other words, killed in the wrong way, with its blood pouring on the soil and polluting the land – many herders fear misfortune. Therefore, even if herders spot symptoms of diseases, some of them will not report it but instead try to cure animals themselves with medicinal and conjuration remedies, and by temporarily separating out infected animals. A herder in Hentii explained:
We firstly always try to cure infected animals. We fast identify sick animals and separate them from healthy animals to protect them from disease, and we cure infected animals, which we keep leashed far away, by hooking them to a pole planted in the ground far from the camp. We preferably don’t cull sick animals even if they are contagious, even if the disease is fatal, but it depends on the dangerousness for animals and humans. In the case of brucellosis, we don’t cull, even if it’s contagious and even if humans can contract it. But in the case of anthrax, we have to cull all suspected and infected animals because it’s a mortal disease. In the case of foot-and-mouth disease, we have to cull, but we don’t do all the time. We don’t say it, we keep it secret, we just don’t tell the veterinarian it emerged, but sometimes, when the virus persists and too many animals fall sick, we finally declare the disease. (summer 2015)
For a majority of herders, culling infected animals is unnecessary and ineffective: the proof is that even when they cull and vaccinate, diseases emerge the following year. In Töv, a herder insisted: ‘The case of foot-and-mouth disease monitoring is the best example of the inefficiency of culling suspected and infected animals, with or without vaccinating healthy animals, and veterinarians know that’ (summer 2014). Nevertheless, according to world animal health guidelines, the emergence of a disease requires curing infected animals and humans, and/or culling the first ones infected to stop the spread of the disease and the pollution it causes. It also involves being cautious with infected and/or contagious substances, such as meat and milk, blood and placental elements, saliva, hair, etc. In general, it is a common rule to boil meat and milk for a long time, which certainly is to satisfy tastes but also to prevent the contraction of zoonoses, such as brucellosis. Another common rule is to refrain from eating an infected animal after symptoms have been identified. In the case of ordinary nonzoonotic diseases, the flesh can be eaten after treatment or the entire carcass of the infected animal is simply thrown away. But in the case of highly contagious nonzoonotic diseases, such as foot-and-mouth disease, or deadly zoonotic diseases, like anthrax, the infected animals’ meat and milk cannot be eaten. The carcass is not thrown away but disinfected and buried or burned.
Even if herders generally rely on veterinarians in the case of highly contagious diseases, they first try to cure the symptoms, hoping the disease will stop. To do so, they use all the tools at their disposal. As one herder put it, ‘veterinarians or not, culling or vaccination or not, we don’t know why, but finally the disease stops on its own, and sometimes comes back the year after. That’s why we often do conjuration while curing them’ (summer 2015).
Foot-and-mouth disease: Veterinarians enter the environment of herders
Herders customarily cure the symptoms of foot-and-mouth disease by piercing and bleeding the hoof at its edge with a heated iron awl; they may also put salt in the animal’s mouth and make it swallow an infusion of the Little Peganum plant (Peganum nigellastrum Bge.) before cutting the hoof (Chagdarsürüng 1980, 134). But curing symptoms is not curing a disease or eradicating an epidemic – or worse, a panzootic.
According to veterinarians of NGOs and to the director of the National Veterinary Agency (winter 2014), as soon as herders identify the symptoms of foot-and-mouth disease, which include salivation, hoof swelling, and lameness, they must declare the disease to the veterinarian of the district. Emergency measures are rapidly implemented, as I observed when an outbreak occurred in the Sühbaatar province in the winter of 2014: the district veterinarian transmitted the information to the National Veterinary Agency; then, the National Emergency Management Agency sent an emergency veterinary team and mobilized military troops and police officers (a total of eight hundred emergency workers). Contaminated areas were quarantined following primary and secondary outbreaks. In this zone, suspected and infected animals – already dead or alive – were promptly carried away and gathered in the steppe to be culled, disinfected, and buried. With live infected animals, veterinarians cut each animal’s throat, allowing the blood to flow out onto the soil. This is an unusual way to kill an animal: in the customary way, herders open the animal down the sternum and promptly cut the thoracic aorta; they make sure that the blood does not fall on ‘the ancestors’ earth’, as they called it, but remains contained in the thoracic cavity (Ruhlmann 2015a). In case of heavy influx, veterinarians sometimes need military assistance. As many herders and state agents told me, and as I read in the newspapers and saw in anonymous online photos,[note 17] carcasses may be piled to be burned on bonfires (during winter, when the earth is too hard for digging), or put in a deep hole, disinfected with powdered lime, and covered with earth, with the surface of the hole being itself disinfected again with lime once flattened. Most of the time, sanitary and/or military forces destroy (ustgah) these carcasses, but sometimes herders do it themselves or help them, without any protection for their hands, faces, and bodies. Since disease chronically emerges in the four eastern provinces, in the beginning of autumn, before the ground is frozen, the government orders the digging of many large pits in anticipation of an outbreak.
The area for culling and disinfection is delimited with a red fabric barrier held by poles planted in the ground. On one side, animals are culled, on the other side, humans, vehicles, and tools are disinfected. Herders have to stop far away from the officer of disinfection, who sits in a small wooden house and disinfects them by stretching his arm through a small window opening. The herders descend from vehicles or from their horses at thirty meters from this disinfection station and follow the indicated ‘pedestrian entrance road’ and walk along the delimited path of red flags. Arriving at the disinfection officer, they receive through the small opening of the window a double disinfection: an internal one, a vaporization of a disinfectant and purifying product in the mouth called ‘spirt’, then an external one, taking a small ball of soaked cotton to apply spirt on their hands and faces. When the disinfection of their bodies is completed, herders disinfect their herding tools with the same sterilizing product that is used for vehicles, which is sprayed from a large barrel equipped with a sprayer. As soon as they return the camp, herders help sanitary officers disinfect the enclosure, the ground, and healthy animals with lime, while veterinarians administer vaccinations. Most of the time they can only vaccinate young and female animals, sometimes due to a lack of vaccines, sometimes due to the vaccination method adopted.
All along the border of the quarantined area, the police and military forces settle in strategic positions to prevent people from roaming with their vehicles and to prevent herders from leading their herds out onto pastures. They want to prevent viruses from spreading to the Western provinces, so that the capital city Ulaanbaatar is not affected and the national economy is not paralyzed.
Herders ‘know the risks’ of zoonotic pathogens, but ‘don’t fear them’ any more than ‘ordinary ones’, which are ‘not too dangerous’, as many herders said to me (Töv, summer 2015). They know that infected animals may contaminate healthy animals and/or humans, but also that they do not inevitably do so. They first consider diseases as a symptom of something they did wrong, the sign of the anger of a spirit. They know that they themselves (with the air they breathe, their hair, etc.) or their vehicle can transport a bacterium or a virus and thus contaminate another area, but they also think, contradicting themselves then, that it is without risk of circulation and they thus break the official rules. For example, during one of our interviews in 2014, the director of the National Veterinary Agency had been interrupted by a colleague who told him that once again herders had crossed the border of the quarantined area by jeep at night, despite security officers stationed in different places. Through the transmission of knowledge, and not firstly because the government, NGOs, and media relay information on disease symptoms and hygienic measures, herders know how brucellosis, anthrax, and foot-and-mouth disease are transmitted from one animal to another, or from animals to humans. Most of the time, they respect the international and the national regulations but they combine these regulations with many kinds of knowledge, conceptions, and principles regarding life and diseases. They consider the problem at different levels: the law, scientific knowledge, customary herding practices and care, and medicinal treatments and conjuration-protections, as well as their livestock capital and financial situation.
Herders make a distinction between the nature of the disease (virus, bacteria, parasite), the means of transmission of the disease (air, ground, water; enclosure and tools; placenta, blood, excreta, urine and saliva; carcasses, meat, and milk), and the origin of the disease (bad actions, bad feelings, misfortune; anger of the dead, spirits of nature, or Buddhist deities, etc.). That is the reason why herders deploy different ways to control and eradicate diseases. Some herders do not ask a monk to say prayers, or consult a shaman, while some others do; many herders declare the disease to the proper authority. However, after the official disinfection, they may also purify the pens and still-living animals, and do consecrated incense fumigations and, more rarely, libations with a mixture of consecrated water and milk. Fumigations and libations are ‘a way to repair bad actions or bad thoughts’, ‘to send away bad spirits and misfortune’; they are a way ‘to call back the good fortune and happiness’ (herder, Töv, summer 2014), or in other words, to reinstate order.
Neoliberal governmentality: A new regime of control for humans, animals, and pathogens
Parasites, bacteria, and viruses do not constitute pathogens for the nomadic herders to fight against but rather to live with, by controlling certain symptoms thanks to daily surveillance and to the use of popular treatments. Although infected animals are not seen as infectious agents to be systematically eradicated, the Mongolian government has sought to impose this understanding since the first half of the twentieth century, a goal that has been reinforced since the country’s accession to the World Organization of Animal Health. Many parasitic, bacterial, and viral animal diseases were under control during the Communist period (Ebright, Altantsetseg, and Oyungerel 2003; Odontsetseg, Mweene, and Kida 2005; Roth 2007; Zinsstag et al. 2007). According to an NGO veterinarian, at that time, ‘veterinarians were very well trained in Moscow and herders received an exemplary and complete animal health service’, and some herders remember that era ‘with nostalgia’ (Ulaanbaatar, winter 2014). A former herder I spoke with in Ulaanbaatar confirmed this: ‘Before, during the Communist period, veterinarians had good medicines, the veterinary care was good and free. Now it’s the opposite: they have bad and expensive medicines and some of them do their work poorly, they make mistakes, and animals sometimes die by veterinarians’ fault’ (winter 2014). Both NGO veterinarians and herders explained to me that ‘before’, each district had its own veterinary clinic with care management, animal health information, and a budget that was allocated for medicines and vaccination programs. Herders lament the decline in medicine quality and availability, the paucity of qualified veterinarians in the workforce, and the loss of free veterinary care.
For anthropologists, what is at stake is understanding how the government can simultaneously enforce international laws and respect the care practices of nomadic herders. This challenge exists in a context where the government, and particularly the National Veterinary Agency, must share initiatives with private partners. NGOs have developed, such as Agronomes et Vétérinaires Sans Frontières (AVSF), to foster local capacities for the treatment of animal diseases. Since 1990, the Ministry of Agriculture has alternated between a policy of vaccination and a policy of culling to control epizootic outbreaks. According to the project coordinator of AVSF, vaccination and culling sometimes concern the entire herd, and sometimes just a part of the herd, but this cannot be determined without any serological testing to identify the disease. Project managers of NGOs and herders argue that some private veterinarians have made mistakes in the administration of vaccines, using outdated or frozen vaccines, and vaccinating during the gestation period, causing abortions, etc. Some project managers claim that the vaccination program is applied for one or two years and stopped before it is successful. During the winter of 2010, the government culled infected animals in localized areas, where the primary outbreaks of disease were located in Sühbaatar province, vaccinated suspected but untested animals, and then culled other infected or suspected animals in areas of the secondary outbreak, ‘in order to consider which solution is the most effective and because there were no more vaccines left and a lack of financial support to buy enough vaccines for all entire herds in the whole quarantined zone’ (director of the National Veterinary Agency, Ulaanbaatar, winter 2014). The consequence was the spread of the foot-and-mouth virus to the four neighbouring provinces of Hentii, Dornod, Dorngov’, and Töv, the contamination of herds, and the eventual quarantine of a large part of the five impacted provinces. The official report to the World Organization of Animal Health indicates that a total of 25,914 infected animals were destroyed and around 6.5 million were vaccinated.
Being in contact with many Mongolian and international researchers and having access to their results, the government is grappling with the different kinds of medical knowledge they have produced.[note 18] It also has to deal with an insufficient budget, the absence of district veterinarians, and a lack of infrastructure to implement effective measures. During the winter of 2014, in the midst of a foot-and-mouth outbreak in the eastern provinces, the director of the National Veterinary Agency complained about not being able to buy vaccines from foreign countries (Russia, China, France, or India) and hoped that major foreign investors working in the contaminated area – the mining companies of the subsoil in Ömnögov’ and Dorngov’ – would finance the purchase of ten thousand vaccines required to eradicate the epizootic. After one month of this public health policy, I noticed that the epizootic was still spreading despite the quarantine procedure, and despite partial or total culling of contaminated herds or herds in contact with sick animals. In the media, herders in turn complained about the inadequate governmental financial compensations for livestock losses.[note 19] A former herder argued: ‘when a family loses its entire herd, it loses its livelihood’ (Ulaanbaatar, winter 2014). As another former herder and his wife explained to me in Ulaanbaatar, ‘We lost everything, our entire herd. And the compensation, the financial support from the government never came, so we decided to move and to live in a neighbourhood of yurts’. They continued: ‘families are forced to change their way of life, to abandon nomadic herding, to live on the periphery of an urban centre and to survive through odd jobs … to pay for food [meat and dairy products], to pay for water, coal heating, and electricity’ (winter 2014).
Foot-and-mouth disease presents an additional challenge for the government. Herds of domestic animals are seasonally in contact with herds of wild animals, particularly white-tailed gazelles, also called Mongolian gazelles (Procapra gutturosa). They live and migrate in a border region touching Mongolia, China, and Russia, where foot-and-mouth disease chronically emerges (see map above). Through media reports and interviews with my informants (herders and the director of the National Veterinary Agency), I noticed that each country rejects responsibility for outbreaks. The Chinese government blames the migrations of gazelles and the nomadic herding way of life. Supporting nomadic herding as part of its national heritage in the development of heritage and touristic programs, the Mongolian government prefers to shift responsibility to the gazelle – characterizing it as a ‘susceptible animal [medremtgii am’tan] that easily contracts infectious diseases, meaning the whitetail gazelles are a reservoir for foot-and-mouth disease’ (director of the National Veterinary Agency, Ulaanbaatar, winter 2014). Since 2000, Mongolia has culled gazelles and erected barbed fences to disrupt and limit their movement (Nyamsuren et al. 2006). While reports about the numbers of affected animals conflict (LHF 2010), the 2010 final report sent to the World Organization of Animal Health stated that, in an emergency action involving the mobilization of military forces, 917 gazelles presenting clinical symptoms were shot and their carcasses disinfected and buried (WAHIS Interface, n.d.). Despite many serological tests clearing gazelles,[note 20] the government acted upon ‘considerable local concern’ about their ‘potential role’ in ‘disease transmission’; interestingly, the report also mentions the destruction of 688 gazelle carcasses that ‘died for unknown reasons’. The 2010 report also notes that the ‘source of the outbreak(s) or origin of infection’ is ‘unknown or inconclusive’ (WAHIS Interface, n.d.).
In 1999, 2001, 2005, 2007, and 2011 Mongolian and international scientists indeed proved through serological research that it is the domestic herds that contaminate the wild herds and not the contrary (Bolortsetseg et al. 2012; Deem et al. 2001; Deem et al. 2002; Huhuu et al. 2000; LHF 2010; Shiilegdamba et al. 2008). NGOs have tried to convince the government to establish a biannual vaccination program for all herds in the four eastern provinces, reminding the government that gazelles are a protected species because they became endangered in the early 2000s, though they are increasing in number. Herders do not accept the culling of hundreds of gazelles, a protected and iconic wild animal, the hunting of which is forbidden by the government. It seems that the culling of animals is better approved when ‘the decision comes from herders themselves’ and when it is ‘unusual’, that is to say not chronic, ‘not every year’, or in a tolerable, moderate number of ‘just a few and really infected animals’ (herder, Töv, summer 2014).
Conclusion
The role of sentinel that has been imposed on herders by the new governance of animal diseases requires them to reconnect with state-driven practices of care and surveillance that veterinarians executed under the Communist period, and also to connect with local knowledge of symptoms and signs of disease, while taking the possibility of misfortune and angry spirits into account, to find appropriate causes and treatments for animal diseases. On the one hand, the government expects herders to play this role carefully. On the other hand, herders regularly point out many discrepancies in culling policy: the arbitrary nature of partial or total culling of domestic animals; the random and illegal shooting of the wild gazelles, a protected species; and the contradictory government orders that alternate culling and vaccination without prior testing due to a lack of an effective vaccination program. They lament the absence of a vaccination program for all herds throughout the country, the lack and poor quality of vaccines, the errors concerning their modalities of inoculation by the veterinarians, the costs of veterinary care, etc. Despite these tensions over culling and vaccination, the herders play their role of sentinel conscientiously, not only because they must follow official regulations but also because they comprehend different kinds of approaches to animal diseases. They combine shamanic, Buddhist, and Western veterinary medicine systems, including local and nonlocal knowledge and know-how. And finally, they play this role because they live in coexistence with their herds and because the health of the herd is for them an indicator of good fortune, of happiness, and of prosperity for humans and for animals.
The nomadic culture and the human-animal relationship underlying the perception of animal diseases are not in opposition to the ‘scientific knowledge’ and public policy of animal health, although international veterinarians from the NGOs WWF Mongolia and AVSF say that herders ‘generally prefer fumigation and refuse vaccines’ (Ulaanbaatar, winter 2014). They combine both, fumigation and vaccines, when they trust in veterinarians, though they also criticize veterinarians for their mistakes. But despite or because of a lack of trust, as herders trust and do not trust at the same time (Ruhlmann 2015b), and following the government’s injunctions, the Mongolian system of animal surveillance works through the daily control practiced by herders. This syndromic system of surveillance does not consist only in categorizing specific clinical events as indicators of a disease (fever, lameness), but also in being attentive to nonspecific health indicators. In a context of financial distress and amidst tensions between local and scientific knowledge and political power (Ruhlmann 2015b), the Mongolian government is able to implement and maintain a governance of animal diseases based on a distribution of roles where humans have learned to share in the management of pathogens while respecting some customary pastoral practices. Political leaders delegate a wide responsibility to herders themselves in the surveillance and management of diseases, considering them as coworkers in the pastoral economy of the country and as the frontline in the emergence of epizootics and zoonoses. In this sense, Mongolia is a sort of laboratory for studying the implementation of a neoliberal governmentality of animal diseases, where the capacities to manage diseases that spread across species (wild/domestic, animal/human) and political borders (regional/national/continental) are delegated to local bottom-level actors.
Acknowledgments
This ethnographical fieldwork has been developed with the support of the Laboratory of Social Anthropology (Paris) and the Axa Research Fund which financed my post-doctorate. I would like to thank the various thoughtful readers and proofreaders who have helped me to clarify parts of my article. I thank them also for the tedious work they have done to correct my English.
About the author
Sandrine Ruhlmann is Researcher of Anthropology at CNRS (UMR 8173 China, Korea, Japan), who specializes in the techniques, material culture, and food practices of Mongols. She studies Mongolian food culture in Mongolia and Southern Mongolia, by exploring the processes of compromise deployed by dominated Mongolian people under the Mongolian and Chinese Communist and post-Communist regimes. She also studies food, health, and security crises through the surveillance of animal diseases and the control of animal and human populations (see https://etudesmongolesetsiberiennes.fr/ruhlmann-sandrine/). Her book L’appel du Bonheur. Le partage alimentaire mongol (Food Sharing in Mongolia: Beckoning Happiness) was published in 2015 (CEMS-EPHE). She has also published many articles in French and in international journals and edited collections (see http://cecmc.ehess.fr/index.php?2528).
References
Adiyasuren, Z., Ts. Ankhtuyaa, and A. Dolgorkhand. 2005. ‘The Current Status of Human Anthrax Epidemiology in Mongolia’. In Proc. Symposium on Problems for Mongolian Medical Science 22: 66–67. Ulaanbaatar: Mongolian Health Academy and Ministry for Health of Mongolia.
Badarch, P. 2000. ‘Early Epizootic Spread of Foot-and-Mouth Disease in Mongolia and Control Measures Taken’. Journal of Mongolian Veterinary Medicine 32: 21–23.
Barbier, Marc. 2006 ‘Surveiller pour Abattre. La Mise en Dispositif de la Surveillance Épistémologique et de la Police Sanitaire de l’ESB (Enquête)’. Terrains & Travaux 11: 101–21.
Basan, Batsukh, Tsedenkhuu Purevkhuu, and Baatar Togoonyam. 2013. The Current Situation on FMD Control in Mongolia. World Organisation for Animal Health meeting report. http://www.rr-asia.oie.int/fileadmin/Regional_Representation/Programme/G_GFTADs/FMD/2013_Meetings_under_OIE_JTF_Project_for_FMD_Control_in_Asia/3._Scientific_Mtg/Abstract_Mongolia_Batsukh_Basan.pdf.
Batsukh, Zayat, B. Tsolmon, Dashdavaa Otgonbaatar, Baatar Undraa, Adyadorj Dolgorkhand, and Ochirpurev Ariuntuya. 2013. ‘One Health in Mongolia’. Current Topics in Microbiology and Immunology 366: 123–37. https://doi.org/10.1007/978-3-642-35846-3.
Batsuuri, N. 2001. ‘63 Day Action against Foot-and-Mouth Disease’. Journal of Mongolian Veterinary Medicine 37: 11–13.
Baumann, Brian. 2008. Divine Knowledge: Buddhist Mathematics According to the Anonymous Manual of Mongolian Astrology. Leiden: Brill.
Bawden, Charles R. 1958. ‘On the Practice of Scapulimancy Among the Mongols’. Central Asiatic Journal 4 (1): 1–44.
Bawden, Charles R. 1961. ‘The Supernatural Element in Sickness and Death according to Mongol Tradition’. Asia Major 8 (2): 215–57.
Bawden, Charles R. 1962a. ‘Calling the Soul: A Mongolian Litany’. Bulletin of the School of Oriental and African Studies 25 (1-3): 81–103.
Bawden, Charles R. 1962b. ‘The Supernatural Element in Sickness and Death according to Mongol Tradition’. Asia Major 9 (2): 153–78.
Bolortsetseg, Sanjaa, Enkhtuvshin Shiilegdamba, D. Nyamsuren, Wendy Weisman, Amanda Fine, Angela Yang, and Damien O. Joly. 2012. ‘Serosurveillance for Foot-and-Mouth Disease in Mongolian Gazelles (Procapra gutturosa) and Livestock on the Eastern Steppe of Mongolia’. Journal of Wildlife Diseases 48 (1): 33–38. https://doi.org/10.7589/0090-3558-48.1.33.
Caduff, Carlo. 2014. ‘Sick Weather Ahead: On Data-Mining, Crowd-Sourcing and White Noise’. Cambridge Anthropology 32 (1): 32–46.
Chabros, Kristina. 1992. Beckoning Fortune: A Study of the Mongol Dalaga Ritual. Wiesbaden: O. Harrassowitz.
Chagdarsürüng, Ts. 1980. ‘L’art Vétérinaire des Mongols Nomades’. Studia Mongolica 8 (16-9): 125–37.
Chateauraynaud, Francis. 1997. ‘Vigilance et Transformation. Présence Corporelle et Responsabilité dans la Conduite des Dispositifs Techniques’. Réseaux 15 (85): 101–27.
Chateauraynaud, Francis, and Didier Torny. 1999. Les Sombres Précurseurs. Une Sociologie Pragmatique de l’Alerte et du Risque. Paris: Éditions de l’EHESS.
Clavandier, Gaëlle. 2006. ‘La Vigilance Comme Avatar de la Société du Risque. Quand la Démocratie Devient une Figure Emblématique du Discours Scientifique’. In Être Vigilant. L’Opérativité Discrète de la Société du Risque, edited by Jacques Roux, 221–35. Saint-Étienne: Publications de l’Université de Saint-Étienne.
Collier, Stephen J., Andrew Lakoff, and Paul Rabinow. 2004. ‘Biosecurity: Towards an Anthropology of the Contemporary’. Anthropology Today 20 (5): 3–7. https://doi.org/10.1111/j.0268-540X.2004.00292.x.
Dashnyam, Bubein, and Raymond A. Zilinskas. 2003. ‘Review of Developments in Biotechnology in Mongolia’. In Mongolia Today: Science, Culture, Environment and Development, edited by Dendeviin Badarch, Raymond A. Zilinskas, and Peter J. Balint, 49–66. London: Routledge, Curzon.
Deem, S. L., M. Linn, William B. Karesh, G. Schaller, B. Lhagvasuren, B. Nyamsuren, Kirk Olson, and E. Dierenfeld. 2001. ‘Health Evaluation of Mongolian Gazelles Procapra gutturosa on the Eastern Steppes of Mongolia’. Gnusletter 20 (2): 18–20.
Deem, S. L., M. Linn, William B. Karesh, G. Schaller, B. Lhagvasuren, B. Nyamsuren, Kirk Olson, and E. Dierenfeld. 2002. ‘Health Evaluation of Mongolian Gazelles Procapra gutturosa on the Eastern Steppes of Mongolia’. Gnusletter 21 (1): 23–24.
Doré, Antoine. 2013. ‘L’Exercice des Biopolitiques. Conditions Matérielles et Ontologiques de la Gestion Gouvernementale d’une Population Animale’. Revue d’Anthropologie des Connaissances 7 (4): 837–55.
Douglas, Mary. 1966. Purity and Danger: An Analysis of Concepts of Pollution and Taboo. London: Routledge and Kegan Paul.
Ebright, John R., Togoo Altantsetseg, and Ravdan Oyungerel. 2003. ‘Emerging Infectious Diseases in Mongolia’. Emerging Infectious Diseases 9 (12): 1509–15.
Empson, Rebecca. 2012. ‘The Danger of Excess. Accumulating and Dispersing Fortune in Mongolia’. Social Analysis 56 (1): 117–32.
Enticott, Gareth. 2001. ‘Calculating Nature: The Case of Badgers, Bovine Tuberculosis and Cattle’. Journal of Rural Studies 17 (2): 149–64. https://doi.org/10.1016/S0743-0167(00)00051-6.
Enticott, Gareth. 2008. ‘The Spaces of Biosecurity: Prescribing and Negotiating Solutions to Bovine Tuberculosis’. Environment and Planning A 40 (7): 1568–82. https://doi.org/10.1068/a40304.
Enticott, Gareth, and Frank Vanclay. 2011. ‘Scripts, Animal Health and Biosecurity: The Moral Accountability of Farmers’ Talks about Animal Health Risks’. Health, Risk & Society 13 (4): 293–309. https://doi.org/10.1080/13698575.2011.575456.
Fallon, Catherine, Grégory Piet, Étienne Thiry, Fabiana Dal Pozzo, and Catherine Zwetkoff. 2012. ‘Renouveler la Gestion du Risque par l’Ouverture à un Système de Vigilance ? Le Cas de la Fièvre Catarrhale Ovine’. VertigO - La Revue Électronique en Sciences de l’Environnement 12 (3). https://doi.org/10.4000/vertigo.13153.
Fearnley, Lyle. 2008. ‘Signals Come and Go: Syndromic Surveillance and Styles of Biosecurity’. Environment and Planning 40 (7): 1615–32. https://doi.org/10.1068/a4060.
Fish, Robert, Zoe Austin, Robert Christley, Philip M. Haygarth, Louise A. Heathwaite, Sophia Latham, William Medd, Maggie Mort, David M.Olivier, Roger Pickup, Jonathan M. Wastling, and Brian Wynne. 2011. ‘Uncertainties in the Governance of Animal Disease: An Interdisciplinary Framework for Analysis’. Philosophical Transactions of The Royal Society B 366: 2023–34. https://doi.org/10.1098/rstb.2011.0151.
Foucault, Michel. 1994. ‘La “Gouvernance”’. In Dits et Écrits III, 635–57. Paris: Gallimard, Seuil.
Foucault, Michel. 2004. Sécurité, Territoire, Population. Cours au Collège de France, 1977–1978. Paris: Gallimard, Seuil.
Giles-Vernick, Tamara, Abdoulay Traoré, and Louis Bainilago. 2015. ‘Incertitude, Hepatitis B, and Infant Vaccination in West and Central Africa’. Medical Anthropology Quarterly 30 (2): 203–21.
Hamayon, Roberte. 1978. ‘Soigner le Mort pour Guérir le Vif’. Nouvelle Revue de Psychanalyse 17: 55–72.
Hamayon, Roberte. 1990. La Chasse à l’Âme. Esquisse d’une Théorie du Chamanisme Sibérien. Nanterre: Société d’Ethnologie.
Hamayon, Roberte. 2009. ‘Âme, Force Vitale, Esprit. L’Animisme dans le Chamanisme des Peuples Chasseurs de la Forêt Sibérienne’. In L’animisme Parmi Nous, edited by Robert Asséo, Jean-Louis Baldacci, Bernard Chervet, Sylvie Dreyfus-Asséo, Michèle Emmanuelli, Claude Janin, Félicie Nayrou, and Anne-Christine Taylor, 201–10. Paris: PUF.
Hinchliffe, Steve, John Allen, Stephanie Lavau, Nick Bingham, and Simon Carter. 2012. ‘Biosecurity and the Topologies of Infected Life: from Borderlines to Borderlands’. Transactions of the Institute of British Geographers 38 (4): 531–43. https://doi.org/10.1111/j.1475-5661.2012.00538.x.
Huhuu, A., S. Tserendorj, T. Bazartseren, and L. Noronpil. 2000. ‘Foot-and-Mouth Disease Diagnosis During the Outbreaks in Dorngobi Province’. Journal of Mongolian Veterinary Medicine 32: 13–15.
Humphrey, Caroline. 1984. ‘A Fragmentary Text of Curative Magic’. Journal of the Anglo-Mongolian Society 9 (1-2): 27–33.
Keck, Frédéric. 2010. ‘Une Sentinelle Sanitaire aux Frontières du Vivant. Les Experts de la Grippe Aviaire à Hong Kong’. Terrain 54: 26–41. https://doi.org/10.4000/terrain.13928.
Lemke, Thomas. 2004. ‘“Marx sans les Guillemets”: Foucault, la Gouvernementalité et la Critique du Néolibéralisme’. Traduit de l’anglais par Marc Chemali. Actuel Marx 36: 13–26. https://doi.org/10.3917/amx.036.0013.
LHF (Large Herbivore Foundation). 2010. ‘Update on FMD in Mongolia: Life Stock Vaccination, or Killing Wild Life?’ LHNet, 21 December. http://www.lhnet.org/update-on-fmd-in-mongolia-life-stock-vaccination-or-killing-wild-life/.
Meserve, Ruth. 1986-1987. ‘A Mongol Cure for the Rabid Horse’. Mongolian Studies 10: 89–96.
Meserve, Ruth. 1993. ‘Additional Notes on Mongol Treatments for Rabid Animals’. Mongolian Studies 16: 41–54.
Meserve, Ruth. 1996. ‘The Terminology for the Diseases of Domestic Animals in Traditional Mongolian Veterinary Medicine’. Acta Orientalia Academiae Scientiarum Hungaricae 49 (3): 335–58.
Meserve, Ruth. 2003. ‘On the History of Medicinal Plant Research in Mongolia’. Studia Orientalia 97: 155–67.
Mostaert, Antoine. 1969. Manual of Mongolian Astrology and Divination. Cambridge, MA: Harvard University Press.
Nyamsuren, D., Damien O. Joly, Enkhtuvshin Shiilegdamba, D. Odonkhuu, Kirk A. Olson, Matthys Draisma, and William B. Karesh. 2006. ‘Exposure of Mongolian Gazelles (Procapra gutturosa) to Foot-and-Mouth Disease Virus’. Journal of Wildlife Diseases 42 (1): 154–58. https://doi.org/10.7589/0090-3558-42.1.154.
Odontsetseg, Namsraijav, Aaron S. Mweene, and Hiroshi Kida. 2005. ‘Viral and Bacterial Diseases in Livestock in Mongolia’. Japanese Journal of Veterinary Research 52 (4): 151–62. https://doi.org/10.14943/jjvr.52.4.151.
Odontsetseg, Namsraijav, Sh. Tserendorj, Z. Adiyasuren, D. Uuganbayar, and Aaron S. Mweene. 2007. ‘Anthrax in Animals and Humans in Mongolia’. Scientific and Technical Review of the Office International des Epizooties (Paris) 26 (3): 701–10.
Odontsetseg, Namsraijav, D. Uuganbayar, Sh. Tserendorj, and Z. Adiyasuren. 2009. ‘Animal and Human Rabies in Mongolia’. Scientific and Technical Review of the Office International des Epizooties (Paris) 28 (3): 995–1003.
Perrin, Jean-Baptiste, Christian Ducrot, Didier Calavas, and Pascal Hendrikx. 2011. ‘La Surveillance Syndromique, une Nouvelle Approche pour la Surveillance Épidémiologique’. Le Nouveau Praticien Vétérinaire Élevages et Santé 4 (17): 9–13.
Prete, Giovanni. 2008. ‘Surveiller en Éradiquant: l’Importance des “Médiateurs de la Surveillance” et des Réseaux Informels dans la Surveillance des Risques Sanitaires et Environnementaux’. Sociologie du Travail 50: 489–504. https://doi.org/10.1016/j.soctra.2008.09.002.
Racloz, Vanessa, Esther Schelling, Nakul Chitnis, Felix Roth, and Jakob Zinsstag. 2013. ‘Persistence of Brucellosis in Pastoral Systems’. Scientific and Technical Review of the Office International des Epizooties (Paris) 32 (1): 61–70. https://doi.org/10.20506/rst.32.1.2186.
Roth, Felix. 2007. ‘The Development of Brucellosis Control in Mongolia’. PhD diss., London School of Hygiene and Tropical Medicine. https://doi.org/10.17037/PUBS.00682361.
Roth, Felix, Jakob Zinsstag, Dontor Orkhon, G. Chimed-Ochir, Guy Hutton, Ottorino Cosivi, Guy Carrin, and Joachim Otte. 2003. ‘Human Health Benefits From Livestock Vaccination for Brucellosis: Case Study’. Bulletin of the WHO 81 (12): 867–76.
Roux, Jacques, ed. 2006. Être Vigilant. L’Opérativité Discrète de la Société du Risque. Saint-Étienne: Publications de l’Université de Saint-Étienne.
Ruhlmann, Sandrine. 2012. ‘Appeler le Bonheur. À Propos de Quelques Pratiques Propitiatoires Domestiques en Mongolie’. In Deviner pour Agir. Regards Comparatifs sur des Pratiques Divinatoires Anciennes et Contemporaines, edited by Jean-Luc Lambert and Guilhem Olivier, 191–213. Paris: CEMS-EPHE.
Ruhlmann, Sandrine. 2013. ‘Quand les Âmes Errantes des Morts se Déplacent Accrochées aux Poils et aux Plumes des Animaux Sauvages. La Vie Post Mortem des Âmes en Mongolie Contemporaine’. In D’une Anthropologie du Chamanisme vers une Anthropologie du Croire. Hommage à l’œuvre de Roberte Hamayon, edited by Katia Buffetrille, Jean-Luc Lambert, Nathalie Luca, and Anne de Sales, 283–302. Paris: CEMS-EPHE.
Ruhlmann, Sandrine. 2015a. L’Appel du Bonheur. Le Partage Alimentaire Mongol. Paris: CEMS-EPHE.
Ruhlmann, Sandrine. 2015b. ‘Des Éleveurs Sentinelles. Les Politiques Contemporaines de Surveillance des Maladies Animales en Mongolie’. Revue d'Anthropologie des Connaissances 9 (2): 237–64. https://doi.org/10.3917/rac.027.0237.
Sanjaatogtokh, Ravdan. 2001. ‘Mongolie : l’Épizootie de Fièvre Aphteuse et les Mesures Appliquées en 2000–2001’. Bulletin de l’OIE 4: 475–541.
Sanjaatogtokh, Ravdan. 2003. ‘Preliminary Results of Rinderpest Surveillance in Mongolia’. Bulletin de l’OIE 3: 29–31.
Shiilegdamba, Enkhtuvshin, Tim E. Carpenter, Andrés M. Perez, and Mark C. Thurmond. 2008. ‘Temporal-Spatial Epidemiology of Foot-and-Mouth Disease Outbreaks in Mongolia, 2000–2002’. Veterinary Research Communications 32 (3): 201–07. https://doi.org/10.1007/s11259-007-9018-6.
Sodnomdarjaa, Ruuragchaa. 2001. ‘The Specificity of Foot-and-Mouth Disease Outbreak Spread and Control Measures’. Journal of Mongolian Veterinary Medicine 37: 3–12.
Sodnomdarjaa, Ruuragchaa. 2004. ‘The Epidemiology and Control of Foot-and-Mouth Disease in Mongolia’. Paper presented at the 13th Federation of Asian Veterinary Associations Congress,Seoul, Korea, 25–27 October.
Stirling, Andrew. 2007. ‘Risk, Precaution and Science: Toward a More Constructive Policy Debate’. EMBO Reports 8: 309–14. https://doi.org/10.1038/sj.embor.7400953.
Torny, Didier. 1998. ‘La Traçabilité comme Technique de Gouvernement des Hommes et des Choses’. Politix 11 (44): 51–75. https://doi.org/10.3406/polix.1998.1761.
Tserendorj, Sh. 2005. ‘Results of Studies on the Causative Agent of Anthrax and Development of Appropriate Methods to Control the Disease Foci’. PhD diss., Ministry for Education, Culture and Science of Mongolia.
WAHIS Interface. n.d. Searches for ‘Foot-and-Mouth Disease’ and ‘Mongolia’. OIE Reports. http://www.oie.int/wahis_2/public/wahid.php/Wahidhome/Home.
Woods, Abigail. 2004. A Manufactured Plague: The History of Foot and Mouth Disease in Britain. London: Earthscan.
Zinsstag, Jakob, Felix Roth, Dontor Orkhon, G. Chimed-Ochir, M. Nansalmaa, J. Kolar, and Penelope Vounatsou. 2005. ‘A Model of Animal-Human Brucellosis Transmission in Mongolia’. Preventive Veterinary Medicine 69: 77–95. https://doi.org/10.1016/j.prevetmed.2005.01.017.
Zinsstag, Jakob, Esther Schelling, Felix Roth, Bassirou Bonfoh, Don De Savigny, and Marcel Tanner. 2007. ‘Human Benefits of Animal Interventions for Zoonosis Control’. Emerging Infectious Diseases 13 (4): 527–31. https://doi.org/10.3201/eid1304.060381.
Endnotes
1 Back
Figures were taken from the website of National Statistics Office of Mongolia (http://www.en.nso.mn/index.php) in 2014.
2 Back
Animal diseases may, for example, interrupt the provision of supplies to the country’s cities and exports of animals and animal products from Mongolia.
3 Back
Among nonspecific health indicators, there is an unusual increase in mortality to detect outbreaks of an infectious disease (Perrin et al. 2011).
4 Back
Vigilance is a widely studied concept in sociology and anthropology, in particular by Chateauraynaud (1997), Chateauraynaud and Torny (1999), Clavandier (2006), Roux (2006), Fearnley (2008), Prete (2008), Fallon et al. (2012), and Caduff (2014).
5 Back
These categories are more or less permeable depending on the period, the country, and the efficiency of techniques. Thus, when the traditional politics of protection and isolation (quarantine) seem inefficient for facing animal diseases, new techniques of governance of people, animals, and animal goods are implemented, such as traceability (Torny 1998). And surveillance sometimes consists of eradicating one part, such as the reservoir of a disease, or animals or herds involved in an outbreak (Prete 2008; Barbier 2006). Sometimes surveillance requires elimination, and sometimes control does not, and sometimes it requires quarantine, vaccination, and culling.
6 Back
Concerning mediators and informal networks in the surveillance of health and environmental risk, see Prete (2008).
7 Back
Regarding the animal health risks and the concept of script in the biosecurity context, see Enticott and Vanclay (2011). To understand the link between animal health, biosecurity, and constructions of spaces and the management of nature, based on the example of bovine tuberculosis in comparison with foot-and-mouth disease, see also Enticott (2001, 2008). For the issue of both biosecurity and the topologies of infected versus noninfected life and the crossing of barriers, see Hinchliffe et al. (2012).
8 Back
For a good example of the exercise of biopolitics in the governance of animal populations, see Doré (2013).
10 Back
Regarding the rituals and techniques of calling or calling back happiness, see Bawden (1962a, 1962b), Chabros (1992), and Ruhlmann (2015a). Other practices based on astrology are sometimes mobilized in the context of cure and protection: divination (Mostaert 1969; Baumann 2008), specifically scapulimancy (Bawden 1958) and propitiation (Ruhlmann 2012).
11 Back
Chagdarsürüng (1980), Humphrey (1984), and Meserve (1996) already mentioned thirty years ago most or all of these treatments or curative techniques, except that of setting alight (tüimerdeh) consisting of ‘use of sparks from flint or bones struck together to cure herpes and ringworm’ (Humphrey 1984, 28).
12 Back
Chagdarsürüng (1980, 132) also notes the use of bile (of marmot, bear, chamois, or wild goat) and blood (of gazelle, antelope, or horse).
13 Back
Regarding the medicinal plants used in Siberia – and some of them in Mongolia – see Hamayon (1978, 59, n2).
14 Back
See Meserve (1996, 336) for an analysis of the naming of diseases according to delineation of external or internal disease, attributed to a supernatural cause, accompanied by the name of the animal or another animal, a color (blue, black, white), the afflicted part of the body, etc.
15 Back
For humans, illness and death are two states in which the soul (süns) separates from the body. After death, the soul may be born again in another human body, ideally in a descendant. Very few people know of the Buddhist conception of being reborn in the body of an animal, inherited from doctrinal Tibetan Buddhism, and the majority of them reject the idea. Most people do many meritorious actions during their life in order to be reborn as a human rather than suffer this ‘bad rebirth’ (Ruhlmann 2015a).
16 Back
See also Meserve (1986-87, 91), who writes that Mongolian herders ‘often scoffed at Western veterinary science’ recommendations that ‘all infected animals be destroyed’, as they saw certain contagious diseases as not ‘nearly so catastrophic’.
17 Back
See the series of photos entitled ‘Work of fighting foot-and-mouth disease’ (Shülhii övchintei temtseh azhil), published on the INET website: http://photo.inet.mn/main/?id=52501.
18 Back
In fact, since the early 2000s, the profusion of scientific articles on epizootics indicates that the government has access to Mongolian and international economic and serological data and knowledge (see, for example, Badarch 2000; Huhuu et al. 2000; Batsuuri 2001; Roth et al. 2003; Deem et al. 2001, 2002; Dashnyam and Zilinskas 2003; Sanjaatogtokh 2001, 2003; Ebright et al. 2003; Sodnomdarjaa 2001, 2004; Tserendorj 2005; Adiyasuren, Ankhtuyaa, and Dolgorkhand 2005; Odontsetseg, Mweene, and Kida 2005; Odontsetseg, Tserendorj, et al. 2007; Odontsetseg, Uuganbayar, et al. 2009; Zinsstag et al. 2005, 2007; Nyamsuren et al. 2006; Shiilegdamba et al. 2008; Bolortsetseg et al. 2012; Racloz et al. 2013; Batsukh et al. 2013).
19 Back
According to the ‘Protection Animal Health and Genetic Pool’ law, herders should get 90 per cent of the market value of their animals as compensation (Basan et al. 2013).
20 Back
See for example Deem et al. (2001, 2002); Nyamsuren et al. (2006); LHF (2010); Bolortsetseg et al. (2012).
