Based on an analysis of the Meningitis Vaccine Project (MVP), a public-private partnership (PPP) set up to introduce the MenAfriVac® vaccine in African countries, this article examines the failures of an accelerated disease control programme that targeted a highly infectious disease. I argue that the integration of MenAfriVac® into the World Health Organization’s (WHO) Expanded Programme on Immunisation had the effect of reinforcing inequalities in access, in particular during epidemic emergencies. I will also show how vaccine shortages during an outbreak in Niger led to political tensions and to the emergence of a parallel and unregulated ‘black market’ of vaccines.
Global health Initiatives as a ‘Drunken Boat’
The Meningitis Vaccines Project Case Study
—
Abstract
Introduction
African vaccinology has, for several years, been undergoing a major reconfiguration. In line with wider structural changes to health systems across the continent, public-private partnership (PPP) models have become central within global health projects and a common vehicle for developing and producing vaccines at cost and scale so as to make them accessible in low- and middle-income countries (Gaudillière 2016; Guilbaud 2015). Founded in 1999, the Global Alliance for Vaccines and Immunization (GAVI) is the main international actor driving this change in the vaccinology field. The GAVI promotes unprecedented funding opportunities and offers an institutional and normative framework for representing the interests and points of view of a wide range of public, private, and charitable health partners (Storeng 2014). At the same time, however, a range of issues limits the effectiveness of PPP interventions, including, inter alia , relationships of accountability between health system sectors and partners, health professionals, and communities. In this article, I use the GAVI’s Meningitis Vaccines Project (MVP) in Niger as a case study to analyse transformations in West African immunisation policies at the intersection of PPP, epidemic response, and vaccinology.
The Position Piece draws from fieldwork conducted since 2009 investigating the question of why, despite meningitis’ predictable seasonality, disease epidemics have remained a constant emergency for global health actors (Thiongane 2013). The case I explore here follows the development and launch of MenAfriVac®, a new meningitis vaccine, the accompanying construction of vaccine introduction narratives, and the consequences of these narratives in resources-poor settings. In particular, I probe the multiple and fragmentary aims (Biehl and Petryna 2013) of the MVP, paying particular attention to what was deliberately hidden or left unspoken during the launch. Against a background of exploding meningitis outbreaks and acute vaccine shortages in West African countries, the MVP intervention worsened a parallel system of care and governance between public and private sectors. The aim of the Position Piece is to discuss the conditions of the emergence of health inequities in vaccination and the consequences of the immunisation choices made by global health entrepreneurs—an experience for Nigerians that I frame, after the famous 19th - century French poet Arthur Rimbaud—as like being on a ‘drunken boat’ (i.e., a chaotic, hectic, and bumpy ride) (1999).
In Niamey a vaccine trial leaves Nigeriens in the lurch
Two years after the creation of the Global Alliance for Vaccines and Immunization (GAVI), the Meningitis Vaccine Project (MVP) was established as a public-private partnership (PPP). Its founding led to a lengthy controversy that I will briefly set out here as it contextualises some of the dynamics at work in the social worlds of vaccination (Thiongane 2013). In 1997, following a meningitis pandemic that had a disastrous impact on countries in the ‘meningitis belt’, [1] a scientific controversy arose between two groups. The first group was made up of the developers of the first generation of vaccinations against meningococcal meningitis, their colleagues at the National Institute of Child Health (NICH), the Rockefeller Institute in New York, and the director of the Centre de Recherche sur les Meningites et les Schistosomiases (CERMES) in Niger. The second group included epidemiologists and modellers from the World Health Organization (WHO), the Centers for Disease Control and Prevention (CDC), and members of Epicentre, Médecins Sans Frontières’s (MSF) epidemiological research division.
A six-year debate finally led to the withdrawal of the polysaccharide vaccines used against meningitis, which were developed in the mid-1960s. The polysaccharide vaccines had been used in both MSF and WHO emergency vaccination campaigns and played an important role in the standard response to epidemic outbreaks, where vaccines would be sent into affected areas as and when they were needed (Thiongane 2013). The withdrawal of the polysaccharide vaccines was a boost for the project, which aimed to develop a conjugate anti-meningitis vaccine (that is, a delivery system in which the immunogenic protein is bound to a diphtheria toxin as a carrier protein that stimulates an antigen response). Conjugate vaccines give better and longer-lasting immunity, which translates to longer protection against disease for recipients. The new vaccine was tested in over 600 infants in a trial that ran from March 1997 to September 2000 at CERMES in Niamey (Campagne et al. 2000). The vaccine, which provided protection against MenA and MenC serogroups (MenA is the most common serogroup in Africa), would subsequently be marketed in Europe and America as granting protection against serogroup MenC, the most widespread serogroup in rich countries, and would be limited to those markets.
This strategic choice, based entirely on economic interests, led the director of CERMES to admit that he had been ripped off by the manufacturers and let down by the WHO (Chippaux 2001a; 2001b). In 2001, Chippaux’s protest was conveyed via op-eds. His critique had little to say about the rights of the low-income countries that had served as experimental spaces for testing to access the final products; he focused instead on an emergency vaccination strategy that was primarily concerned with putting out fires and delivering inadequate vaccines even as epidemics ravaged Sahelian countries. [2] The debate around trials and access was not raised. A year later, the MVP was put in place with the objective of making the conjugate vaccine available in sub-Saharan Africa. The goal was to develop a conjugate vaccine against serogroup MenA, believed to be the most common form of meningitis in the African meningitis belt. This conjugate vaccine bound the polyoxide to a tetanus toxin.
MenAfriVac: A ‘vaccine for the poor’?
The Meningitis Vaccine Project (MVP) began as an initiative of the World Health Organization (WHO) and the Programme for Appropriate Technology in Health (PATH) with the objective of preventing meningitis epidemics in sub-Saharan Africa. Its responsibilities were to establish, develop, introduce, and roll out vaccines on a large scale. In 2000, the WHO put out a call for expressions of interest, bringing together public- and private-sector actors in Ouagadougou. Discussions with pharmaceutical industry leaders such as Sanofi Pasteur and GlaxoSmithKline (GSK), who held the patent on the polyvalent conjugate vaccines, quickly stalled. After the Gates Foundation donated 70 million dollars to finance the negotiation, an agreement was signed in 2001. It allowed for the transfer of affordable conjugate methods from the American Food and Drug Administration (FDA) Centre for Biological Evaluation and Research (in collaboration with the US National Institutes of Health) to the Serum Institute of India (located in the city of Pune), a pharmaceutical firm specialising in the production of vaccines for children.
While this agreement was being negotiated, a meningitis pandemic broke out in Saudi Arabia. After being reported in 10 countries, the pandemic reached West Africa, where it had a particularly severe impact in Burkina Faso. Genomic analysis revealed that the pandemic was due to a particular clonal complex of serogroup W135, a strain associated with a high mortality rate. Vaccine shortages prevented an effective response to the outbreaks, and Saudi Arabian authorities banned pilgrims from West Africa from travelling to Mecca. Nonetheless, the pandemic spread as far as the United Kingdom. Experts feared that the W135 serogroup would gain a foothold in Africa. Convening a consultation meeting in September 2001 in Geneva, the WHO stressed that:
The potentially changing epidemiology of the disease is a prerequisite for taking any decision to reorient the current global policy for preventing and/or controlling epidemic meningococcal disease (OMS 2001, 1).
Neither this call for a rethink of vaccination strategies nor the ongoing pandemic could motivate the MVP to produce a single valence vaccine for Africa. In 2002, an emergency meeting was organised in Burkina Faso, where the epidemic had resulted in 12000 cases and 2500 deaths. The Minister of Health, Alain Yoda, appealed for a vaccine that would provide protection against the W135 strain, but the MVP paid more attention to the Secretary of the Nigerian Health Ministry, Hassane Amadou, and his widely reported plea: ‘Please don’t give us a vaccine we can’t afford. That is worse than no vaccine.’ [3] It was Amadou’s perspective rather than Alain Yoda’s through which MVP’s narratives could be constructed and understood (Thiongane et al. 2017).
The challenge of the public-private partnership was to develop a low-cost vaccine (40 cents a dose) that would protect against serogroup MenA. When they successfully achieved this goal, it made MenAfriVac an exemplar of public- and private-sector collaboration, global health vaccinology, north/south technology transfer, and collaborative regulation via the African Vaccine Regulatory Forum (AVAREF). [4] Promotional materials claimed it would be available to sub-Saharan African countries within five years, but the MenAfriVac vaccine was not rolled out until 2010, first in Niger, Mali, and Burkina Faso, and subsequently in other sub-Saharan countries. [5] Eleven years had elapsed since Niger, the country most affected by the epidemics, had hosted the first conjugate vaccine trials.
Far from being an exception, this vaccine timeline is highly representative of the history of vaccine trials in West Africa. It mirrors, for example, the vaccine trials of hepatitis B in Senegal in the 1980s (Moulin, Chabrol, and Ouvrier 2018). In Niger, a former researcher who had worked as a physician-researcher on the first conjugate vaccine while working at what became in 2002 the Centre de Recherche Médical et Sanitaire [the Centre of Medical and Health Research] observed bitterly:
The clinical trial was suspended because they decided it was not beneficial for them to sell a conjugate vaccine in poor countries. It was the same vaccine as the MenAfriVac, apart from the fact that it was developed for the European market. Because African countries at the time had not negotiated access to the vaccine at a lower price, it took 12 years for the vaccine to be made available in Africa. And it’s still only an A vaccine! What about the other strains? I follow the news on meningitis closely; we are having a W135 epidemic this year. Do we now need to develop a conjugate vaccine for W135, then for C, and so on? You see the position we are in! (Doctor, CERMES, 19 March 2011).
Big pharma business models do not always fit alongside realities of pathogenic variability or with scientific hypotheses (Wallace et al. 2016). Even after having served as the sites of the first vaccine trials, African countries were considered low priority by promoters of the trials (usually pharmaceutical firms based in the Global North). Anne Marie Moulin (1996) wondered how to include and push in the legislation of different countries the legal duties that guarantee the distribution of a future vaccine to the populations who participated in the trial. More than 20 years later, this interrogation is neither a priority for African states nor a consideration for international health agencies. The MVP business model was widely criticised for being less efficient at delivering vaccines to low-income countries than it was at delivering HPV vaccines tailored for rich countries (Wailoo and al. 2010). These vaccines garnered similar levels of attention at the WHO during the same period (Graham 2016).
In 2003, Rino Rappuoli—the head of the vaccine department of the pharmaceutical firm Chiron which had, in the 1990s, developed the first MenA and MenC conjugate vaccine—wrote a commentary in The Lancet responding to an article written by promotors of MenAfriVac. In this piece, Rappuoli asked if the search for alternative solutions could be considered a strategy for accelerating the availability of vaccines in the Global South. He closed his letter: ‘I believe that by trying to reduce the cost to a minimum, the vaccine’s development has been delayed by 3–8 years, which seems a high price to pay’ (Rappuoli 2003, 251). Fundamentally, Rappuioli’s critique was the same one that NGOs such as MSF posed to GAVI: why not advocate or legislate for lowering prices rather than inventing new models designed to develop alternatives that are untested? (MSF 2013).
Five years later, Rappuioli, who had by then become head of the Global Vaccine Research Department at Novartis, returned to his critique, recalling the circumstances under which the first conjugate vaccine was produced. His conclusion was uncompromising: ‘Waiting for the cheapest vaccine was actually more expensive, in terms of lives lost in the interim.’ Rappuioli lamented a ‘beautiful vaccine’ that yielded impressive results during field trials in Niger and the Gambia. However, the group C component of this vaccine was developed for the British market and, Rappuloli recalled, ‘We were asked to remove A,’ which was needed only for Africa—the ‘market was only for C’. Rappuoli argued that instead of trying to reinvent the wheel, the MVP should ‘dust off their vaccine and make it quickly available’ (cited in Roberts 2008).
With a touch of cynicism, Rappuoli called into question the relevance of the business model promoted by the MVP. It is questionable whether a low-cost vaccine supplied by an Indian company to poorer countries in the Global South would prove competitive for big pharma; indeed, I actively question whether the MenAfriVac business plan is really a threat to the highly successful pharmaceutical multinationals in rich countries.
The MenAfriVac roll-out was a gamble. It relied on and reinforced a strategic ignorance based on the total denial of the role that competition between different meningitis pathogens has played in, over the course of many years, triggering ‘two-headed’ epidemics caused by two different strains. The strategy pursued by the MVP had consequences in turn for the availability of vaccines and the increasing privatisation of prevention in Niger.
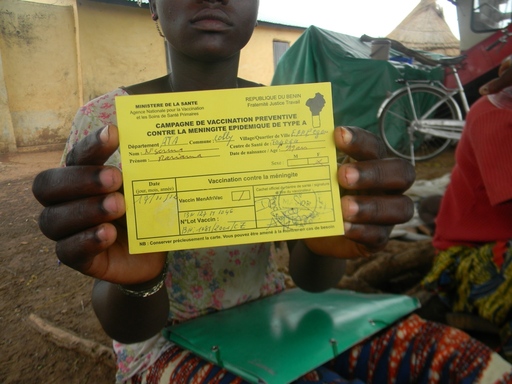
Interrogating the black market for vaccines in times of scarcity
In 2015, five years after MenAfriVac roll-out, a meningitis epidemic struck Niger again. Estimates suggest that more than 8000 people fell ill, and the Centre de Recherche Médical et Sanitaire recorded 573 deaths. The epidemic revealed how unprepared Niger was; a complete lack of vaccines unleashed panic and generated political tension within the National Assembly. The Health Minister was summoned to give evidence to MPs. Schools were closed in Niamey, galvanising fear among the population, which then led to long queues forming from dawn onwards outside the capital’s pharmacies. Biological analysis indicated that MenC was responsible for the epidemic. Shortages of vaccines were first noticed at the national level; in particular, the MenC vaccine was not available in pharmacies. To tackle this shortage, associations and private donors organised vaccine donation drives, targeting in particular prisons and schools.
Niamey’s pharmacists came under pressure to find ways to meet demand, and so began to develop strategies for getting around import laws and for finding new supply chains. Some were able to bring in vaccines from Burkina Faso via personal networks—the vaccines were packed onto buses in cool boxes and then delivered to dispensaries via taxis, a mode of procurement that led to these vaccines being dubbed ‘Mercedes vaccines’. [6] The price of vaccines soared, fluctuating according to demand but rising at certain points to more than 110,000 CFA, or 167 euros. At its highest point the average Nigerien salary would have bought 10 doses of tetravalent vaccine against MenA, MenC, W135, and Y strains.
Families organised themselves into groups to buy in bulk so they could get themselves vaccinated by pharmacists or private nurses. In April, batches of vaccines were recalled by a mayor in Niamey following the circulation of rumours about the quality of the vaccines. The recalled products were deposited at the Niger Direction de la Pharmacies et de la Médecine Traditionnelle (DPHMT), where they were deemed fakes as the vials contained 50 doses, a packaging quantity that had been changed years before. This discrepancy suggested that the vaccines had been manufactured by GlaxoSmithKline (GSK). The head of the DPHMT raised the alarm and sent photographs of the vials to the World Health Organization (WHO) in Geneva. Samples were then sent via DHL to the WHO, where they were analysed. The WHO immediately published a briefing on the circulation of counterfeit vaccines in Niger.
Events took a dramatic turn when the Nigerien government warned against vaccines delivered and administered in pharmacies. Many Nigeriens interpreted this intervention as an attempt on the part of Western countries to restrict access to the ‘Burkinabe vaccine’, thereby generating more profit for the vaccines from Europe, which were expensive. In fact, the introduction of MenAfriVac resulted in the drying-up of the stock of MenA and MenC vaccines and a loosening effect on epidemic preparedness.
As the state struggled to maintain the supply of vaccines, citizen-led organisations stepped into the breach and opportunities for speculation on the black market were rife. In 2017, there was another outbreak in Niger, once again caused by strain MenC. This time, the WHO was forced to issue warnings about the circulation of polysaccharide vaccines, whose packaging claimed they had been made by the Bio-Manguinhos/Fiocruz laboratory. The Brazilian laboratory contacted the WHO to confirm that they did not in fact make the polysaccharide meningitis vaccines circulating in Niger. This falsification (and the truth about the quality of the drugs involved) was not made public. [7]
The meningitis outbreaks of 2015 and 2017 illustrate the ongoing privatisation of vaccination (before 2015, emergency vaccination was handled by the state and NGOs, and vaccines were free) while at the same time showing how scarcity led to the emergence of alternative-access models. The commodification of vaccines is the consequence of short-term thinking in vaccine policy and of the partial answers provided by public-private partnerships (PPPs).
The objective of the Meningitis Vaccine Programme (MVP) was to integrate progressively MenAfriVac into the WHO’s Expanded Programme on Immunisation. However, during my interviews in Senegal, the president of the vaccine advisory committee criticised the pressure to introduce MenAfriVac and confirmed that, in Senegal, there was some doubt as to whether MenAfriVac was necessary. [8] Nigeria has classified the vaccine as ‘less protective’, and saw it as a stopgap before the arrival of a multivalent vaccine (Howard et al. 2018). MenAfriVac is part of the category of ‘intermediate’ vaccines, emblematic of modern vaccinology and the era of the establishment of the Global Alliance for Vaccines and Immunization (GAVI). These intermediate products are technologies of waiting , or provisional foresight , an idea borrowed from Niklas Luhmann (1998). They are placeholders whose necessity is derived not from their epidemiological efficacy but from their role in shaping a market in the Global South and in the broader neoliberal project of vaccinology (Rajan 2005).
Viewed in this light, the MVP is the crowning achievement of a policy of accelerating vaccine production and vaccination that fails to take into account questions of access and cost. It is an unambiguous failure. Furthermore, the project is the outcome of the proliferation of highly unequal vertical models characteristic of the current neoliberal agenda shaping global health (Kerouedan 2013). Atlani-Duault and Vidal (2013, 11) were correct in claiming that this agenda ‘emphasizes the importance of having the capacity to respond to emergencies, in particular epidemic outbreaks, while the long-term social impact of programmes is not taken into consideration, let alone the structural transformation of health systems in the Global South’.
Conclusion
The Meningitis Vaccines Project (MVP) is indicative of the relentless pursuit of the immunisation agenda—set in the early 2000s by pharmaceutical companies and the Global Alliance for Vaccines and Immunization (GAVI)—that presented vaccine products as miracles that should rapidly solve any challenges posed by actual and future epidemics. The introduction of improved and new vaccines, in this ideological context, is at the service of a particular agenda: the globalisation of vaccinology. However, the means to meet this goal seem to be putting unprecedented pressure on the health systems of the poorest countries while failing to implement efficient vaccination projects capable of combating health inequities.
Acknowledgements
I want to express my deep gratitude to Dr Branwyn Poleykett, who translated this text from French, and to MAT ’s editors for their comments on the draft version of this article. Many thanks also to LASDEL researchers in Niamey for all the inspiring discussions. Part of this research is founded by the Maison des Sciences de l'Homme, Paris North (Grant 15/2.6.6, axis of research Space Environment and Health). I am thankful to Research Assistant Djibrillou Arimi of the University Abdou Moumouni of Niamey (Niger), who performed the press review.
About the author
Oumy Thiongane is a medical anthropologist working at CIRAD (Agriculture Research Centre for International Development), France, and a research associate at Dalhousie University, Canada. For 10 years, she has been studying epidemics and neglected tropical diseases (NTDs) in West Africa. Her current research focuses on the use of data sciences and the digitalisation of health as part of European Union-sponsored health surveillance systems. She is also currently preparing an ethnographic book on epidemics and vaccine transformation in West Africa in the 2000s.
Footnotes
-
A designation used by epidemiologists, the ‘belt’ extends from Senegal to Ethiopia between the eighth and 16th parallel, overlapping with the annual rainfall isohyets of 300mm in the north and 1,100 in the south. The belt brings together Sahelian countries, with Niger as the epicentre. ↩︎
-
This combative position vis-à-vis the dictates of the pharmaceutical industry would leave him side-lined in the important meetings to come, where decisions were made about meningitis vaccination. He made this clear in two conversations I had with him in Cotonou in October 2010 and Paris in January 2012. ↩︎
-
Marc Laforce repeated this request several times in press material for the MVP. See also the discussion in Roberts (2008). ↩︎
-
Margaret Chan mentioned MenAfriVac in her final speech to the WHO in May 2017. See the full speech: https://apps.who.int/iris/bitstream/handle/10665/274658/A70_3-en.pdf?sequence=1&isAllowed=y . ↩︎
-
The campaign targeted 25 countries and around 300 million Africans. ↩︎
-
Hassane Moussa Ibrahim, a researcher at LASDEL, brought this popular categorisation to my attention during an interview about the politics of the epidemic in the municipality of Dosso, 130km from Niamey in Niger. ↩︎
-
In September 2017, an inquiry was announced into the fake vaccines. We do not yet know who will be involved in the inquiry. ↩︎
-
Although it was a test site for MenAfriVac, Senegal has low rates of meningitis; additionally, W135 is the primary strain in Senegal, not A. ↩︎
References
Atlani-Duault, Laëtitia and Laurent Vidal. 2013. ‘Le Moment de la Santé Globale’. Revue Tiers Monde 215: 7–16. https://doi.org/10.3917/rtm.215.0007.
Biehl, João, and Adriana Petryna. 2013. ‘Interventions. Overview ‘. Biehl, João, and Adriana Petryna (eds). When People Come First: Critical Studies in Global Health . Princeton, NJ: Princeton University Press. 133–140.
Campagne, Gerard, Amadou Garba, Pascal Fabre, Anne Schuchat, Robert Ryall, Denis Boulanger, Mike Bybel, George Carlone, Philippe Briantais, Bogdan Ivanoff, Bertrand Xerri, Jean-Philippe Chippaux. 2000. ‘Safety and Immunogenicity of Three Doses of a Neisseria Meningitidis A+ C Diphtheria Conjugate Vaccine in Infants from Niger’. The Pediatric Infectious Disease Journal 19 (2): 144–50. https://doi.org/10.1097/00006454-200002000-00013.
Chippaux, Jean-Philippe. 2001a. ‘Meningitis Epidemics: A Foreseen Disaster’. Médecine Tropicale : Revue Du Corps De Santé Colonial 61 (2): 137–38.
Chippaux, Jean-Philippe. 2001b. ‘Conflits Autour de la Méningite en Afrique’. Le Monde Diplomatique 22B–22B.
Gaudillière, Jean-Paul. 2016. ‘Un Nouvel Ordre Sanitaire International ?’ Ecologie Politique 1: 107–124. https://doi.org/10.3917/ecopo1.052.0107.
Graham, Janice. 2016. ‘Ambiguous Capture: Collaborative Capitalism and the Meningitis Vaccine Project’. Medical Anthropology 35 (5): 419–32 https://doi.org/10.1080/01459740.2016.1167055.
Guilbaud, Auriane. 2015. ‘Les Partenariats Public-Privé Sanitaires Internationaux: Diffusion et Incarnation d’une Norme de Coopération'. Mondes en Développement 2: 91–104. https://doi.org/10.3917/med.170.0091.
Howard, Natasha, Helen Walls, Sadie Bell, and Sandra Mounier-Jack. 2018. ‘The Role of National Immunisation Technical Advisory Groups (NITAGs) in Strengthening National Vaccine Decision-Making: A Comparative Case Study of Armenia, Ghana, Indonesia, Nigeria, Senegal and Uganda’. Vaccine 36 (37): 553643. https://doi.org/10.1016/j.vaccine.2018.07.063.
Kerouedan, Dominique. 2013. ‘Diplomatie de la Santé Mondiale’. Santé Publique 25 (3): 253–253. https://doi.org/10.3917/spub.253.0253.
Luhmann, Niklas. 1998. Observations on Modernity. Stanford, CA: Stanford University Press.
Moulin, Anne-Marie. 1996. ‘L’aventure Humaine de la Vaccination’. Moulin, Anne-Marie Moulin (ed.). L’Aventure de la Vaccination . Paris: Fayard, 11–37.
Moulin, Anne-Marie, Chabrol, Fanny, and Ashley Ouvrier. 2018. ‘Histoire d’un Vaccin pas Comme les Autres: Les Premiers pas du Vaccin Contre l’Hépatite B au Sénégal’. Delauney, Valérie, Alice Desclaux, and Cheikh Sokhna (eds). Niakhar Mémoires et Perspectives: Recherches Pluridisciplinaires sur le Changement en Afrique . Marseille et Dakar: L’harmattan & IRD Editions, 489–510.
MSF. 2013. The Right Shot: Extending the Reach of Affordable and Adapted Vaccines . Web. Lausanne. http://www.msfaccess.org/sites/default/files/MSF_assets/Vaccines/Docs/Vaccines_Report_Right-shot_FR.pdf.
OMS. 2001. ‘Emergence de la Méningococcie W 135’. Rapport d’Une Consultation de l’OMS Genève . 17–18 September. Genève.
Rajan, Kaushik Sunder. 2005. ‘Subjects of Speculation: Emergent Life Sciences and Market Logics in the United States and India’. American Anthropologist 107 (1): 19–30. https://doi.org/10.1525/aa.2005.107.1.019.
Rappuoli, Rino. 2003. ‘The Real Cost of an Affordable Vaccine for Meningococcus A’. The Lancet 362 (9379): 250–251 https://doi.org/10.1016/S0140-6736(03)13929-3.
Rimbaud, Arthur. 1999. Poésies. Une Saison en Enfer. Illuminations . Paris: Gallimard.
Roberts, Leslie. 2008. ‘An Ill Wind, Bringing Meningitis’. Science 320 (5884): 1710–1715. https://doi.org/10.1126/science.320.5884.1710.
Storeng, Katerini T. 2014. ‘The GAVI Alliance and the ‘Gates Approach’ to Health System Strengthening’. Global Public Health 9 (8): 865–879. https://doi.org/10.1080/17441692.2014.940362.
Thiongane, Oumy Baala. 2013. Anthropologie de la Méningite au Niger : Espaces épidémiques, Mobilisations Scientifiques et Conceptions de la Maladie . Paris: Ecole des Hautes Etudes en Sciences Sociales.
Thiongane, Oumy, Janice Graham, and Hélène Broutin. 2017. ‘Lueurs et Leurres de la Santé Globale. À Propos de MenAfriVac®, un Vaccin “Africain” Contre la Méningite’. Anthropologie & Développement 46 (47): 213–234. https://doi.org/10.4000/anthropodev.607.
Wailoo, Keith, Julie Livingston, Steven Epstein, et Robert Aronowitz. 2010. Three Shots at Prevention: The HPV Vaccine and the Politics of Medicine’s Simple Solutions . Baltimore, MD: Johns Hopkins University Press.
Wallace, Robert G., Richard Kock, Luke Bergmann, Marius Gilbert, Lenny Hogerwerf, Claudia Pittiglio, Raffaele Mattioli, and Rodrick Wallace. 2016. ‘Did Neoliberalizing West African Forests Produce a New Niche for Ebola?’ International Journal of Health Services 46 (1): 149–165. https://doi.org/10.1177/0020731415611644.