Fat, in the context of dissection, is a nuisance, an obstruction to anatomical order and orientation. Yet it makes up a large part of the human body, and in the practice of dissection becomes one of the most prominent materials in the room, as it sticks to gloves and spreads through the dissection hall, making chairs greasy and instruments slippery. In this article I explore the role and significance of fat tissue in anatomical dissection for medical students. In anatomy, fat remains largely an excess material; something superfluous, insignificant, left-over when the body is turned into an anatomical body consisting of muscles, nerves, blood vessels, and bones, cleaned and displayable. But fat is also something which appears in experience as excessive, omnipresent, proliferating, and resistant to attempts to keep it in order. Much anthropological work within dissection practices has described the process of ‘cleaning’ the bodies, but often—mirroring medicine—these accounts follow the becoming of the anatomical body and leave the fat behind. In this article, I try to ‘stick with’ the fat and suggest that fat tissue, as an embodiment or material manifestation of the more-than-anatomical-body, may tell us something about bodies, subjectivity, scientific order, and dissection.
Sticking with the Fat
Excess and Insignificance of Fat Tissue in Cadaver Dissection
—
Abstract
Introduction
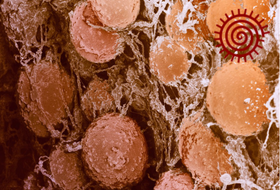
The human body is full of fat, and this is not just the case for bodies we might call ‘fat’—all bodies have fat: in layers of subcutis beneath the skin; in the in-between spaces of muscles or organs; around joints; behind the eyes. Fat sprawls through the body as energy storage, insulation, shock absorber, and endocrine organ (Scanlon and Sanders 2015, 89).
Recent years have seen an increased biomolecular interest in fat tissue, particularly in its metabolic and endocrine features, and it is primarily from this interest that it has gained status as an organ (e.g., Coelho, Oliveira, and Fernandes 2013). In gross anatomy, however, fat tissue, or adipose tissue, is classified as a type of connective tissue (e.g., Shier et al. 2012, 104; Scanlon and Sanders 2015, 89), the ‘stuff in between’. Fat is typically ascribed only a short section or a few lines in anatomy books and teaching material; mostly left nameless or named en masse depending on its broad location, such as subcutaneous, visceral (around organs), intramuscular, or perivascular fat. In anatomical dissection, as I will show, fat is quite literally positioned as that which needs to be removed in order for anatomy to appear. That is—as manifested in anatomical drawings—fat remains at best in the margins of human anatomy: a few millimetres of yellow between the skin and the muscles (see examples in Pond 2017, Figure 1).
The term ‘fat’ is somewhat equivocal, designating multiple things: a chemical category/dietary component, a type of bodily tissue, and a bodily form, and it carries heavy normative connotations (Hardy 2013). In cultural studies, fat—particularly in its association with large bodies—has received much attention and been debated for its normative and political symbolic significance. For example, Jana Evans Braziel and Kathleen LeBesco have argued that there is a need to ‘unmask’ the fat body, to ‘render it visible’ in new ways, and intervene in what they describe as a fixed discourse (Braziel and LeBesco 2001, 1). Taking a slightly broader approach to fat, Christopher Forth traces its cultural history, both in the sense of large human bodies and of oily resource, noting the symbolic as well as the material resistance fat poses to desires of domestication and control (Forth 2019, 276). The literature is rich in examples of this cultural approach (e.g., Gilman 2008; Cooper 2010; Forth, Leitch, and Murray 2014). Mirroring the medical lack of interest in fat in the context of gross anatomy, however, fat tissue has received very little attention in anthropological research on medical science and dissection practices, compared with politicised notions of fat and ‘fat’ that is tied to bodily forms and dietary practices. Indeed, in my search for literature I found only one qualitative study (mixed methods) which dealt explicitly with a potential effect of the work with fat in dissection (Goss et al. 2020).
Motivated by a curiosity about what we might learn if we focus on fat tissue, this piece takes the initial steps of such an exploration by drawing attention to fat as it is encountered by medical students in anatomical dissection. In particular, I explore a materially focused analysis of fat, as a sticky, blubbery mass, which is literally ‘left behind’ in the making of anatomy, and the ways in which it becomes a manifestation of relations between abstracted order (anatomy) and a concrete messy reality (human bodies)—relations which have been the topic of much scholarship the past 50 years or more (e.g., Latour 1993; Mol 2002; Rheinberger 2010).
I aim to convey not just observations about the symbolic role of fat, but a sense of the dissection space and the way in which fat—even if not the focus of the activities—spread and encroached on students, taking up a prominent position in their experience despite its anatomical insignificance. To fulfil this aim, I draw on both autoethnographic experience and observations and conversations with students, as we—myself, the students, and the bodies for dissection—became materially entwined through the proliferation of grease. The emphasis is on providing a sense of material encounters, and to think through and with fat: about bodies, subjectivity, scientific order, and dissection. I want briefly to remark here that while I take a material approach to fat tissue, and to the bodies in the dissection hall, this should not read as a lack of acknowledgement of the persons whose bodies were being dissected, nor as a neglect of the subjectivity that was still tied to these liminal bodies. Focusing on the materiality of fat is not meant as a reductionist stance on fat as a decoupled thing or object. Rather, the retained subjectivity in the fat of the dissection hall is an important element of its material power. As Merleau-Ponty’s (2005) work on embodiment shows repeatedly, materiality is not opposed to persons; we are and live bodies, and bodies are material.
The field: Fat in the dissection hall
During spring and autumn 2019, I conducted ethnographic fieldwork at
an anatomy course for undergraduate medical students at the University
of Copenhagen in Denmark. The fieldwork was part of my PhD studies on
the role of the body in medical practice and for what I discuss in this
article the main field site was the dissection hall. However, as already
skilfully described by Elisabeth Hallam (2020), settings of teaching
anatomy stretch across multiple spaces and include an assortment of
bodies: biological specimens and bodies (cadavers, prosections, and the
students’ own bodies as they investigate each other); images and texts
in anatomical atlases (both on paper and in 3D-apps); plastic and
porcelain models; radiological imaging (e.g., MRI or X-ray); and even
YouTube videos, not to mention the multiple metaphors and analogies
employed to convey anatomical knowledge. All of these co-constitute and
mutually bring about a sense of the ‘medical body’ (as an abstract,
composite concept) which students study. For most of these ‘partial
bodies’ in anatomy, fat is either literally left out (e.g., from models
or many anatomical drawings) or consigned to the margins (e.g., in
physical specimens) with none of the indicator pins, stickers, lines,
squares, or coloured string and rubber bands that point out and
delineate muscles, glands, blood vessels, and so on (see Figure 1). This
all provides material manifestations of the neglect or even erasure of
fat tissue as anatomically relevant. For the sake of this article, I
focus on one type of body in which the encounter with fat is  unavoidable, namely the
cadaver for full body dissection.
unavoidable, namely the
cadaver for full body dissection.
Figure 1. Anatomical specimens with coloured pins to mark muscles, nerves, and other anatomical structures. Photo from The Body Collected exhibition, Medical Museion, 2016.
During fieldwork I followed two rounds of the anatomical dissection course which makes up part of the course in anatomy of the head, neck, and musculoskeletal system. The anatomical dissection course stretches across eight non-consecutive days over a month, which are punctuated by lectures, group work, ‘clinical anatomy’ (i.e., live body anatomy where students examine each other), and endless hours recapitulating and preparing topics in the ‘wet’ and ‘dry’ study halls.[1] I walked around freely, having been invited by the head of the donation programme, who was held in high esteem by both staff and students. In the dissection hall he introduced me to the students, and I was dressed in a blue university laboratory coat, which all signalled my belonging in the hall. Sometimes I would walk from workstation to workstation to see different approaches; sometimes I would sit with a group of students for an extended period of time (e.g., 30–40 minutes), asking them questions about what they were doing, or more abstract questions about how they perceived their activities. Sometimes the students would ask me to help—to pick up a book, pull back a sleeve, hold the scissors. Sometimes they would spontaneously begin narrating their activities, call me over, or beckon me in closer to show me something, occasionally offering me a glove so I could touch this or that structure to feel its texture or weight. When this happened, I was always a little taken aback by the coldness of the dissection bodies. For the spring semester class, I also spent time following many of the students’ other activities, often joining them, for instance, in the two study halls, sitting with them for hours as they practised their Latin glossaries, shared snacks, talked about weekend plans, and complained about the long hours. Although the group of students was rather large (approximately 280 students per semester), most of the students knew who I was by the middle of the course. They asked curiously about my project and sometimes came to fetch me if something they considered relevant for me was happening while I was somewhere else. The spring class and I also shared the experience of entering the dissection hall for the first time.
The bodies used for anatomical dissection are donor bodies,
voluntarily donated before death to science and education. They are real
bodies, bodies that have lived. Thick and thin, old and young, worn,
‘repaired’ or sick bodies—all are welcomed. In order to donate your
body, you must make, and have legally validated, a last will and
testament, and you must be 18 years of age to sign such a will. Other
than that, there are no requirements. Once the donated bodies enter the
university, they undergo different procedures depending on their future
use. Bodies for the medical students’ use are preserved with
formaldehyde and alcohol to ensure safety from infection, as students
are not used to holding scalpels or cutting into flesh and might make
slips and cut themselves. These preserving substances give the bodies a
strange waxy colour, but also allow some hindrance of decay during the
month that the course lasts. However, they do not prevent a smell of
sour-sweet decay creeping in as the days pass by.[2]
During the dissection course, students are split into two teams, working
on opposite sides of the cadaver—one team in the morning, and one team
in the afternoon. Each team divides further into pairs working
simultaneously on different zones (such as seen in Figure 2: the head
and neck region, example marked as ‘zone 1’; the upper torso and
extremities, marked as ‘zone 2’; and lower torso and extremities, marked
as ‘zone 3’). Every second course day the students rotate in order to
get acquainted  with the
different areas of
the body.
with the
different areas of
the body.
Figure 2. Image from the dissection hall before dissection starts, showing tables with bodies, the yellow buckets, and (behind the air extraction pipes) decorations by Poul Gernes. Photo courtesy of Maria Olejaz, 2014.
When I first decided to undertake fieldwork in a dissection hall, I read Maria Olejaz’s work on practices of dissection in Danish universities, and prepared myself for the anticipated ethical complexity and existential conversations with students and staff (Olejaz 2020). I also imagined my fieldwork would involve overcoming revolting smells and less-than-pleasant confrontations with death, decay, and human remains. What I did not expect, and I shared this surprise with many of the students, was the messiness and physicality of dissection, and the role that fat tissue played as a materialisation of this. The sense of fat tissue spread throughout the dissection hall and its materiality haunted me in coffee breaks, when the handle of a coffee pot in the adjacent break area felt slightly greasy in my hands, and my immediate—neurotic—association was whether this might stem from the dissection hall. Fat was both a source of annoyance and of disgust: it got in the way of making the bodies appear neat, made instruments slippery, demanded hours of meticulous, repetitive, and slow labour; it made its way in small pieces onto the clothes of the students, even beneath their lab coats, and clogged the drains of dissection tables, keeping (other) materials such as fixation fluids or residue faeces from the intestines from finding their proper way off the working station. Going over my field notes from the dissection hall, fat was one of the most prominent themes: the students talked about it, I wrote repeated notes about it, it seemed to be everywhere.
Cutting into the flesh
In order to contextualise fat, let me take you through the activities of the dissection hall. The dissection course is held in a large hall specifically designed for the purpose and located in the basement of the university. You arrive there by walking through long hallways and passing through several heavy doors. As you enter the general area, you are met by colourful wall decorations by the well-known Danish artist Poul Gernes. You need a bit of beauty and colour around you when working in a place like this, as the head of programme told me on my first day there. When you get close to the hall itself, A0-size posters from Andreas Vesalius’s De Humani Corporis Fabrica Libri Septem (1543), with anatomical bodies elegantly posing, add another layer of artistry to the room’, and you start to perceive the sweetish smell of human specimens. In the dissection hall, the first surprise is the daylight; this room is built so that natural light streams down through one-way glass in the ceiling. We may be in the basement, but there is nothing covert about it. The sense is clinical rather than clandestine, as one student remarked, smiling at his own inexplicable expectation of the latter. Approximately 25 tables are lined up in two rows with three to four metres between each, and bodies lie ready, covered in white plastic sheets. There is a general buzz as anxious and excited students find their correct place. Sounds are loud and hard to differentiate, as sound waves bounce off the tiled walls and metal surfaces of the hall. Before dissection starts, the head of the programme gives an introductory speech: about practicalities, about the donors, about ethics, respect, and about the potential difficulty or awkwardness that students may experience. In the semesters when I joined them, he ended by referring to me, adding that I was there doing fieldwork and had been allowed to do so. The dissection hall is not a place where strangers are free to come and go. After this short speech the students can begin.
 Figure 3. Vein
being
exposed from the subcutaneous layer of fat using an inverse scissors
method. Source: Still from exhibition film ’Dissection’, The body
collected exhibition, Medical Museion, 2016.
Figure 3. Vein
being
exposed from the subcutaneous layer of fat using an inverse scissors
method. Source: Still from exhibition film ’Dissection’, The body
collected exhibition, Medical Museion, 2016.
The first step of anatomical dissection is to make a very fine cut
through the skin. Students are told repeatedly that it should not be too
deep, as they risk destroying important structures they cannot see
underneath the skin if they cut anything more than merely the one
millimetre which allows you to go through the body’s barrier. Many
students are hesitant about making this first cut. They spend up to 15
minutes discussing how to go about it, pointing, checking with
instructors if they are doing it right, and once they finally make the
cut they do so slowly. The cut is made in the shape of three sides of a
rectangle, leaving the last side untouched, so as to create a flap of
skin that can be folded to the side and then placed back at the end of
the session to protect the body while it waits for the students to
return a few days later. After this, the work of separating the skin
from subcutaneous fat begins. This is delicate work which requires focus
and technical skill. Students are told that they must take care to
separate the layers with their scalpels without cutting into either the
skin—as they will destroy the protection it offers—or the underlying
tissue, the contents of which they cannot yet see. Again, emphasis is
put on the risk of inadvertently destroying important anatomical
structures. Some students do it well, some not, you can tell which by
looking at the flap of skin as it slowly works its way out to the side:
it should not have any fat tissue on it. While they work at this, the
tenseness and hesitation slowly fade, replaced by the level of
concentration demanded for this challenging labour. After considerable
time and effort, students can fold back the flap of skin, and—if they
have done their job properly—they can now look at a more-or-less
structureless surface of yellow fat (see bottom right part of the cut
depicted in Figure 4). Briefly, the integrity of the fat counts as
reassurance that the anatomy remains intact. Then the next task begins:
removing the fat without destroying its hidden treasures, namely those
 ’important structures’
that
the students are all here for (i.e., the anatomy).
’important structures’
that
the students are all here for (i.e., the anatomy).
Figure 4. Illustrating the flap of skin folded to the side and anatomical structures exposed underneath (no trace of fat tissue). Lithograph by G.H. Ford. Dissection showing the contents of the axilla (1867). Image courtesy of the Wellcome Image Collection.
At this point, students are asked to put away their scalpels: there is to be no cutting into tissue where you cannot see what is hiding out of sight. Some instructors tell their students to use their hands. They show the students how to create an opening by poking into the fat tissue, then use their fingers to loosen it. This way, students will be able to feel any structures hidden in the fat—and maybe even find some of the small subcutaneous nerves, as instructors explain with an air of promise and respect for any who manage this difficult task, given how delicate and hard to see these are. Other instructors show their students how to use scissors in a strange reverse way, not cutting but rather expanding tissue by pushing in the scissors in a closed state, opening them once they are deep in the tissue, pulling tissue apart rather than cutting it. While all this pushing and pulling looks surprisingly volatile and requires a degree of manual force not present in the previous tasks, both the students and I—equally surprised by this—gradually learn that the forceful, physical engagement with the bodies, in a process referred to as ‘blunt dissection’, protects structures and causes less harm than the seemingly delicate, controlled cut of a scalpel. Irrespective of how the students work (by hand or inverse scissors) it is a laborious process that demands a balance between the physical effort of removing fat and careful attentiveness not to accidentally remove something else, before anatomical structures—the targets of today’s session, as written down on students’ lists—show up as recognisable. That is, at this stage and for the rest of the dissection, fat plays the ambiguous role of both insignificant and major obstacle. It is a material that ‘hides’ the important stuff: the anatomy. While it needs to be removed for the anatomical structures to appear, students still need to treat it with some care. On several occasions I watched students learn this lesson the hard way, realising—after spending hours searching for a structure (often a vein or a nerve)—that their efficiency in fat removal had effectively robbed them of the structure they needed to see, and much of their work would be lost. One student, for example, told me that until he had accidentally removed a very important structure in the neck without even noticing it, he had not fully grasped how easily something vital could be missed, and how important it was to know thoroughly all the details of the anatomy (specifically in this case, the layout of blood vessels and nerves) when cutting into human beings.[3]
Fat and the anatomical body
Fat, then, is something with which the students have to engage with a certain gentleness, at first even protectiveness, not for its own sake but for its treachery, its devious covering over of ‘vital’ nerves and veins. It is not counted as significant for the curriculum, and yet it requires hard physical labour and bodily engagement.
On my first day in the field—also the first day of dissection for the students—I witnessed and noted down the following scenario:
Two students are working with the subcutaneous fat of a corpse. They are told that they should use their fingers to loosen the fat. One of the students (a female in her early twenties dressed in a white coat and wearing rubber gloves) pushes her finger in under the fat—she has to put some force into the push to make the hole big enough to get a finger in—and leans her head back, away from the body, in aversion. She then uses only two fingers to loosen the tissue (the index and middle finger), and the three other fingers are pointing straight out into the air—attempting to escape contact with the body. Her study partner suggests she puts down the scalpel, so that she won’t hit someone with it—she still holds it in her other hand and is clearly not paying attention to what she is doing with this part of her own body. ‘This feels so disgusting’, she says (partly to me, partly to her partner), ‘I am literally standing putting my finger into a person’.
She gets hold of something different (that is, not fat) and moves in a little closer. ‘Oh look, it’s a nerve’, she says. She starts using both hands to get it fully exposed. The muscle structure underneath starts to appear. Now both students have their hands in the body while they are discussing which anatomical structures they will find. ‘Wow, it’s starting to stick, this stuff’, says the female student, and smiles, referring now not to the fat tissue but to the Latin names for structures that the students must remember. Still her hands in the body.
During the approximately ten minutes within which this played out, several changes happened in the approach of the student to the body. First, the physical engagement required of her in fat removal—her contact with the body no longer mediated by an instrument—overwhelms her: she forgets everything else around her, even the sharp knife in her other hand, and signals aversion with every bit of her own body. Then, after a while, she gets hold of something in the fat tissue—a definable structure—and her body posture changes: she leans in, and her partner joins in also. This is what they came here for (the curriculum): they have found ‘something’ and can now start deciphering its exact name and category. Even if fat here provides the actual occasion for physical (intercorporeal, if you will) engagement of student and donor body, it is only with a definable structure (anatomy) that the student engages wholeheartedly. Conversely, this curious engagement with definable anatomy seems to obscure the part of the contact as marked by human-to-human interaction—the fact of the student ‘having her finger in another person’.
As days go by, the bodies change. The students remove fat and other connective tissue, so that the anatomical structures become clear; the bodies are transformed from personal bodies to scientific anatomical bodies made up of bone, muscle, nerves, and vessels in what T. Kenny Fountain calls a ‘process of making through unmaking’ (2014, 122). The practice of the students thus becomes a repetition of the contrast between fat and anatomy—shaped partly by the material treachery of the fat, partly shaping and constituting this same treachery of materiality through positioning it as insignificant (i.e., disposable). The unmaking of the body simultaneously creates anatomical bodies and establishes fat—a type of tissue that is present in all human bodies—as being a material in excess, something insignificant at best, which we should get rid of. As pointed out by Daniel Miller (2005), materiality both shapes and is shaped by practices: dissection, as a material practice, is not only shaped by, but also shapes, fat as we encounter it.
This contrast between fat and anatomy is established in multiple ways in the dissection hall. Towards the end of the first day of dissection, an instructor walks past a table which I am sitting next to, and notices a muscle is missing from the body laid on it. He asks who is responsible. A student responds to the instructor, explaining that they removed it in order to reach the layer underneath, but that they ‘put it in the bucket’. During dissection the integrity of the donor body is sustained through meticulously keeping track of the material of each body as it is taken apart. Students are instructed to transfer any tissue removed from the body into a yellow bucket placed at the end of each table (see Figure 2 above). After the course ends, each body is collected and returned to the specific coffin in which it originally arrived, to be buried or cremated according to the wish of the deceased.[4] While students are told to remove fat tissue (and, to some degree, tendons and membranes) and place it in the bucket, they are given strict instructions not to remove any of the ‘anatomical structures’ from the body. The instructor who stopped by the table reprimands the student, stressing that ‘only fat’ should go in the bucket; the anatomical structures are important for the next team of students working in this area (once they rotate) to be able to orient themselves in the body—they (i.e., anatomical structures already located and ‘cleaned’) are an essential part of the anatomical map and should not be removed. Skin must remain to be folded back over at the end of the day, and any anatomical structures (muscles, veins, arteries, nerves, ligaments, and to some extent bones) that get in the way of further dissection must be cut in one place only, in a manner that indicates how to place them back in their original position, so as to allow for them to be folded to the side like the skin.
What I have described so far aligns with multiple other descriptions of dissection (e.g., Prentice 2013; Fountain 2014; Hallam 2016; Olejaz 2020), perhaps emphasising fat tissue slightly more, but not recounting anything of radical difference. However, at this point most scholars move on to talk about the anatomical body and leave the fat behind—much like the medical students do—noting perhaps the symbolic role of its removal. Here, I want to stick with the fat to see what observations we may make from this strange material.
Excess: Unctuous omnipresence and anatomical insignificance
Contrary to my pre-dissection ideas, fat tissue is neither a well-defined, self-contained layer between the skin and ‘all the rest’, nor is it even a homogenous mass. Rather, fat is ‘lobular’, proliferating in small droplets or cells throughout the body. As explained to me by a student: ‘When you speak of something lobular, you should think raspberries [pauses for a while before adding]: that is, structure-wise, not other things about raspberries. You shouldn’t think about those’. If fat tissue is scarce in a place—such as in the neck region—and the structures the students are looking for are small, the work may consist in removing individual ‘droplets’ of fat with tweezers in order to ‘clean’ the area to have a proper overview. Students collect small piles of fat tissue on the table next to the body or place the surplus tissue in a metal bowl. If fat tissue is more abundant, it comes off in bigger lumps, quivering as it lets go of the body; it is structured a bit like Styrofoam, only heavy and wet. When students have finished their current task, or need a break, they transfer their piles or the content of the metal bowls into the yellow bucket. While, as we have seen, the fat is almost the only tissue that is supposed to go in the bucket, its sticky, lobular structure resists a straight path there. It sticks to gloves and instruments in small, persistent pieces that are not easy to shake off. Sometimes, when the manual force demanded to loosen it is not properly calibrated, it jumps off the body, and into the hair of the students or even onto their cheeks, setting about a brief moment of panic. Students rub their gloves together when they ask me to fetch something, demonstrating the greasy layer, which has also spread across their workstation and made instruments slippery. Marks of grease from the liquid that comes off the bodies seep through the sleeves of the students’ white coats and the notes that they bring into the room, remaining as stains once aqueous elements of the liquid have long evaporated or been washed out. Even without my touching the bodies, these stains reach me with their greasy mark: when I help students adjust air extraction pipes or raise the seat on one of the metal chairs, surface grease transfers to my skin and ends up as stains in my field notebook.
A perhaps obvious analytical concept to invoke here, to help make sense of the role of fat in the dissection hall, is Mary Douglas’s notion of ‘matter out of place’. To Douglas, ‘matter out of place’ summarises how materials can come to be considered dirty or invoke disgust through being improper to their context, and by so being obtain pollutive powers—that is, the power to make dirty through contact (Douglas [1966] 2003). The notion comes up in cultural studies of fat and fat bodies. Fat, for example, is referred to as matter-out-of-place—or as bodies out of bounds (Braziel and LeBesco 2001)—in relation to ‘an ordered cultural system of ideas and images about health and beauty’ (Forth 2019, 8, referencing Douglas [1966] 2003). That is, fat is that which should be removed to become ‘healthy’ (with all the cultural connotations that this word entails).[5] As pointed out by Goss et al. (2020), ideas of fat related to health are not absent from the dissection hall, and students do talk about the size of cadavers in relation to health—although this also applies to particularly ‘skinny’ cadavers, about whom it is assumed that they must have been very ill leading up to their death.
For the focus here—on a more concrete unruliness of fat as a salient material aspect of dissection—‘matter out of place’ is relevant as a term that helps deepen our understanding of fat as a materialisation of the ‘messiness’ and physicality of dissection, as described in the beginning of this article. That is, I invoke this notion in particular for its inclusion of ‘matter’ and ‘space’ as decisive elements in establishing appropriateness. It is worth mentioning that Douglas’s notion is often criticised for reducing notions of dirt to the consequence of fixed social structures, and it may be argued both that dirt is not merely a social matter, and that social matters are far more fluid and plastic than Douglas acknowledges. Megan Warin makes this point specifically in referencing Douglas to make sense of the pollutive power of fat (Warin 2003, 82). However, in dissection, the fat becomes surplus to requirements and a source of annoyance and disgust exactly in relation to a rather fixed system—namely, the atlas order of the anatomical body, and the clear dissection practice guidelines, set in place to manage the integrity of student and donor bodies.
Fat is ‘out of place’ in relation to the atlas order in the sense of keeping bodies neat: producing well-ordered, easily navigated anatomical bodies. Any remaining fat in the bodies becomes dirt, or perhaps rather impurity, as it obscures the targeted structures and disrupts (anatomical) orientation. That is, fat, as something which is spread throughout the body but has no anatomical place, becomes a surplus material that is always already out of place. Similarly, fat is ‘out of place’ in the dissection practice guidelines because it resists the efforts to keep bodies ‘contained’: the efforts to uphold both the integrity of donors through the use of the yellow bucket, and the integrity of the students through the separation of living and dead bodies by means of gloves and lab coats. Fat respects neither of these orders; its unctuous materiality resists both containment and separation, ambivalently transferring traces of other human beings to places where they should not be, such as on my notebook.
As such, fat marks human bodies as unruly, not merely in their anatomical variations (marking each individual body as not entirely contained by the anatomical atlas-body) (Alraddadi 2021), but in a sense of being in excess of normative and scientific order. And we might also say that fat holds pollutive powers in the sense that its presence in the dissection body makes the body more-than-anatomical. This, in turn, invokes normative dilemmas for students—reminding them that they are ‘digging into’ a human body—and, through touch, fat passes on to the students the liminal subjectivity of the cadaver.
However, there are also ways in which Douglas’s notion is an awkward fit for fat. While fat can be framed as out-of-place in anatomy, the issue is not so much that fat is not supposed to be where it is (i.e., that it should be elsewhere), but rather that fat is not supposed to be there at all; it is not misplaced, but outside of place. Yet, despite this, part of the teaching objectives in this type of dissection class is exactly for students to encounter ‘real bodies’ (as opposed to anatomical model bodies) and to understand what it means to cut into these real bodies: in this regard, the fat is exactly what asserts the donor body as being a real body. It is what pulls the students into material relations with this real body—it makes them lean in, put their fingers into the bodies—not, as they would do with prosections, where the body is already neat anatomy, but in an unsettled search for anatomy. In this context, fat is somehow exactly ‘in place’, yet it remains an obstacle and a source of discomfort: fat hides important anatomy—deviously, creating a risk error—and resists when students attempt to put it into the bucket. Its ‘powers’, so to speak, do not come from its pollutive placement, but from its material treachery: quivering, enveloping, revealing bodies as a materiality that neither yields effortlessly to our interventions nor lets itself be demarcated and contained. And even the ‘pollutive power’ to proliferate is not—as for Douglas—symbolic, transferred through chains of contact, but rather occurs very concretely and materially as greasy traces that spread through touch and spray. That is, while Douglas is helpful for understanding the importance of space and materiality in making sense of the role of fat tissue in dissection, her notion also unhelpfully obscures significant material aspects of fat tissue in dissection.
In order to think about this, I have found it generative to draw on Sartre’s analysis of ‘slime’ as an in-between material.[6] In his cultural history of fat, Forth has already emphasised something similar: fat is a trickster material—we encounter it as both solid and fluid, and never really one or the other:
It isn’t a very convincing solid when congealed. Neither easily grasped nor managed, fat jiggles and slides about, seemingly ready to collapse into a liquid state at any moment. But even melting does not restore fat to its ‘true’ state, for oil doesn’t quite fit into the category of most liquids either (Forth 2019, 22).
Fat is unctuous and soft, it is greasy, sticky, and blubbery. Once removed it is not fully gone, it leaves a trace on surfaces that it comes into contact with, then further proliferates as the grease transfers—onto hands, onto handles, chairs, and notes. As students in the dissection hall navigate both the normative and the scientific goals of their practice—keeping the body whole through tracking and bucketing any removed tissue and clearing out anatomical structures so as to map out the body in ways that mimic the medical atlas—fat tissue resists their efforts. As an unruly companion, fat unsettles instructions and jumps, jiggling, off the bodies, sticks to surfaces, seeps into clothes and onto skin.
In the same way as Forth describes fat, Sartre ([1943] 1993) places slime as neither solid nor liquid. Slime does not mark us out as delimited subjects the way solid objects or liquids do. It is a seemingly both active and passive material, neither solid nor liquid, viscously spreading, oozing yet resisting with a heavy, slow, but persistent presence. As a solid, slime is not an object which we can possess or control (Sartre [1943] 1993, 776), manifesting our subjectivity through autonomy, which is equivalent to freedom for Sartre. As liquid, neither does it disappear effortlessly to our touch, marking us (the subjects) as durable (idem, 774). In the dissection hall, fat tissue similarly is neither an anatomical structure and nor is it like the preservation fluid—or even leftover faeces—which may be surplus material but can be flushed away in the drain. Rather fat, or grease, in the dissection hall, like the Sartrean slime, is there as a persistent, proliferating resistance, impossible to wipe off properly.
Grounded in its strange pseudo-agency, slime for Sartre is not just in between solid and fluid, but—being neither—also challenges categories of subject and object. In fact, slime almost reverses this relation, sucks us in (idem, 776), so that our sense of being subjects is compromised by materiality, and we must work tirelessly to separate matters from us and from each other to maintain order. ‘Slime is the revenge of the in-it-self [i.e., materiality]’, Sartre writes (idem, 777); but it is preconditioned by the fact that we are always already material. Encountering ‘slime’—or fat—is an ambiguous embodied realisation that we are bodies and not merely free subjects, a material manifestation of our own inescapable materiality: in other words, fat only sticks to material surfaces. Fat—as opposed to solid objects, definable anatomical structures that we can grab, cut, and place—touches us back, places itself on us: the greasy handle of the coffee pot or the air extraction pipe makes me acutely aware of the surface of my skin in contact with it. The young female student, initially unable to target a defined object (an anatomical structure), is engulfed by the fat tissue; inside another person—not because the fat is out of place, but because it is ‘slimy’, obscure, amorphous. Yet, while she leans away and attempts to lessen the contact between herself and the fat as much as possible, it is also this contact that carves out the two bodies—the student and the donor body—as embodied subjects: as one person poking her finger into another person’s flesh. As Forth writes, referencing William Miller’s The Anatomy of Disgust (1998): ‘disgust at fat materializes ambivalence about the fact that humans are embodied as well as misgivings about the wider material worlds to which those bodies belong’ (Forth 2019, 12). The greasy traces on sleeves or small pieces of fat in the hair of the students are not easily subdued, and through the fat—marking the bodies as real people’s concrete bodies rather than anatomical bodies—the dissection bodies assert themselves as not entirely subjugated to either the scientific system or the will of the students. Fat establishes the struggle for anatomical order in the form of annoyance and demands a deliberate and strong effort to ‘undo’ the existence of fat. Ironically, this effort requires physical labour and material engagement with the fat itself, looping back, so to speak, to its ‘sticky’ disrespect for bodily integrity. Anatomy and subjectivity are thus simultaneously contrasted yet tied into each other by the greasy resistance. In other words, material fat, and the necessity of engaging physically with it, mark the donor body as more-than-anatomical, as more than a tool for learning. But as the fat transfers onto gloves, pipes, and into students’ hair, it also discloses the lack of integrity in embodied personhood as such, through our (mine, the students, and the dissection bodies) inescapable material entanglements.
It is perhaps worth noting here that Sartre’s notion of slime has been the target of feminist critique, because Sartre aligns the slimy and the feminine (for an example see Sartre [1943] 1993, 776; for critiques see Collins and Pierce 1973; Barnes 1990; Murphy 2007). And while ideas of gender and embodiment are not the topic of this article, and I think we can draw on Sartre’s notion without necessarily invoking its gendered connotations, it curiously echoes similar tendencies in our conceptualisation of fat. In an article on Gunther von Hagen’s (in)famous exhibition Body Worlds, Tony Walter paraphrases von Hagen’s defence of using almost exclusively male bodies: ‘with on average 40 per cent less muscle [largely compensated by more fat], female whole-body plastinates display musculature [anatomy] poorly’ (Walter 2004, 483). One might wonder what role fat would have had in an anatomy which took its point of departure in the female body; or what status the female body would have had in an anatomy that included fat compartments in its mapping; or what status it will have in an anatomy which now, at least on a biomolecular level, recognises fat tissue as an active organ rather than a passive vessel for energy storage. But this is, however, a musing for another article.
What lessons do we learn from sticking with the fat?
In her work on fat replicas and their potential as evocative objects for cultural studies of fat, Kristen Hardy points to the affective learning that these objects aim at—of fat and fatness as something threatening (Hardy 2013, 11, 16). Similarly, fat in the dissection hall teaches, but not in the strong normative, univocal sense of Hardy’s fake fat. In the dissection hall, fat is more ambiguous than a mere threat. Its proliferation throughout the dissection hall, its mysterious covering over of anatomical structures, and its demand for careful attention and hard labour, all tie students and cadavers into each other as bodies: embodied, material humans. Fat teaches us to think of the body as more-than-anatomy and of the subject as inescapably material. Fat, as insignificant anatomical tissue in most partial, anatomical bodies (e.g., specimens and models), thus becomes significant excess in dissection. This is not so much with respect to the amount of it, but for its ‘being everywhere’, in the body and in the dissection hall, and for the material challenge that its removal poses: the difficult balance in care and physical engagement, the slipperiness of instruments, its clinginess that makes the task of keeping the workstation in order a tiresome one, making it practically dominant despite its anatomical neglect. Several times during my fieldwork, I asked students what the hardest part was about dissection. I expected them to talk about death or the macabre or even the difficulty of the curriculum, but their immediate response was to complain that they were tired of removing fat, that it was everywhere, that it smelled and made the whole process difficult. Fat is disposable yet resistant to this very disposal. And I have aimed to show that it is so in a very material sense.
So, where do we go if we stick with the fat? Into the bucket? Onto air extraction pipes and students? Away from anatomy—or into a different, feminine anatomy? Or perhaps towards a re-conceptualisation of embodied subjectivity? Perhaps we can go to all of them; perhaps none. The ambition of sticking with the fat in this article is similar to Astrida Neimanis’s (2016) invitation to think through water: it is an invitation to allow a mix of concrete material capacities, metaphorical associations, and theoretical considerations to guide our way through unexplored ways of thinking about human bodies and their composition. This journey should take us to the buckets, the air extraction pipes, the students, the dissection bodies, the specimens, and a vast greasy network of elements beyond anatomical order.
Acknowledgements
According to the Danish ethics committee law §2, no. 1, only health scientific research that includes biological material and clinical trials needs ethical approval. Therefore, no official approval was sought out, nor granted for the fieldwork. However, a data-compliance approval was granted by the university data committee, approving the projects compliance with GDPR regulations. All students and staff present at the dissection hall were informed of my presence and purpose, and I always asked permission to join students when I shadowed individual students or smaller groups. I would like to thank Jørgen Tranum-Jensen for allowing me into the dissection hall and for spending many hours answering questions and giving feedback; the medical students in the two courses I followed, who were all impressively kind and curious; Simone Cecilie Grytter for several rounds of thorough comments; the Medical Museion Research Lab, where I presented an early version of this article; as well as two anonymous reviewers and the MAT editor who all made helpful suggestions that greatly improved the article.
About the author
Helene Scott-Fordsmand is an empirical philosopher working with ethnographic methods in philosophy of science and philosophy of medical practice. She completed her PhD at Medical Museion and the Centre for Medical Science and Technology Studies in the Department for Public Health, University of Copenhagen. She graduated in October 2021 with the dissertation ‘Encountering the unruly: Reflections on epistemic aspects of the abject and the out-of-place in medical practice’. She is currently conducting research on a Carlsberg Foundation Postdoctoral Fellowship, ‘Diagnosing bodies in a messy reality’, at the Department for History and Philosophy of Science, University of Cambridge.
Footnotes
-
Both are different from the dissection hall, where students only come when they have their allotted course time. The wet study hall is a tile-covered room in the vicinity of the dissection hall, where a variety of (fatless) prosections are kept in large opaque jars, available for students to pick up, touch, and investigate, but are not accompanied by any guidance other than a descriptive label on the jar pertaining to their general anatomical region (e.g., ‘Regio glutealis et regio coxae’). The dry study hall is a closed-off section of the medical library, where a large collection of sealed specimens, with coloured markings on all relevant anatomical structures, are lined up in glass vitrines and matched with sheets providing keys for all the markings.↩︎
-
Apart from the bodies used for medical students, bodies are also used for surgical courses and research. Bodies used for these purposes are usually preserved merely by freezing, as these activities rarely span more than two to three days, and the risk of infection is seen to be offset by the more experienced practitioners and the benefits of keeping the bodies as ‘life-like’ as possible (see Olejaz 2020 for more detail on the specifics of donation in Denmark).↩︎
-
Elizabeth Hallam describes a similar reflection from a student about learning from mistakes in dissection (Hallam 2016, 74).↩︎
-
The body’s return can take place up to two years from the time of death but must not exceed this period. This limited time span is due to the fact that proper preparation of the bodies prior to dissection takes several months: the liquids need time to permeate the cells in a non-destructive way; first the formaldehyde to fixate structures, then alcohol to wash out any free (carcinogenic) formaldehyde. The additional need to align the reception of bodies—which is, for obvious reasons, non-plannable—with the timing of the course presents further challenges to this timeline.↩︎
-
Nuancing this idea of fat as undesirable because it is out of place, Forth also points to neoliberal ideals of ‘trimming the fat’ (Forth 2019, 276): fat as an unnecessary, unproductive surplus. Hardy indicates something similar in her analysis of the fat replica and the body fat vest, which establishes fat as an extra, ‘which can and ought to be removed from the “real” not-fat body’ (Hardy 2013, 16).↩︎
-
Another common analytical reference, used, for example, by both Warin (2003) and Hardy (2013), is Julia Kristeva’s notion of ‘abjection’ (Kristeva 1982). While there are similarities between Kristeva’s abject and Sartre’s slime, and Kristeva’s notion is superior in terms of being more elaborately articulated by her and further developed by other scholars, I have chosen to draw on Sartre, because his notion of slime posits an in-between entity that draws its in-betweenness from its materiality, rather than—as I read Kristeva—an in-between entity that draws its in-betweenness from having transgressed from one category to another without fully letting go of the first. I have developed Kristeva’s notion in the context of medicine elsewhere (Scott-Fordsmand 2021).↩︎
References
Alraddadi, Abdulrahman. 2021. ‘Literature Review of Anatomical Variations: Clinical Significance, Identification Approach, and Teaching Strategies’. Cureus, 13 April, 2021. https://doi.org/10.7759/cureus.14451.
Barnes, Hazel E. 1990. ‘Sartre and Sexism’. Philosophy and Literature 14 (2): 340–47. https://doi.org/10.1353/phl.1990.0012.
Braziel, Jana Evans, and Kathleen LeBesco. 2001. Bodies Out of Bounds: Fatness and Transgression. Berkeley, CA: University of California Press.
Coelho, Marisa, Teresa Oliveira, and Ruben Fernandes. 2013. ‘Biochemistry of Adipose Tissue: An Endocrine Organ’. Archives of Medical Science 9 (2): 191–200. https://doi.org/10.5114/aoms.2013.33181.
Collins, Margery, and Christine Pierce. 1973. ‘Holes and Slime: Sexism in Sartre’s Psychoanalysis’. Philosophical Forum 5 (1): 112.
Cooper, Charlotte. 2010. ‘Fat Studies: Mapping the Field: Fat Studies’. Sociology Compass 4 (12): 1020–34. https://doi.org/10.1111/j.1751-9020.2010.00336.x.
Douglas, Mary. (1943) 2003. Purity and Danger: An Analysis of Concepts of Pollution and Taboo. Collected Works, Mary Douglas, Vol. 2. London: Routledge.
Forth, Christopher E. 2019. Fat: A Cultural History of the Stuff of Life. London: Reaktion Books.
Forth, Christopher E., Alison Leitch, and Samantha Murray, eds. 2014. Fat: Culture and Materiality. London and New York, NY: Bloomsbury Academic.
Fountain, T. Kenny. 2014. Rhetoric in the Flesh: Trained Vision, Technical Expertise, and the Gross Anatomy Lab. New York, NY: Routledge.
Gilman, Sander L. 2008. Fat: A Cultural History of Obesity. Cambridge, UK and Malden, MA: Polity Press.
Goss, Adeline L., Leah Rethy, Rebecca L. Pearl, and Horace M. DeLisser. 2020. ‘The “Difficult” Cadaver: Weight Bias in the Gross Anatomy Lab’. Medical Education Online 25 (1): 1742966. https://doi.org/10.1080/10872981.2020.1742966.
Hallam, Elizabeth. 2016. Anatomy Museum: Death and the Body Displayed. London: Reaktion Books.
Hallam, Elizabeth. 2020. ‘Relational Anatomy: Dissecting and Memorialising the Dead in Medical Education’. Medicine Anthropology Theory 4 (4): 99–124. https://doi.org/10.17157/mat.4.4.314.
Hardy, Kristen A. 2013. ‘The Education of Affect: Anatomical Replicas and “Feeling Fat”’. Body & Society 19 (1): 3–26. https://doi.org/10.1177/1357034X12441629.
Kristeva, Julia. 1982. Powers of Horror: An Essay on Abjection. New York, NY: Columbia University Press.
Latour, Bruno. 1993. We Have Never Been Modern. Cambridge, MA: Harvard University Press.
Merleau-Ponty, Maurice. 2005. Phenomenology of Perception. Translated by Colin Smith. London: Routledge.
Miller, Daniel. 2005. ‘Materiality: An Introduction’. In Materiality, edited by Daniel Miller, 1–50. Durham, NC: Duke University Press. https://doi.org/10.2307/j.ctv11hpnrp.
Miller, William Ian. 1998. The Anatomy of Disgust. Cambridge, MA: Harvard University Press.
Mol, Annemarie. 2002. The Body Multiple: Ontology in Medical Practice. Durham, NC: Duke University Press.
Murphy, Julien S., ed. 2007. Feminist Interpretations of Jean-Paul Sartre. University Park, PA: Pennsylvania State University Press.
Neimanis, Astrida. 2016. Bodies of Water: Posthuman Feminist Phenomenology. London: Bloomsbury Publishing.
Olejaz, Maria. 2020. ‘When the Dead Teach: Exploring the Postvital Life of Cadavers in Danish Dissection Labs’. Medicine Anthropology Theory 4 (4): 125–49. https://doi.org/10.17157/mat.4.4.310.
Pond, Caroline M. 2017. ‘Accuracy and Artistry in Anatomical Illustration of Perivascular Adipose Tissue’. Frontiers in Physiology 8 (December): 990. https://doi.org/10.3389/fphys.2017.00990.
Prentice, Rachel. 2013. Bodies in Formation: An Ethnography of Anatomy and Surgery Education. Durham, NC: Duke University Press.
Rheinberger, Hans-Jörg. 2010. An Epistemology of the Concrete: Twentieth-Century Histories of Life. Durham, NC: Duke University Press.
Sartre, Jean-Paul. (1943) 1993. Being and Nothingness: An Essay on Phenomenological Ontology. New York, NY: Washington Square Press.
Scanlon, Valerie C., and Tina Sanders. 2015. Essentials of Anatomy and Physiology. 7th edition. Philadelphia, PA: F. A. Davis Company.
Scott-Fordsmand, Helene. 2021. ‘Abject Object Relations and Epistemic Engagement in Clinical Practice’. Philosophy of Medicine 2 (2). https://doi.org/10.5195/pom.2021.45.
Shier, David, Jackie Butler, Ricki Lewis, and John W. Hole. 2012. Hole’s Essentials of Human Anatomy & Physiology. 11th edition. Boston, MA: McGraw-Hill Education.
Vesalius, Andreas. 1543. De Humani Corporis Fabrica Libri Septem. Basel: Johannes Oporinus.
Walter, Tony. 2004. ‘Body Worlds: Clinical Detachment and Anatomical Awe’. Sociology of Health & Illness 26 (4): 464–88. https://doi.org/10.1111/j.0141-9889.2004.00401.x.
Warin, Megan. 2003. ‘Miasmatic Calories and Saturating Fats: Fear of Contamination in Anorexia’. Culture, Medicine and Psychiatry 27 (1): 77–93. https://doi.org/10.1023/A:1023683905157.