Making Sense of New Disease Categories
Naming, Spatialising, and Serialising in Genomic Medicine
—
Abstract
Introduction
As we sit in the genetic counselling outpatient room in March 2018, I hear geneticist Esther say: ‘Listen, Simon, we’ve found an explanation for why you’re different. You know, why you find school work difficult and all that …?’ Esther finds a piece of paper and writes down ‘DPF2’ and goes on, ‘Yes, I know it’s a strange name, and it doesn’t mean anything, and you don’t have to remember the name. This doesn’t change who you are as a person’. On another occasion, sometime in May 2019, genetic counsellor Astrid in the diabetes clinic explains to 65-year-old patient Henrik:
G246A is the name of the genetic variation you have. It is not important that you remember the name. What is important is that if we are right about this it means … that you will not develop diabetic complications and you will respond poorly to medical treatment. Therefore, we believe you should NOT take medication. Then you are healthy [ rask ] … I can see that you are the only one of your kind in Denmark and in the world.
To this, I hear Henrik respond: ‘How now, damn that is fantastic! OK, that is exciting! Damn I am an interesting person!’
This Research Article explores how patients like Simon and Henrik 1 and their families make sense of naming practices in the field of genomic medicine, which—in the aim for ever-more precise disease categorisation—result in names almost akin to car-license plates for disorders such as DPF2 (which stands for ‘Double PHD Fingers 2’) and G246A (which stands for mutation ‘p.G246A (Substitution - Missense, position 246, G➞A)’. Even though the human genome was mapped out decades ago, clinicians and scientists continue to find and add new disorders caused by genetic variants to the catalogue of single-gene conditions. In the past decade alone, 2500 new conditions were added to this catalogue (Rasmussen 2020). However, whether the newly identified genetic variants—along with the pursuit of certainty and precision in biomedicine more generally —elicit more precision or create more confusion and uncertainty is an ongoing discussion within both medicine and social science (Green et al. 2019; Navon 2019; Pickersgill 2013; Reardon 2017; Timmermans 2017; Tutton 2014).
The speed with which genetic knowledge is produced and the continuously changing disease taxonomies have given birth to a new nomenclature in genetics based on the location of a genetic mutation. While genetic syndromes were once named after the scientist who first ‘found’ the mutation responsible for the disorders, such as Huntington’s syndrome and Marfan’s syndrome, today’s phenotypes are often named after the gene in which a mutation that causes the condition occurs, as is the case with Simon and Henrik mentioned above. Within the field of genomic medicine, proponents of this new naming practice argue that it provides a welcomed flexibility, given that phenotype descriptions are moving targets, constantly changing as more patients are described. Opponents, on the other hand, fear that this new naming practice will lead to confusion among patients. Rasmussen (2020, 1573–74) argues, for example, that ‘ideally, names should be medically informative; meaningful; accessible across disciplines […] gene names are often cumbersome and less meaningful, making them difficult to remember’.
When I began fieldwork in genomic medicine, I was familiar with the classic literature on the social dynamics of categorisation, which has focused on how classifications came into being historically, how they change people, and how people change classifications in return (Foucault 1988; Hacking 1986, 1995; Goffman 1986; Bowker and Star 1999). Consequently, I was intrigued by the geneticists and researchers’ framing of gene names as somehow devoid of meaning. This made me curious to understand how the patients and their families use and make meaning of these new gene names.
Between 2017 and 2021, I documented the introduction of personalised medicine in Denmark as part of a larger study on the ethics of genomic or personalised medicine. Personalised medicine, also often referred to as precision medicine, has a clinical, research, and political agenda that aims at tailoring prevention, diagnosis, and treatment to the individual based on genomic and other data (see, e.g., Chan and Ginsburg 2011; Perlman and Govindaraju 2016; Erikainen and Chan 2019). Specifically, I followed the use of exome and whole genome sequencing in two medical fields occupied with identifying genetic diagnosis, conducting fieldwork in clinical genetics and diabetes research and treatment in Denmark. In total, I observed more than 20 genetic counselling sessions and interviewed 10 clinicians, and 22 patients and families. On the one hand, in regards to clinical genetics, I sat in hour-long genetic counselling sessions attended by children with rare genetic diseases and their parents in a Danish clinic, which sometimes resulted in a genetic diagnosis like DPF2 . The majority of the children I met in the clinic were adolescents at the time, but had demonstrated developmental delay and cognitive disabilities from an early age. In the sessions, their parents presented stories of problematic pregnancies, difficult births, breast-feeding challenges, delayed walking and talking, as well as experiences of intellectual and social problems in school. Many of the parents had a long history of feeling misrecognised. They often described being categorised as unfit parents by their health visitor or the local authorities; that is, that the child’s issues could be due to mental problems, a lower IQ, or ‘bad parenting’. Meanwhile, not all of the families present in the sessions received a genetic diagnosis for their child, and for those who did, a treatment rarely existed for the child’s condition.
On the other hand, in the context of diabetes research, I followed two related research projects, called StratDiab and TRANSLATE. These scientific studies aimed to identify 1–2% of the world’s entire diabetes population (starting with Denmark) carrying rare variants in genes that have implications for treatment choice, risk of comorbidities, and diabetes detection within the patient’s family. The projects looked for patients with genetic variants that are associated with monogenic diabetes, termed ‘Maturity-Onset Diabetes of the Young’ (MODY). One such mutation (known as ‘MODY 2’) is the rare genetic variation in the GCK gene, which encodes for the Glucokinase enzyme which causes a subtype of diabetes that does not require patients to take medical treatment (Shepherd et al. 2018; Stride et al. 2014) and rarely develops diabetes complications. In fact, these patients are not deemed sick. According to the TRANSLATE project website, their stated aim is to ‘prevent overtreatment’ and to redirect this subgroup of patients carrying ‘a benign form of diabetes’ from ‘standard treatment to no treatment’. 2 Thus, in the field of diabetes, genetic test results may have treatment consequences.
Following the diabetes researchers carrying out their work, I observed four hour-long sessions where a medical doctor and a medical student tested and monitored type 2 diabetes patients, like Henrik above, for genetic variations. Here, I learned that some diabetes patients had been (mis)labelled with a disease for between 10 and 20 and sometimes up to 40 years before being suddenly relabelled with a GCK mutation such as the G246A.
By engaging with theories of naming (Hacking 1986, 1995), I show that while the geneticists, researchers, and patients seemed to treat the new variant names haphazardly, were often unable to remember them, and articulated them as ‘meaningless’, their diagnoses carried significant and multiple meanings. First, I argue that it is exactly because of their unsettled meaning, or ‘epistemic murk’ (Taussig 1987), and their lack of disease history or ‘data inheritance’ (Green and Svendsen 2021) that strange names for genetic diseases such as DPF2 and G246A may provide patients some flexibility and extra room for creative identity work. In eclectic ways, these patients and their families ‘mobilise’ mutations (Navon 2019) and disease labels interchangeably (Stivers and Timmermans 2017; Featherstone et al. 2006; McLaughlin and Clavering 2012), or immobilise the labels by deactivating or ‘downplaying’ (Latimer 2013) them to achieve membership of a specific community and refuse membership of another.
Second, I show that some patients and families use the unsettled character of the new disease labels to escape particular unwanted moral regimes. For example, the new gene names allow children diagnosed with developmental delays and their parents to shed labels such as ‘lazy child’ and ‘bad parent’. Moreover, for people diagnosed with the GCK mutation, they too can rebuff labels such as ‘unhealthy’ and ‘undisciplined’ that haunt some (but not all) people diagnosed with type 2 diabetes. Drawing on Nikolas Rose’s work on ‘spatialising’ (2007), I argue that names like DPF2 relocate disease aetiology from a highly moralised landscape to a ‘molecularised’ (Rose 2007) genetic landscape that—for now—lacks strong moral associations. With time, we can expect these genetic diseases to gain new names and acquire new social and cultural meanings, as the patient population grows and the patients’ phenotypes are better described in the scientific literature.
Third, in what follows I engage theories of serialisation and bureaucratisation (i.e., Stevenson 2014; Petryna 2003) when discussing issues of anonymous versus personalised forms of care. I examine what is at stake when patients like Henrik come to feel ‘interesting’ and recognised as ‘unique persons’ when presented with semantically haphazard disease labels. I argue that the serialisation offered by genomic medicine is experienced as empowering rather than disempowering and as individualising rather than anonymising. I end by challenging the assertion, as voiced by geneticist Esther, that the new genetic labels ‘don’t change who you are as a person’. On the contrary, the empirical findings of this study suggest that while the new genetic names may not at present stigmatise, they do change the patients’ idea of who they are in surprising and subtle ways, some of which the geneticists had not anticipated.
The Danish context
The Danish welfare state offers tax-financed healthcare to all citizens from conception to grave and steers its citizens through various forms of institutionalised care (Navne and Svendsen 2017). Obligatory in-home visits from a health visitor following the birth of a child constitute one such type of care. These home visits are performed not only to monitor the development of the infant (e.g., to check on growth, hearing, and breast-feeding), but also to assess the parents’ ability to care for and form attachment to the child. If the health visitor suspects that something is wrong with the infant’s development or with the parents’ ability to care for the child, they may refer or report the family to additional health services or to child welfare authorities. Employed at state schools, health visitors may also observe issues of parental neglect or developmental delays in a child’s life at a later stage. Other forms of institutionalised care extend to citizens who are diagnosed with a so-called lifestyle disease, such as type 2 diabetes, that is often considered to be caused by overeating, improper diet, or lack of exercise. With regard to preventing diseases such as diabetes and lung and heart diseases, Danish public health policies focus on creating a healthy population through public campaigns that target the individual as being responsible for living a healthy life and making healthy lifestyle choices (Vallgårda 2011). When a patient is diagnosed with type 2 diabetes, they are automatically referred to patient education, for example, in the form of cooking classes especially designed for people with diabetes.
The public healthcare system in Denmark rests on a complex distribution system in which the state allocates a budget for the local municipalities to manage service provision. The families of children with disabilities are, in principle, entitled to services such as special education, and people with chronic diseases are entitled to patient education. However, the principles and practices for distribution are interpreted and managed differently by each municipality. Legally, therefore, social workers should be able to assign help to a citizen even though they do not have a diagnosis. Nevertheless, service distribution practices vary greatly depending on the municipality of residence.
Danish healthcare planning has increasingly turned its rhetoric to one of patient-centred care and patient empowerment (Danish Regions 2015). In social science, discourses on patient involvement and healthy citizenship have widely been conceptualised as modes of social control and governmentality (see Foucault 1977, 2008). More recently, Richard Tutton (2014) and Barbara Prainsack (2017) have established a historical continuity between the family doctor who conducts home visits and attends to personal narratives at the bedside, and the current rhetoric of personalised medicine, whose proponents advocate tailoring treatment to the individual. Yet, while the ideal of patient-centred healthcare may be echoed in the visions of personalised medicine, what is considered personal may, as we shall see, be located, as in this case, at a molecular level.
Naming, disciplining, and serialisation
Theoretically, I interrogate naming practices in genomic medicine. My interpretations are situated within theories on disease labelling, identity, and biopolitics. Numerous social science studies have examined the power of naming a medical disease and how a name affects patient identities (e.g., Foucault 1988; Rose 2007; Hacking 1995). Following Foucault’s seminal work on biopolitics, philosopher Ian Hacking (1986) pursued the question of what labelling and naming does to people and their identities in the context of deviation and control. In his article ‘Making up People’, Hacking argues that knowledge production creates new categories and ‘kinds’ of people and that the people come to fit their categories (1986, 160–3). In other words, disease labels are loaded with social and cultural meaning that carries a transformative potential that affects personal identity. Later in his career, Hacking added to this argument that the actions and responses of people being categorised come to change the categories themselves and in turn offer ever new knowledge about their phenotype or ‘kind’ (Hacking 1994, 370). This process is what Hacking termed ‘the looping effect’ (1995) or ‘dynamic nominalism’ (1986, 170).
Building on Hacking’s insights, I explore the social contexts in which labelling of children with rare genetic diseases and the relabelling of long-term diabetes patients occur, and how these two patient groups ascribe meaning to the new genomic labels and use the space of possibility provided by these labels. While Hacking emphasises the importance of the historicity of a disease and the language available for describing and explaining disease (Hacking 1994, 368), I present a case in which the disease category has neither history nor recognisable conceptualisation. I demonstrate that the combination of its novelty and its intangible and fleeting semantic expression of the new genetic codes offers extraordinary potential for identity transformation—an unsettled moralised landscape to manoeuvre for the patient and family. I describe the creative ways in which patients and families use (and do not use) the new genetic disease names—sometimes unmaking the identities assigned to them as service ‘clients’ or undisciplined citizens.
Renaming practices are sometimes politically motivated. The renaming of streets and public institutions from male to female names is just one example of how gender politics is shaping naming practices, for instance. The Icelandic anthropologist Gisli Palsson (2014) has explored personal names and, in particular, the politics of naming. Palsson looks at names as technologies of the self and as ‘both means to domination and empowerment, facilitating collective surveillance and subjugation and the individual fashioning of identity and subjectivity’ (2014, 620). He demonstrates that names gain power and can exclude and subjugate; primarily through history and memories.
Bringing together the work of Hacking and Palsson helped me pose the following question in the context of my field: what does it mean to be labelled DPF2, a brand-new label carried only by—at the time of my fieldwork—eight other individuals in the world? I was curious as to how patients and their families experienced receiving a disease label largely devoid of history, memory, and predefined meaning as a consequence of the recent naming system emerging in the field of genomic medicine.
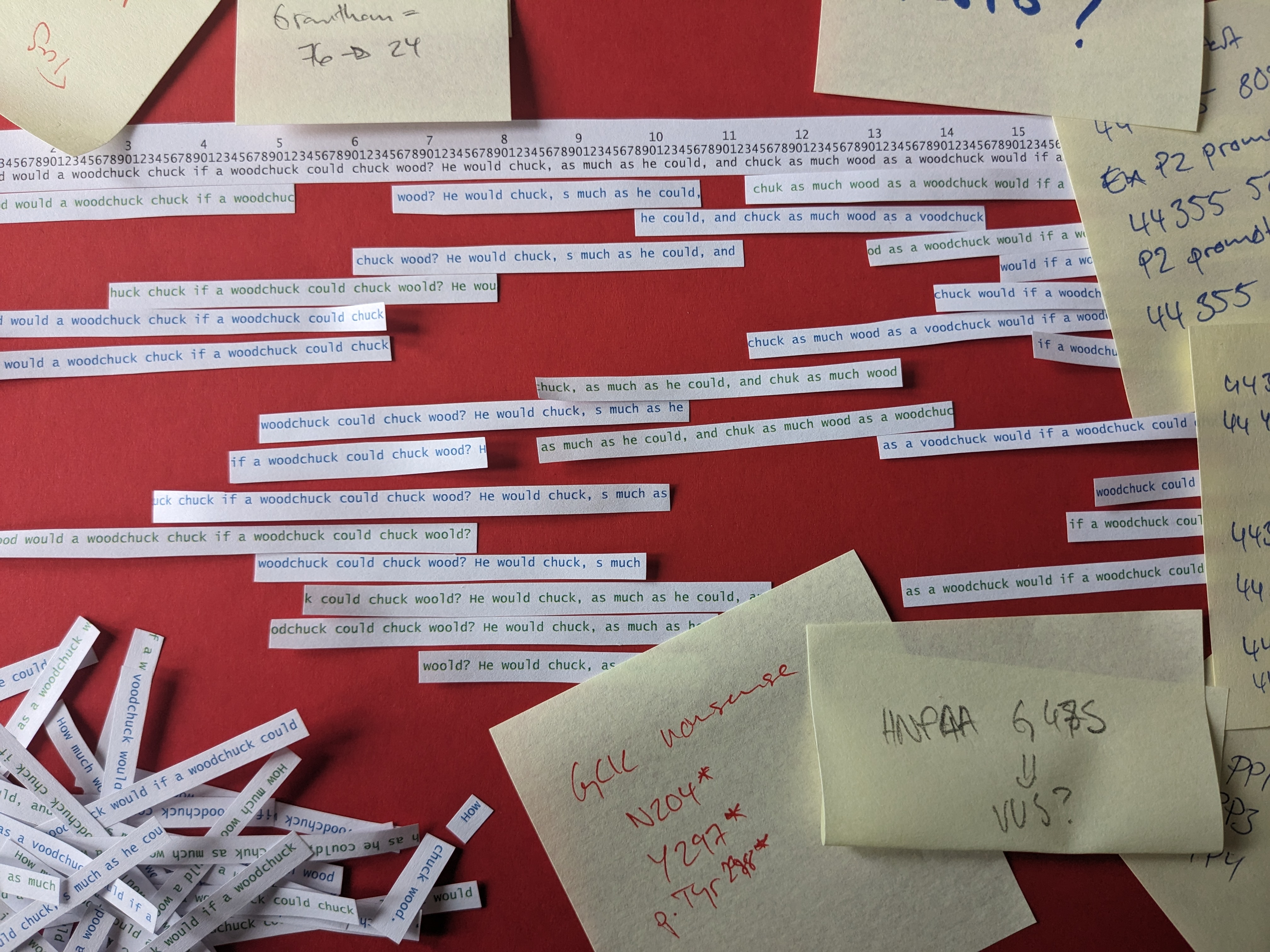
According to Abel, Tyson, and Palsson (2019), renaming efforts can be both emancipating and subjugating, in that a new name holds both the potential to set the renamed free of their history and to weigh them down with new stigmas. In what might seem a contradiction in terms, patients and families experienced the new gene names as not only unsettled in meaning and easy to forget, but also as a means of empowerment. For them, these names represented a personal and individualised type of care as opposed to standardised and anonymous care. In her book Life Beside Itself (2014) on postcolonial forms of care in the Canadian Arctic, Lisa Stevenson demonstrates that statistics and population health interventions are governmental technologies of serialisation and symptoms of anonymous, and indifferent forms of care (2014, 29). She exemplifies such indifferent forms of care with the Canadian health authority’s introduction of identification tags for Inuit as a means to keep track of transmission routes during an epidemic outbreak of tuberculosis in the 1940s (idem, 26). Evidently, making humans and disease names into numbers have very different implications, but in both contexts the counting and registration practices serve bureaucratic and public health purposes (Danish Regions, 2015) and become implicated in questions of identity. In the case of the Canadian Arctic, numbering practices become illustrative of ‘the biopolitical insistence that care should be administered indifferently without it mattering for whom ’ as Stevenson notes (2014, 5, original emphasis). In contrast, numbering in the case of genetic disease offers not only flexibility and creativity in identity work but also a unique biological identifier that singles out the individual. Where serialisation was central to ‘making up’ (Hacking 1986) bodies and lives in public healthcare in the Canadian Arctic, so, too, is serialisation at the centre of the making up of bodies and lives in present day precision medicine in public healthcare in Denmark. This is evident in the dual purpose of this new naming practice, i.e., the purpose of naming diseases according to causative genes to ensure precision and flexibility in future diagnostic work and the purpose of anticipating the speed of changes within genomic medicine (Rasmussen 2020, 1573). Such serialisation, which involves naming disease according to the position of genes, inevitably shapes patients’ understandings of their bodies and lives. However, serialisation in genomic medicine is not experienced as anonymous care. On the contrary, for the patients and families in clinical genetics and diabetes research in my fieldwork, the serialisation produced by genomic medicine was experienced as individualising or singularising in that it made them feel like ‘not just a number in a row’, as one of the interlocutors expressed it.
A space for creative identity work
When the two genetic counsellors in the opening citations trivialise the ‘need to remember’ the gene names DPF2 and G246A, they suggest that the gene names easily escape human memory. Also, downplaying the significance of the names by saying ‘it doesn’t mean anything’, the genetic counsellors suggest that the actual letters and numbers carry no significant meaning and that having the diagnosis does not change who, for example, the 16-year-old boy Simon or the 65-year-old man, Henrik, is. The articulation of genetic disease labels as somehow ‘meaningless’ was a general one among the clinicians I interviewed; however, I soon learned that this did not mean that the labels did not transform patient identity, nor that the patients and families did not ascribe meaning to them. Rather, I learned that somehow these new gene labels offered the patients and families a space of possibility for shaping their identity in new and flexible ways and for renegotiating relationships with others in society.
Existing literature on disease categories argues that such disease categories may alter a person’s room for manoeuvre (e.g., Kohrman 2003; Antze and Lambek 2016; Manderson 2020). The patients and families I interviewed found these semantically ‘odd’ and ‘forgettable’ labels particularly productive due to their blank slate and opaque quality.
I carried out an interview in the hospital cafeteria with Kirsten, mother of the 18-year-old Ole, who had recently been diagnosed with EBF3 (EBF Transcription Factor 3). Here, she expressed her response to the name of the diagnosis of her son:
Laura: It is difficult to understand, when you get these letter-number combinations … and you cannot immediately relate to it.
Kirsten: No, no, no, you can’t [understand and relate to it]. If Esther [geneticist] hadn’t translated it for us, we would have been clueless.
Within the community of genetic counsellors and geneticists, a central critique of the new naming system is that the labels make little sense to patients. However, while the new labels might leave patients and families ‘clueless’, as Kirsten says, they offer families the long-awaited recognition that their children’s symptoms are related to somatic disease. In the following excerpt, Kirsten introduces me to how she and her family make sense of this label exactly because the new genetic label offers no clear description of a phenotype or a ‘kind’:
When my son was younger, I always said, argh, if only he had had Down’s syndrome, it would have been easier, because then I would’ve had a book to read and I could’ve gone to the social authorities and asked for the help I needed. … Today I can say: How lucky and grateful I am, because bottom line, I don’t care. It [the diagnosis] won’t change the way my son is. We have never seen ourselves as a disabled family, and we have never seen Ole as a disabled person.
Kirsten suggests that the degree to which you start seeing your child through a disease label/diagnosis has to do with how well established the meaning of the label is. The ‘older’ and ‘thicker’ the name of the diagnosis (e.g., Down’s syndrome), the more settled are the moral connotations it has, and the more it shapes the ‘looping effect’ (Hacking 1995) between the label and the person’s identity. For Kirsten, having an authoritative book to read about her child’s disease once seemed attractive, but when looking back at their lives, not having a well-described syndrome made it easier to displace the identity as a family with disabilities.
The ways in which the qualities and values of a name impact processes of domination or empowerment occupy Palsson’s work (2014, 620). Drawing on the historical case of slavery, Palsson describes the act of naming of the enslaved after historical figures such as Cicero, the famous Roman general, as a deliberate ploy to undermine subjective identity (idem, 625). In addition, by naming the enslaved after a European ancestor of the suppressors, this emphasised their marginalisation (Ibid). While Down’s syndrome has a substantial history—and has for decades represented a large community of people who carry the same condition—many of the genetic diagnoses established through the use of new genetic testing technologies (such as EBF3 or DPF2) are very rare and only found in a few individuals worldwide. Their names have no or very short histories. Temporarily at least, these new genetic names represent recent discoveries and open categories yet to be filled out by their name-bearer(s). Put differently, the narratives of these illnesses have not yet been written, and people like Ole and Simon may write these narratives themselves, perhaps to be used in turn by future patients to help them understand themselves.
Resisting the label ‘disabled family’ and refusing to be part of patient communities was a common approach for many of the families I interviewed. This was also the case for Simon’s mother Inge, who deliberately avoided joining a Facebook group for parents of children carrying the same genetic variation as Simon, because her family needed so badly to stop feeling like and being seen as a ‘disabled family’, as she phrased it. Following the legacy of Paul Rabinow and contemporary scholars working with the concept of biosociality (Rabinow 1992; Finkler 2000; Franklin and McKinnon 2001; Gibbon 2009; Novas 2007), scholars have convincingly demonstrated the power of genetic diagnostics to mobilise patient communities (see Navon 2019; Novas 2007; Petryna 2003; Rose 2007). Having become familiar with these analyses, I was surprised to learn that many of the families I met in clinical genetics were not interested in joining a patient community. Instead, they sought a name for the disease, while also appreciating the negligible history of the new names. This, I learned, allowed them to selectively activate and disable the disease names; they could choose not to participate in patient communities and at the same time use the new label to access the welfare state community. For example, Simon’s mother Inge used her son’s label to get help in the public education system:
Laura: Do you think this new diagnosis has made a difference in Simon’s life?
Inge: Yes! Certainly. I believe it has. Like, the other children at his boarding school, they either have ADHD or autism. It’s a school for children with special needs. Here, I believe it’s been good for Simon to have a name. For instance, next summer he has to pass an exam for graduation and this is extremely difficult. This winter Simon failed the test exam. Now, with the diagnosis, we can articulate that he needs help. Simon can say, ‘It’s because I have this syndrome’. He doesn’t have to just say, ‘I’m not very good at Danish or math’, and the teacher can’t just say ‘but you can learn’. Now the teacher can check his files and read about the reason for it. So, if we can find a way to use this in a constructive way, and not just think that now you have this label attached … then I think it makes sense for Simon.
For Inge, the diagnosis provides a flexibility that can be used strategically to Simon and his family’s advantage. First, the family can present the diagnosis to the local authority, to challenge their policy thus far of treating Simon like a ‘normal kid’ who, in their view, just needs to ‘work harder’. The new name translates Simon’s difficulties in school into a language the system understands and responds to with educational support. Second, while Simon was already granted admission to the boarding school for children with special needs before he was diagnosed, Inge anticipates that the diagnosis may help Simon feel included in the boarding-school’s social community in which a diagnosis is the norm. Thus, the name enables him to ‘fit in’ and belong to a social community with his peers.
Talking to the children themselves, they expressed that receiving a diagnosis mainly raised questions and concerns related to their everyday lives such as, ‘Does that mean I need orthopaedic shoes?’; ‘Is that why I always only want to play with that same swing in the school yard every day?’; and ‘Can I ride a moped with my friends?’. I interviewed Simon six months after he got his diagnosis. I asked him to tell me what he remembered about the conversation with Esther, the geneticist:
Simon: It was about … we were told what diagnosis I had. That was it. And that was okay … exciting to come and hear what it was and yes …
Laura: What did it mean to you to get this diagnosis?
Simon: Uh, [silence] … I don’t really know what it means, not much.
Laura: Did you tell any of your friends?
Simon (promptly, sounds happy): Yes!
Laura: What did they say?
Simon: They thought it was interesting.
Laura: What did you tell them?
Simon: What it’s called and how many people have it.
Laura: How did they react?
Simon: They think it’s cool that so few people have it.
[…]
Laura: Have you ever experienced people asking you about your feet and toes?
Simon: Not in kindergarten, but in school a few kids asked. But I didn’t know then. If someone asks me now, I can tell them, because now I know.
It is difficult to say exactly how Simon felt about all this. Yet, considering that Simon generally responded to my questions with a neutral ‘yes’ or ‘no’, the way his voice went up a few times showing enthusiasm indicated to me that these issues mattered to him. One such moment was when I asked him what he wanted to be when he grew up. He instantly replied, ‘I want to be a carpenter!’ Another such moment was the one cited above where he talks about being able to tell his friends about why his feet look different and how his friends thought ‘it was cool’ that so few people carry this genetic variation. His reaction suggests that even though Simon says that getting a diagnosis ‘did not mean much’ and that he does not remember what the disease is called, the diagnosis performs socially important work for him; it helps Simon explain to his friends why he is different.
In Simon’s case, we may say that Hacking’s theory of a looping effect between the label and the person, that interchangeably shapes the other, holds strong. For Simon and many of the children and parents I talked to, the fact that they do not really remember and understand the labels and their meaning may contribute to them being able to read their own meaning into the label and to shape their own identity in doing so. While Simon used the diagnosis as a way to navigate being different in his peer community, his mother, Inge, not only used the label to renegotiate help from the state authorities, but also to secure her son’s future:
Laura: Earlier, you talked about how difficult it could be to get help from the municipality when Simon was younger. Did they ask for a diagnosis back then?
Inge: They said, ‘We can’t help you because you don’t have a diagnosis.’ That’s why I became obsessed with chasing a diagnosis. Now, I’m so relieved that Simon got the diagnosis before he enters the adult world [age 18], because in that system, you’re completely lost without a diagnosis.
‘Feeling lost without a diagnosis’ is a well-described experience among families of children with rare diseases and disabilities in Denmark (Spalletta 2020) and elsewhere (Timmermans 2017; Latimer 2013). For Inge, Simon’s diagnosis meant she was less worried about her son’s future. The diagnosis consolidated her son’s access to support and benefits from the welfare state in Denmark, and secured him a right to reasonable adjustments in relation to education, economy, employment, and accommodation on the verge of his independent adult life.
To sum up, these patient and family experiences of disease names are akin to Hacking’s theory of dynamic nominalism. For Hacking (1994), disease labels are loaded with socially and culturally ascribed meanings that shape the person being labelled. In turn, the person can defy these labels, react to them, and come to reshape them too. In addition, in the dynamic field of new disease taxonomies, the semantically opaque genetic disease labels may come to represent a form of blank slate (see also Navon 2019). This is, these new labels have yet to be inscribed with societal norms and expectations. In the words of Daniel Navon (2019, 6), ‘a mutation can begin its social career as a thin case report […] but then metamorphose into a bona fide medical condition and eventually a richly detailed kind of person’. The fact that the labels are unsettled and carry murky meanings appears to be part of what makes them elastic, providing the patient and their families more room for individual identity work. This is evident in the eclectic ways parents activated and disabled the diagnosis to gain recognition and help from state authorities and to enable and disable participation in patient communities. Patients like Simon and Ole, and their families, use the labels for selected and context-specific purposes (e.g., when dealing with the local authorities or in conversations with curious friends looking at their toes). Contributing to the scholarly efforts to thicken Hacking’s analysis of the ‘looping effect of human kinds’ (see e.g., Eyal et al. 2014), with this finding, my study points to the less explored space for creativity that these names may afford, to which I turn in the next section.
An escape from unwanted moral regimes
I met 16-year-old boy Anders and his parents at a genetic counselling consultation in the spring of 2018. On our way to the consulting room, the geneticist Esther told me, ‘This is about pain’. Anders was a tall teenager with curly hair. He entered the room with a walker, a crutch, and a heavy winter coat that never came off during the hour-long consultation. He laid his head on the table and yawned many times. Moreover, he avoided eye contact with Esther and me. Esther asked the family to tell their story. ‘My body hurts constantly, my legs, hips, and back’, Anders said. His father continued, ‘He has trouble walking. Even as a little kid, he couldn’t walk very far or run like the other kids. He gets tired easily’. His mother added, ‘And he’s hypermobile like his father, who also couldn’t walk for a period of three months when he was 13’. During the consultation, we learned that Anders had not attended school for three years. Numerous doctors had examined him. They had suggested diagnoses ranging from depression, ADHD, to chronic pain syndrome. Just like many of the other families I met, Anders’s mother, Solvej, told me that she longs for a genetic diagnosis:
If only we could find some ‘marker’ for it; that this is something physical, somatic, and related to genetic dispositions … We have people invading our private space constantly. I mean, they walk in and out of our life. For Anders’s sake … it’s important that we can say, ‘Well, this is what it is’, … then we can avoid running into these people who just say, ‘pain begins in the head’. … Both the municipality and the doctors, they stick their noses into our life as if it was the most natural thing to do … If they start coming here … [in our house] I will god damn put up a gate. That’s where it ends. This is our space. When you start feeling this way, it’s because someone is getting too close. I don’t need other people to have an opinion about us [as a family].
Solvej expects a genetic diagnosis will relieve both her son and their family from the unwanted moral judgements exercised by the health and social authorities. Here, it is not the name inasmuch as it is the ‘genetic-ness’ of the disease that may afford them a particular escape from stigma. This finding is in line with, for example, Navon’s work on how discourses of autism’s genetic origin help parents escape degrading labels such as ‘refrigerator moms’ (2019, see also Eyal 2013). As opposed to Simon’s parents, who used the genetic name to get the help they needed from the municipality, for Solvej, a genetic label is key to getting the authorities to back off. Through the relabelling of her son’s condition (from a psychiatric diagnosis to a biological, genetic label), she hopes to renegotiate the existing social contract with the authorities and the label they have been given as ‘bad parents’. To understand what is at stake for parents who, like Solvej, find biological labels attractive, I turn to studies on the destigmatising effects of biological and genetic disease aetiologies (Lippman 1991; Hacking 1995; Phelan 2005; Petryna 2003; Navon and Eyal 2016). I specifically focus on Michel Foucault’s and Nicolas Rose’s idea of ‘spatialisation’.
Over a decade ago, Rose (2007) noted that biomedicine increasingly targets diagnosis and interventions at the ‘molecular’ level (i.e. involving DNA, genes), moving our view of disease as being spatially located in the ‘molar’ body (i.e. involving limbs, organs, tissues). Foucault’s original idea of vitality located disease in the ‘molar’ body, as a mechanism that humans could engineer (Foucault 1973, cited in Rose 2007, 11–12). As opposed to the molar body, the molecular body is outside of the individual’s control to transform and discipline. From these ideas about the localisation of disease in the body grew Foucault’s notion of ‘spatialisation’. As Rose explains, ‘illness and medicine came to be spatialized upon the individual body’ and ‘the body itself remains the focus of the clinical gaze. […] Even when the disease is situated in a field of attitudes, habits, and behaviors, as in attention to dangerous sexual or dietary practices, it is the body itself that becomes ill’ (2007, 9–10).
If we follow this line of thought on spatialisation, we may say that Solvej hopes that genomic medicine will relocate her son’s disease from the molar body (inside of an individual’s control) to the molecular body (beyond individual control). More specifically, Anders’s mother hopes to relocate disease from her son’s mind or the dynamics of their family to his genes. Disease within the molar body is well established (e.g., diabetes, heart disease, and cancer), and these diseases carry with them moral associations about how to live in the right or wrong way. But for diseases located at the molecular level, the weight of disease cannot be placed on individual habits, behaviours, and responsibility. Using spatial metaphors herself, Solvej draws the boundaries around the body of her family. She depicts state care as a suffocating and controlling regime that comes too close and from which she needs to fence in her family’s privacy. Thus, Solvej adds a third ‘body’ to the idea of spatialising disease; that is, beyond the molar and molecular, there is the authority’s localisation of disease in the body of the family.
In contrast, type 2 diabetes is a disease that is generally considered to be within the individual’s control and, as such, carries moral connotations. Hence, like Simon’s mother, participants in the TRANSLATE research project hoped to get a genomic label to designate their diabetes condition. This was the case for Lotte, as she explained in an interview:
Lotte: The TRANSLATE people said I have a special mutation … that explains why doctors thought I had diabetes, but it turns out that I don’t have diabetes after all.
Laura: What did it mean to you to hear that you had a MODY-variant [HNF1A]?
Lotte: It meant that I no longer had to feel ashamed if I crave chocolate or cake, because when I tell people I have diabetes then their face says, ‘How can you eat candy and sugar when you have diabetes, you are not supposed to’ [voice goes up—sounds indignant]. Often I choose not to tell people I have diabetes. Now it turns out I don’t have diabetes and it made me so happy that I don’t need to feel different.
I had expected that patients who were relabelled from type 2 diabetes to a MODY genetic variation, like Lotte, would on the whole express relief at ‘no longer being sick’. I was surprised, however, to find that the main response to the diagnosis was that they now felt destigmatised. In fact, for Lotte, the best part about her new diagnosis was that it set her free from the social and cultural expectations regarding her lifestyle; she no longer felt subject to the moral stigma attached to diabetes.
Upon being diagnosed with type-2 diabetes, all my interlocutors had been referred to so-called patient education, with the expectation of achieving increased self-discipline (see e.g., Broom and Whittaker 2004; Ingadottir and Halldorsdottir 2008). In Denmark, the colloquial name for type 2 diabetes ( gammelmandssukkersyge ) translates as ‘old man’s sugar disease’, which inherently links the disease to aging, individual lifestyle, and behaviour. Because of these connotations, for people with diabetes, social encounters involving shared meals hold the potential for judgement. In a sense, Lotte uses her new labels ‘HNF1A mutation’ (one of the 11 known MODY variants) and ‘not diabetic’ to escape the disciplining of diabetes patients’ lives.
For Dina, a 50-year-old woman who was relabelled G214A (a new MODY variant) after having lived with the diagnosis type 2 diabetes for 40 years, it felt like a validation of her own ‘reading’ of her body. Dina was diagnosed with type 2 diabetes at the age of 12, but her symptoms were not standard, and sometimes a new doctor would suggest that she could be a type 1. She did not take medication; it only made her feel worse. Instead, she reorganised her life. As a teenager, her parents would control her intake of cake and alcohol and monitor her sleep. During her three pregnancies, she strictly monitored her blood sugar levels, diet, and exercise to avoid having to take medication that could affect her unborn child. In an interview with Dina, I mentioned the vision of personalised medicine to target treatment to the individual based on genetic testing. Dina promptly responded:
That’s exactly what this is about! Genetic testing can do what no other health care person has ever been able to do before. They [healthcare staff] have generally considered me a serial number and misrecognised my accounts of how my body responds [to the medicine and blood sugar levels].
For Dina, as for many of the people I met who had previously been diagnosed with type 2 diabetes and were now being relabelled, her disease had until recently been located in the molar body, and thus something that she could act upon to change. However, while the diagnosis had certainly made Dina reorganise her life, she had declined medication and resisted standard treatment. Being relabelled as G214A serves as a reassurance that she knows her body well; it confirms her disease identity and self-image. Furthermore, Dina adds that the new genetic label somehow sets her free from the confinements of standard care. In light of the present knowledge of her genetic mutation, Dina sees the attempts made by doctors in the past to offer her standard treatment for type 2 diabetes as both ‘overtreatment’ and ‘maltreatment’, in that they treated her as they would treat any other patient. She concludes that these doctors did not see her as a unique person, but as a serial number. In contrast, genomic medicine finally recognised her distinctness as an individual person.
In contrast to existing social studies on genomic medicine (see, e.g.,, Lock 2013, 2015; Saldaña-Tejeda and Wade 2019), Dina and the other participants in my study did not see the genetic label as reducing them as persons, but as facilitating a personal type of care compared to the standard forms of care they had received so far. When I shared my reflections on this with Anders’s mother, Solvej, for instance, she also expressed an experience of genomic medicine as a type of care that is personal.
Solvej: That’s what is so nice about seeing Esther [geneticist] because she’s actually interested in Anders. She’s not interested in just how dysfunctional our family may be.
Laura: Well, she doesn’t look at psychology or psychiatry, only at DNA.
Solvej: That’s right, and that is absolutely fantastic (laughs), it’s pure mathematics (both laughing).
Laura: You can’t find anything more reductionist (laughing).
Solvej: I know, talk about getting to the heart of the matter, right? So yes, it’s really great when you meet someone where it’s about Anders. That’s amazing and we appreciate it (laughs) . […] It’s amazing to finally have someone look inside my son. Until now, the doctors have only looked at him from the outside.
For Solvej, the care offered by the geneticist, the hour-long consultation with Esther who listens to Anders and his family tell their story from the very beginning, shows a sincere interest in her son as a person. Solvej thinks of genetic knowledge as a form of knowledge that—as opposed to the social authorities or the psychiatrists who look at social problems—‘comes close’ to identifying who her son is by ‘getting to the heart of the matter’ or by looking ‘inside’ Anders, as she puts it. Again, Solvej draws on spatial metaphors to describe various medical gazes and deems some more authentic and personal than others. How should we understand this idea that the new gene names—anticipated to appear ‘cumbersome and less meaningful’ or even reductionist to patients—offer some patients and families an experience of a more personal type of care than the standard may provide them?
To address this question, I turn to the work of social scientists who have studied the relationship between numbering practices and the human experience of being numbered. In her work, Lisa Stevenson (2014) offers two controversial cases of serialisation performed by health authorities for public health purposes. First, she describes the case of identity tags introduced by the Canadian government to keep records of the Inuit population in Nunavut during a tuberculosis epidemic from the 1940s to the 1960s. And second, she recounts the practices of turning Inuit individuals into statistics during a so-called suicide epidemic, which still haunts Nunavut today. Stevenson suggests that these practices of serialisation are a form of ‘anonymous care’ (2014, 187). She characterises the Canadian government’s response to both the historic tuberculosis and the more recent suicide epidemics as a type of care mainly concerned with ‘the maintenance of life itself’, and a biopolitical form of governance that was directed at populations rather than individuals (Ibid, 3). Stevenson lays out how the government counted with huge precision ‘the sick and the dead Inuit without knowing who had died and who was buried where ’ (Ibid, 25, original emphasis), leaving personal stories of Inuit deaths an enigma. Asking how Inuit youth respond to public health interventions aimed at suicide in Canada, Stevenson concludes that such bureaucratic forms of care come across as anonymous and indifferent and should be seen as a symptom of an uncaring or even violent colonial authority. She gives the example of the Kamatsiaqtut help line, a suicide hotline established in 1989 as a form of care that is delivered in a way that is ‘too professional’ or anonymous; i.e., is delivered by volunteers with no background knowledge of the people they are helping. Stevenson claims that this is so that the volunteers can ensure a ‘discreet and anonymous service’ for anyone ‘experiencing emotional distress’ (2014, 83) and keep professionally distanced.
I am aware that the case of the Canadian government’s attempts to serialise Inuit bodies and the Danish patient receiving a genetic disease label are incomparable in so many ways. However, both are examples of how public health interventions involving serialisation practices can sometimes come across as anonymous and disempowering whilst other times as personal and empowering.
To further the discussion on the way numbering practices act as technologies of governance and become pervasive in care regimes, I draw on the work of Adriana Petryna (2003) on ‘biological citizenship’ in the aftermath of the Chernobyl disaster in Ukraine. Petryna argues that for the government and for citizens, the quantification of the risk of radiation and proof of biological injury became resources in a social and political game of legitimacy (2003, 206). Citizens in Ukraine, she argues, mobilised their individual levels of exposure through technologies such as ‘dosimetric passports’ (Ibid, 83) that contain individual measurements of radiation to access social welfare (i.e., ‘disability claims’) (Petryna 2003, 5, 90). In both cases of public health interventions in the Canadian Arctic and in Ukraine, statistics and numbering practices came to shape care regimes. However, whereas the serialisation of tuberculosis and suicidal deaths are viewed as mechanisms of anonymous care in Stevenson’s work, the serialisation or ‘quantifications of radiation risk’, and even the scientific uncertainty surrounding what qualifies as a risk, became empowering for the citizens categorised as ‘sufferers’ or ’disabled’ in Petryna’s work (Ibid, 255). In the Ukrainian case, serialisation creates anonymisation and in turn empowers citizens when they use statistics to gain access to a political economy of illness. As Petryna argues, this also has the effect of displacing patients’ self-perception and threatening other identities they may have such as being a ‘breadwinner’ and a ‘paternal figure’ (Ibid, 256).
Managing populations through the management of risk and biology are also at the heart of genomic medicine. However, serialisation seems to enact the opposite of anonymisation here. In the experience of Henrik, Solvej, and Dina, serialisation both empowers them and gives them a unique identity. In the Danish context, the political turn to precision medicine—tellingly also called personalised medicine—draws on the paradigm and rhetoric of person-centred care when advocating that future medicine should be tailored to the individual. Also, as the opening example illustrates, when the 65-year-old Henrik receives the diagnosis of G246A, this particular enumeration practice makes him feel special and unique. This experience of uniqueness is underlined by the doctor with the words: ‘I can see that you’re the only one of your kind in Denmark and in the world’, and in Henrik’s own response, ‘Damn, I’m an interesting person!’
In this case, we see that to patients like Henrik, the ‘specialness’ of these genetic mutations fold into attributes of ‘personalised care’. 3 Moreover, as most standard consultations in Danish healthcare last between 10 and 15 minutes, the four-hour-long physical exam and the close monitoring of what he eats and drinks by two young and friendly doctors could be one reason why Henrik feels interesting and unique too. Indeed, this form of care contrasts with the indifferent and professionally distant handling of the suicide hotline callers in Stevenson’s work and the empowering yet anonymous distribution of economic compensation for citizens broadly labelled as ‘disabled’ or ‘sufferer’ in Petryna’s example from the Chernobyl disaster. All the interlocutors in my study recounted the amount of time their medical doctor spent with them as extraordinary. This finding suggests that temporality feeds into patients’ notion of ‘personalised care’. In addition, the physical presence of a medical expert in a consulting room on a one-on-one basis was interpreted in the same way—as a genuine interest in the individual person. This resonates with research carried out with clinical trial participants, who find the care they receive in research trials better than in standard care (Wadmann and Hoeyer 2014; Bogicevic and Svendsen 2021). But there is something more to the experience of individualisation and personalisation taking place here. I suggest that the practice of serialisation in genomic medicine is experienced as singularising.
In a way, Dina’s conception of standard care as treating her as simply a number and not a person and Henrik’s (and Simon’s) feeling of being recognised as someone special, are in line with the connection between serialisation and anonymous care that Stevenson makes. Standard, bureaucratic care that targets large patient populations with broad disease categories is experienced as a form of serialisation that results in anonymous and indifferent types of care. However, in contrast to this, the families involved in clinical genetic care and the patients that participate in diabetes research use their opaque new gene label to escape ‘standard’ care and treatment. The new labels and the ‘longer than standard’ consultations seem to make the patients feel unique and singular, as opposed to being just an anonymous statistic. To patients and their families, these genomic naming practices seem to represent a hidden knowledge that can be extracted from a molecular locus in the depths of their bodies to reveal some truth about who they are. Or rather: who they are not (for instance, bad parents or overeaters). As such, I suggest that the experience of genomic naming practices is constituted through practices of not only spatialisation but also serialisation.
Importantly, biopolitics, in the form of a strong imperative to maintain life, is as much a pillar of precision medicine as it is the pillar of the Canadian public health strategy to prevent suicide or the Ukrainian State strategy to compensate bodies exposed to radiation. For Stevenson, the example of the tag system imposed by the Canadian government on the Inuit from the 1940s to the 1960s demonstrates that numbers erase individuality (2014, 27). Contrary to this, in genomic medicine—as illustrated by the case of Henrik and Dina—seriality produces singularity and marks out individuality. The example of Henrik illustrates this clearly. He is the only person in the world known with that exact (rare) disease label. Ironically, the identifying that serialisation practices concede in genomic medicine has made my own attempts to anonymise my interlocutors difficult. 4
‘Statistics are a technique of surveillance’, Stevenson (2014, 29) reminds us. The mapping of the human genome is indeed also a technique of surveillance. Therefore, in as much as the new genetic labels (combinations of numbers and letters) may make patients feel liberated from unwanted forms of surveillance and moral regimes and may make them feel singularised (or individualised), exome and whole genome sequencing technologies 5 still hold the patient in a system of surveillance and tracking for public health purposes. For instance, the patients who undergo exome sequencing in Denmark sign an agreement to share their genome code with the National Genome Center (NGC)—a government agency established in 2019 by the Danish government with the aim of securing an infrastructure that collects, stores, tracks, and registers genomes of Danish citizens in the name of future developments in public health, research, and industry. In the near future, the NGC may decide to contact patients like Henrik and Lotte if they find a genetic variation that predicts cancer, as part of a strategy to ‘return knowledge’. Such ‘returned knowledge’ will yet again add new loops to the continuous work of making sense of new disease categories.
Conclusion
The political turn to precision medicine has far-reaching ethical, social, and economical consequences and warrants continuous scholarly scrutiny. In this Research Article, I have explored the declared aim of precision medicine to make disease taxonomies more dynamic and finer-grained. One of the results of these efforts is the creation of thousands of new gene names such as DPF2 or G246A. For the patients and families in my fieldwork who are given these names for their health conditions, these new disease labels offer a space for creative identity and meaning making. This is because, as I have argued, these new disease labels carry little history and have an unsettled and murky social and cultural meaning. In this article, I have shown that it is exactly because the labels are semantically negligible and represent a blank slate that patients feel that their identity is not fully defined nor determined by these labels. Instead, patients can utilise (or not) their diagnosis as they see fit, in various contexts and in creative ways. Moreover, the unsettled social context of the disease offers patients a chance to imbue their new diagnosis with their own understanding of their bodily symptoms and disease. For families with children with developmental and behavioural problems and for patients formerly diagnosed with the lifestyle-related disease type 2 diabetes, getting a genetic label repositions them within moral regimes. These patients and families may experience an acknowledgement that they neither belong to dysfunctional families nor are they non-compliant diabetics. Furthermore, receiving an extremely rare disease label makes the patients feel like they are special and no longer just a number in the row of patients who are offered standard care.
On the one hand, the experience of being ‘one of a kind’ does not negate the relevance of Hacking’s theory that disease categories create ‘kinds’ of people. But while Hacking suggests that people become ‘kinds’ of people with a predefined social and cultural meaning when they are labelled with a disease, and that such membership transforms the labelled person and vice versa (Hacking 1995), it is worth noting that, for my interlocutors, although the new genetic disease labels carry plenty of meaning, very little of this is predefined. The labels seem to produce ‘kind’ in singular. In other words, ‘kinds of people’ are not nullified with precision medicine; instead, precision medicine produces disease categories that are governed in a way that make patients feel like they are ‘one of a kind’.
Locating the source of the disease not only in the individual body, but also within the molecular, genetic code, makes patients feel relieved of responsibility and blame. This relocation becomes particularly useful and potent for people who have been labelled as ‘bad parents’ or ‘bad diabetics’, whose disease aetiology is moved from a highly moralised landscape to uncharted territory. Based on this finding, I have argued that the patients and families’ experiences of genomic naming practices are constituted through practices of both spatialisation and serialisation.
Returning to the geneticist’s prediction in the opening quotation, ‘it doesn’t change who you are as a person’, this statement appears to be challenged by the empirical findings of this study. While the new genetic names may not stigmatise the patients, they do change their ideas of who they are in surprising and subtle ways that the geneticists had not anticipated.
Authorship statement
The article was conceived and written in its entirety by the author.
Ethics statement
All data were handled and kept according to the rules of the Danish Data Protection Agency.
Acknowledgements
I would like to thank the people who willingly told their stories of getting a genetic diagnosis. I thank the clinicians at the genetic department and the researchers in the TRANSLATE project who invited me to follow their work. The initial ideas about pursuing naming practices in genetics were conceived during much appreciated walks in the streets of Toronto with Janelle Taylor during a time of pandemic. This work has benefitted greatly from the editorial guidance of Olivia Spalletta, Mie Seest Dam, Iben Mundbjerg Gjødsbøl, and Mette N. Svendsen. They all contributed substantially to this paper. I would like to thank all members of the MeInWe research group for stimulating discussions on precision medicine and for giving helpful comments on this paper. Finally, I am very grateful to the anonymous reviewers for their close readings and very helpful comments. The research and writing of this article was supported by the Carlsberg Foundation (Semper Ardens grant ‘MeInWe’ CF17-0016).
About the author
Laura Emdal Navne is associate professor at The Danish Center for Social Science Research, Copenhagen and affiliated associate professor at the Center for Medical Science and Technology Studies at the Department of Public Health, University of Copenhagen.
Laura Emdal NavneReferences
Abel, Sarah, George F. Tyson, and Gisli Palsson. 2019. ‘From Enslavement to Emancipation: Naming Practices in the Danish West Indies’. Comparative Studies in Society & History 61 (2): 332–65. https://doi.org/10.1017/S0010417519000070 .
Comparative Studies in Society & History https://doi.org/10.1017/S0010417519000070Antze, Paul, and Michael Lambek (eds.). 2016. Tense Past: Cultural Essays in Trauma and Memory . New York, NY: Routledge.
Tense Past: Cultural Essays in Trauma and MemoryBogicevic, Ivana, and Mette N. Svendsen. 2021. ‘Taming Time: Configuring Cancer Patients as Research Subjects’. Medical Anthropology Quarterly 35 (3): 386–401. https://doi.org/10.1111/maq.12647 .
Medical Anthropology Quarterly https://doi.org/10.1111/maq.12647Bowker, Geoffrey C., and Susan Leigh Star. 2000. Sorting Things Out: Classification and its Consequences . Cambridge, MA: MIT Press.
Sorting Things Out: Classification and its ConsequencesBroom, Dorothy, and Andrea Whittaker. 2004. ‘Controlling Diabetes, Controlling Diabetics: Moral Language in the Management of Diabetes Type 2’. Social Science & Medicine 58 (11): 2371–82. https://doi.org/10.1016/j.socscimed.2003.09.002 .
Social Science & Medicine https://doi.org/10.1016/j.socscimed.2003.09.002Chan, Isaac S., and Geoffrey S. Ginsburg. 2011. ‘Personalized Medicine: Progress and Promise’. Annual Review of Genomics & Human Genetics (12): 217–44. https://doi.org/10.1146/annurev-genom-082410-101446 .
Annual Review of Genomics & Human Genetics https://doi.org/10.1146/annurev-genom-082410-101446Chial, Heidi. 2008. ‘DNA sequencing technologies key to the Human Genome Project’. Nature Education 1 (1): 219. https://www.nature.com/scitable/topicpage/dna-sequencing-technologies-key-to-the-human-828/ .
Nature Education https://www.nature.com/scitable/topicpage/dna-sequencing-technologies-key-to-the-human-828/Danish Regions. 2015. Shared Declaration: Health Care of the Citizens – Our Health Care System. Copenhagen: Danish Regions.
https://www.regioner.dk/sundhed/medicin/personlig-medicin .
https://www.regioner.dk/sundhed/medicin/personlig-medicinDickenson, Donna. 2013. Me Medicine Vs. We Medicine: Reclaiming Biotechnology for the Common Good. New York, NY: Columbia University Press.
Me Medicine Vs. We Medicine: Reclaiming Biotechnology for the Common Good.Dumit, Joseph. 2012. Drugs for Life. How Pharmaceutical Companies Define Our Health. Durham, NC: Duke University Press.
Drugs for Life. How Pharmaceutical Companies Define Our Health.Erikainen, Sonja, and Sarah Chan. ‘Contested Futures: Envisioning “Personalized,” “Stratified”, and “Precision” Medicine’. New Genetics and Society 38 (3): 308–30. https://doi.org/10.1080/14636778.2019.1637720 .
New Genetics and Society https://doi.org/10.1080/14636778.2019.1637720Eyal, Gil. 2013. ‘For a Sociology of Expertise: The Social Origins of the Autism Epidemic’. American Journal of Sociology 118 (4): 863–907. https://doi.org/10.1086/668448 .
American Journal of Sociology https://doi.org/10.1086/668448Eyal, Gil, Des Fitzgerald, Eva M. Gillis-Buck, Brendan Hart, Martin Lappé, Daniel Navon, and Sarah S. Richardson. 2014. ‘New Modes of Understanding and Acting on Human Difference in Autism Research, Advocacy and Care: Introduction’. BioSocieties 9 (3): 233–40. https://doi.org/10.1057/biosoc.2014.19 .
BioSocieties https://doi.org/10.1057/biosoc.2014.19Featherstone, Katie, Paul Atkinson, Aditya Bharadwaj, and Angus Clarke. 2006. Risky Relations: Family, Kinship and the New Genetics . Oxford: Berg.
Risky Relations: Family, Kinship and the New GeneticsFinkler, Kaja. 2000. Experiencing the New Genetics: Family and Kinship on the Medical Frontier . Philadelphia, PA: University of Pennsylvania Press.
Experiencing the New Genetics: Family and Kinship on the Medical FrontierFoucault, Michel. 1977. Discipline and Punish: The Birth of the Prison. Translated by A. Sheridan. London: Allen Lane.
Discipline and Punish: The Birth of the Prison.Foucault, Michel. 1973. The Birth of The Clinic: An Archeology of Medical Perception. London: Tavistock Publications.
The Birth of The Clinic: An Archeology of Medical Perception.Foucault, Michel. 1988. ‘Technologies of the Self’. In Technologies of the Self, edited by Luther H. Martin, Huck Gutman, and Patrick H. Hutton, 16–49. Amherst, MA: University of Massachusetts Press.
Technologies of the Self,Foucault, Michel. 2008. The Birth of Biopolitics . Translated by G. Burchell. New York, NY: Palgrave Macmillan.
The Birth of BiopoliticsFranklin, Sarah, and Susan McKinnon (eds.). 2001. Relative Values: Reconfiguring Kinship Studies . Durham, NC: Duke University Press.
Relative Values: Reconfiguring Kinship StudiesGibbon, Sarah. 2009. ‘Genomics as Public Health? Community Genetics and the Challenge of Personalised Medicine in Cuba’. Anthropology & Medicine 16: 131–47. https://doi.org/10.1080/13648470902940671 .
Anthropology & Medicine https://doi.org/10.1080/13648470902940671Goffman, Erwing. 1993. Stigma: Notes on the Management of Spoiled Identity. New York, NY: Touchstone.
Stigma: Notes on the Management of Spoiled Identity.Green, Sara, Anna Maria Carusi, and Klaus Hoeyer. 2019. ‘Plastic Diagnostics: The Remaking of Disease and Evidence in Personalized Medicine’. Social Science & Medicine 304. https://doi.org/10.1016/j.socscimed.2019.05.023 .
Social Science & Medicine https://doi.org/10.1016/j.socscimed.2019.05.023Green, Sara, and Mette N. Svendsen. 2021. ‘Digital Phenotyping and Data Inheritance’. Big Data & Society 8 (2): 1–5. https://doi.org/10.1177/20539517211036799 .
Big Data & Society https://doi.org/10.1177/20539517211036799Hacking, Ian. 1986. ‘Making Up People’. London Review of Books 28 (16). https://www.lrb.co.uk/the-paper/v28/n16/ian-hacking/making-up-people .
London Review of Books https://www.lrb.co.uk/the-paper/v28/n16/ian-hacking/making-up-peopleHacking, Ian. 1995. ‘The Looping Effects of Human Kinds’. In Causal Cognition: A Multidisciplinary Debate , edited by Dan Sperber, David Premack and Ann J. Premack, 351–94. Oxford: Oxford University Press.
Causal Cognition: A Multidisciplinary DebateHedgecoe, Adam M. 2003. ‘Expansion and Certainty: Cystic Fibrosis, Classification and Genetics’. Sociology of Health & Illness 25 (1): 50–70. https://doi.org/10.1111/1467-9566.t01-2-00324 .
Sociology of Health & Illness https://doi.org/10.1111/1467-9566.t01-2-00324Hoeyer, Klaus. 2019. ‘Data as Promise: Reconfiguring Danish Public Health through Personalized Medicine’. Social Studies of Science 49 (4): 531–55. https://doi/pdf/10.1177/0306312719858697 .
Social Studies of Science https://doi/pdf/10.1177/0306312719858697Ingadottir, Brynja, and Sigridur Halldorsdottir. 2008. ‘To Discipline a “Dog”: the Essential Structure of Mastering Diabetes’. Qualitative Health Research 18 (5): 606–19. https://doi.org/10.1177/1049732308316 .
Qualitative Health Research https://doi.org/10.1177/1049732308316Kohrman, Matthew. 2003. ‘Why Am I Not Disabled? Making State Subjects, Making Statistics in Post-Mao China’. Medical Anthropology Quarterly 17 (1): 5–24. https://doi.org/10.1525/maq.2003.17.1.5 .
Medical Anthropology Quarterly https://doi.org/10.1525/maq.2003.17.1.5Latimer, Joanna. 2013. The Gene, the Clinic and the Family: Diagnosing Dysmorphology, Reviving Medical Dominance . Milton Park: Routledge.
The Gene, the Clinic and the Family: Diagnosing Dysmorphology, Reviving Medical DominanceLock, Margaret. 2013. ‘The Epigenome and Nature/Nurture Reunification: A Challenge for Anthropology’. Medical Anthropology 32 (4): 291–308. https://doi/abs/10.1080/01459740.2012.746973 .
Medical Anthropology https://doi/abs/10.1080/01459740.2012.746973Lock, Margaret. 2015. ‘Comprehending the Body in the Era of the Epigenome’. Current Anthropology 56 (2): 151–77. https://doi.org/10.1086/680350 .
Current Anthropology https://doi.org/10.1086/680350Lury, Celia, and Sophie Day. 2019. ‘Algorithmic Personalization as a Mode of Individuation’. Theory, Culture & Society 36 (2): 17–37. https://doi.org/10.1177/0263276418818888 .
Theory, Culture & Society https://doi.org/10.1177/0263276418818888Manderson, Lenore. 2020. ‘After Illness, Under Diagnosis’. Medicine Anthropology Theory 7 (2): 1–9. https://doi.org/10.17157/mat.7.2.685 .
Medicine Anthropology Theory https://doi.org/10.17157/mat.7.2.685Martin, Emily. 2007. Bipolar Expeditions: Mania and Depression in American Culture . Princeton, NJ: Princeton University Press.
Bipolar Expeditions: Mania and Depression in American CultureMcLaughlin, Janice, and Emma K. Clavering. 2012. ‘Visualising Difference, Similarity and Belonging in Paediatric Genetics’. Sociology of Health & Illness 34 (3): 459–74. https://doi.org/10.1111/j.1467-9566.2011.01388.x .
Sociology of Health & Illness https://doi.org/10.1111/j.1467-9566.2011.01388.xMinistry of Health and Danish Regions. 2016 . Personlig Medicin Til Gavn for Patienterne. Klar Diagnose, Målrettet Behandling, Styrket Forskning. National Strategi for Personlig Medicin 2017–2020. København: Ministry of Health and Danish Regions.
. Personlig Medicin Til Gavn for Patienterne. Klar Diagnose, Målrettet Behandling, Styrket Forskning. National Strategi for Personlig Medicin 2017–2020.https://ngc.dk/Media/A/E/Strategi%20Personlig%20medicin%202021-22.pdf .
https://ngc.dk/Media/A/E/Strategi%20Personlig%20medicin%202021-22.pdfNavne, Laura E., and Mette N. Svendsen. 2018. ‘Careography: Staff Experiences of Navigating Decisions in Neonatology in Denmark’. Medical Anthropology 37 (3): 253–66. https://doi.org/10.1080/01459740.2017.1313841 .
Medical Anthropology https://doi.org/10.1080/01459740.2017.1313841Navne, Laura E., and Mette N. Svendsen. 2022. ‘De Novo Kin: Sharing Data, Shielding Persons, and Forging Relatedness in Precision Medicine’. Journal of the Royal Anthropological Institute 28 (4): 1159–76. https://doi.org/10.1111/1467-9655.13817 .
Journal of the Royal Anthropological Institute https://doi.org/10.1111/1467-9655.13817Navon, Daniel. 2019. Mobilizing Mutations: Human Genetics in the Age of Patient Advocacy . Chicago, IL: The University of Chicago Press.
Mobilizing Mutations: Human Genetics in the Age of Patient AdvocacyNavon, Daniel and Gil Eyal. 2016. ‘Looping Genomes: Diagnostic Change and the Genetic Makeup of the Autism Population’. American Journal of Sociology 121 (5): 1416–71. https://doi.org/10.1086/684201 .
American Journal of Sociology https://doi.org/10.1086/684201Novas, Carlos. 2007. Governing Risky Genes: Predictive Genetics, Counselling Expertise and the Care of the Self . London: British Library Document Supply Centre.
Governing Risky Genes: Predictive Genetics, Counselling Expertise and the Care of the SelfPalsson, Gisli. 2014. ‘Personal Names: Embodiment, Differentiation, Exclusion, and Belonging’. Science, Technology, & Human Values 39 (4): 618–30. https://doi.org/10.1177/01622439135168 .
Science, Technology, & Human Values https://doi.org/10.1177/01622439135168Perlman, Robert L., and Diddahally R. Govindaraju. 2016. ‘Archibald E. Garrod: The Father of Precision Medicine’. Genetics in Medicine 18 (11): 1088–89. https://doi:10.1038/gim.2016.5 .
Genetics in Medicine https://doi:10.1038/gim.2016.5Phelan, Jo C. 2005. ‘Geneticization of Deviant Behavior and Consequences for Stigma: The Case of Mental Illness’. Journal of Health & Social Behavior 46 (4): 307–22. https://doi.org/10.1177/002214650504600401 .
Journal of Health & Social Behavior https://doi.org/10.1177/002214650504600401Pickersgill, Martin. D. 2014. ‘Debating DSM-5: Diagnosis and the Sociology of Critique’. Journal of Medical Ethics 40 (8): 521–5. http://doi.org/10.1136/medethics-2013-101762 .
Journal of Medical Ethics http://doi.org/10.1136/medethics-2013-101762Prainsack, Barbara. 2018. ‘The “We” in the “Me”: Solidarity and Health Care in the Era of Personalized Medicine’. Science, Technology, & Human Values 43 (1): 21–44. https://doi.org/10.1177/0162243917736139 .
Science, Technology, & Human Values https://doi.org/10.1177/0162243917736139Prainsack, Barbara. 2017. Personalized Medicine: Empowered Patients in the 21st Century? New York City, NY: NYU Press.
Personalized Medicine: Empowered Patients in the 21st Century?Rabinow, Paul. 1992. ‘Artificiality and Enlightenment: From Sociobiology to Biosociality’. In Incorporations (Zone 6) , edited by Jonathan Crary and Sanford Kwinter: 181–93. New York, NY: Zone Books.
Incorporations (Zone 6)Rasmussen, Sonja A., Ada Hamosh, Joanna Amberger, Cassandra Arnold, Carol Bocchini, Marla J.F. O ‘Neill, and Anne Stumpf. 2020. ‘What’s in a Name? Issues to Consider When Naming Mendelian Disorders’. Genetics in Medicine 22 (10): 1573–5. https://doi.org/10.1038/s41436-020-0851-0 .
Genetics in Medicine https://doi.org/10.1038/s41436-020-0851-0Reardon, Jenny. 2017. The Postgenomic Condition: Ethics, Justice, and Knowledge After the Genome . Chicago IL: University of Chicago Press.
The Postgenomic Condition: Ethics, Justice, and Knowledge After the GenomeRose, Nikolas. 2007. The Politics of Life Itself: Biomedicine, Power, and Subjectivity in the Twenty-First Century . Princeton, NJ: Princeton University Press.
The Politics of Life Itself: Biomedicine, Power, and Subjectivity in the Twenty-First CenturySpalletta, Olivia. 2021. ‘Patrons of the State: Reciprocity, Belonging, and Life with Down syndrome in Denmark’. PhD dissertation, Brandeis University.
Saldaña-Tejeda, Abril, and Peter Wade. 2019. ‘Eugenics, Epigenetics, and Obesity Predisposition among Mexican Mestizos’. Medical Anthropology 38 (8): 664–79. https://doi.org/10.1080/01459740.2019.1589466 .
Medical Anthropology https://doi.org/10.1080/01459740.2019.1589466Shepherd, Maggie H., Beverley M. Shields, Michelle Hudson, Ewan R. Pearson, Christopher Hyde, Sian Ellard, Andrew T. Hattersley et al. 2018. ‘A UK Nationwide Prospective Study of Treatment Change in MODY: Genetic Subtype and Clinical Characteristics Predict Optimal Glycaemic Control after Discontinuing Insulin and Metformin’. Diabetologia 61 (12): 2520–7. https://doi.org/10.1007/s00125-018-4728-6 .
Diabetologia https://doi.org/10.1007/s00125-018-4728-6Stevenson, Lisa. 2014. Life Beside Itself: Imagining Care in the Canadian Arctic . Oakland, California, CA: University of California Press.
Life Beside Itself: Imagining Care in the Canadian ArcticStivers, Tanya, and Stefan Timmermans. 2017. ‘The Actionability of Exome Sequencing Testing Results’. Sociology of Health & Illness 39 (8): 1542–56. https://doi.org/10.1111/1467-9566.12614 .
Sociology of Health & Illness https://doi.org/10.1111/1467-9566.12614Stride, Amanda, Beverley Shields, Olivia Gill-Carey, Ali J. Chakera, Kevin Colclough, Sian Ellard and Andrew T. Hattersley. 2014. ‘Cross-sectional and Longitudinal Studies Suggest Pharmacological Treatment used in Patients with Glucokinase Mutations does not Alter Glycaemia’. Diabetologia 57 (1): 54–6. https://doi.org/10.1007/s00125-013-3075-x .
Diabetologia https://doi.org/10.1007/s00125-013-3075-xTimmermans, Stefan, Caroline Tietbohl, and Eleni Skaperdas. 2017. ‘Narrating Uncertainty: Variants of Uncertain Significance (VUS) in Clinical Exome Sequencing’. Biosocieties 12 (3): 439–58. https://doi.org/10.1057/s41292-016-0020-5 .
Biosocieties https://doi.org/10.1057/s41292-016-0020-5Tutton, Richard. 2014. Genomics and the Reimagining of Personalized Medicine . London: Routledge.
Genomics and the Reimagining of Personalized MedicineVallgårda, Signild. 2011. ‘Why the concept ‘‘lifestyle diseases’’ should be avoided’. Scandinavian Journal of Public Health 39 (7): 773–5. https://doi.org/10.1177/1403494811421978 .
Scandinavian Journal of Public Health https://doi.org/10.1177/1403494811421978Wadmann, Sarah, and Amalie. M. Hauge. 2021. ‘Strategies of Stratification: Regulating Market Access in the Era of Personalized Medicine’. Social Studies of Science 51(4): 628–53. https://doi.org/10.1177/03063127211005539 .
Social Studies of Science https://doi.org/10.1177/03063127211005539Wadmann, Sarah, and Klaus Hoeyer. 2014. ‘Beyond the “Therapeutic Misconception”: Research, Care and Moral Friction’. BioSocieties 9 (1): 3–23. https://doi.org/10.1057/biosoc.2013.37 .
BioSocieties https://doi.org/10.1057/biosoc.2013.37-
All names in this article are pseudonyms. With consent from patients and families, I have kept the names of the genetic variations affecting interlocutors. While anonymity seems salient when working with minors, the children with rare diseases in this article were between 16 and 18 years old and gave consent to their genetic variation and stories being published in an article. Moreover, a geneticist reminded me that making up a fictitious name for the gene variation is almost impossible. The risk of accidently using a ‘real’ one is huge considering the speed with which new genetic variations are identified, which underlines the ever changing landscape of genetic naming practices. ↩︎
-
See more: https://innovationsfonden.dk/da/i/historier/gendiagnostik-skal-personalisere . ↩︎
-
I am grateful to the generous reviewers for making me aware of this point. ↩︎
-
See again footnote 1. Thanks to the generous editors and reviewers for suggesting this methodological connection. ↩︎
-
Whole genome sequencing (WGS) is a laboratory process used to determine nearly the entirety of the DNA sequence of an individual’s genome at a single time, including the non-coding sequences (see e.g., https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/whole-genome-sequencing ). ↩︎
-
All names in this article are pseudonyms. With consent from patients and families, I have kept the names of the genetic variations affecting interlocutors. While anonymity seems salient when working with minors, the children with rare diseases in this article were between 16 and 18 years old and gave consent to their genetic variation and stories being published in an article. Moreover, a geneticist reminded me that making up a fictitious name for the gene variation is almost impossible. The risk of accidently using a ‘real’ one is huge considering the speed with which new genetic variations are identified, which underlines the ever changing landscape of genetic naming practices. ↩︎
-
See more: https://innovationsfonden.dk/da/i/historier/gendiagnostik-skal-personalisere . ↩︎
-
I am grateful to the generous reviewers for making me aware of this point. ↩︎
-
See again footnote 1. Thanks to the generous editors and reviewers for suggesting this methodological connection. ↩︎
-
Whole genome sequencing (WGS) is a laboratory process used to determine nearly the entirety of the DNA sequence of an individual’s genome at a single time, including the non-coding sequences (see e.g., https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/whole-genome-sequencing ). ↩︎
All names in this article are pseudonyms. With consent from patients and families, I have kept the names of the genetic variations affecting interlocutors. While anonymity seems salient when working with minors, the children with rare diseases in this article were between 16 and 18 years old and gave consent to their genetic variation and stories being published in an article. Moreover, a geneticist reminded me that making up a fictitious name for the gene variation is almost impossible. The risk of accidently using a ‘real’ one is huge considering the speed with which new genetic variations are identified, which underlines the ever changing landscape of genetic naming practices. ↩︎
All names in this article are pseudonyms. With consent from patients and families, I have kept the names of the genetic variations affecting interlocutors. While anonymity seems salient when working with minors, the children with rare diseases in this article were between 16 and 18 years old and gave consent to their genetic variation and stories being published in an article. Moreover, a geneticist reminded me that making up a fictitious name for the gene variation is almost impossible. The risk of accidently using a ‘real’ one is huge considering the speed with which new genetic variations are identified, which underlines the ever changing landscape of genetic naming practices. ↩︎
↩︎See more: https://innovationsfonden.dk/da/i/historier/gendiagnostik-skal-personalisere . ↩︎
See more: https://innovationsfonden.dk/da/i/historier/gendiagnostik-skal-personalisere . ↩︎
https://innovationsfonden.dk/da/i/historier/gendiagnostik-skal-personalisere ↩︎I am grateful to the generous reviewers for making me aware of this point. ↩︎
I am grateful to the generous reviewers for making me aware of this point. ↩︎
↩︎See again footnote 1. Thanks to the generous editors and reviewers for suggesting this methodological connection. ↩︎
See again footnote 1. Thanks to the generous editors and reviewers for suggesting this methodological connection. ↩︎
↩︎Whole genome sequencing (WGS) is a laboratory process used to determine nearly the entirety of the DNA sequence of an individual’s genome at a single time, including the non-coding sequences (see e.g., https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/whole-genome-sequencing ). ↩︎
Whole genome sequencing (WGS) is a laboratory process used to determine nearly the entirety of the DNA sequence of an individual’s genome at a single time, including the non-coding sequences (see e.g., https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/whole-genome-sequencing ). ↩︎
https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/whole-genome-sequencing ↩︎