Irritating Bowels
Attention and Everyday Management of Gut Trouble in Denmark
—
Abstract
Irritable bowel syndrome (IBS) constitutes an irritating and embarrassing problem for an estimated 11–16% of the Danish population. Based on long-term ethnographic fieldwork, this article explores how young and middle-aged people diagnosed with IBS attend to, experience, and manage gut trouble in a Danish welfare context. It asks how we may understand the relation between IBS, irritation, and attention. Drawing on conceptualisations of ‘dys-appearance’ (Leder 1990) and ‘attentional pulls’ (Throop and Duranti 2015), I explore how afflicted individuals’ attention is pulled towards unwanted and unexpected gut sensations in everyday life, and how a Danish welfare context, manifesting itself in notions of ‘faring well’ (Langer and Højlund 2011) and moral imaginings of ‘good lives’ (Mattingly 2014), may contribute to this. Furthermore, I show how people are impelled to experiment with consciously paying attention to the gut and deciphering its signals to try to alleviate gut trouble. I suggest that irritation may not only be an empirical focal point, but also a heuristic tool for troubling and refining concepts.
Introduction
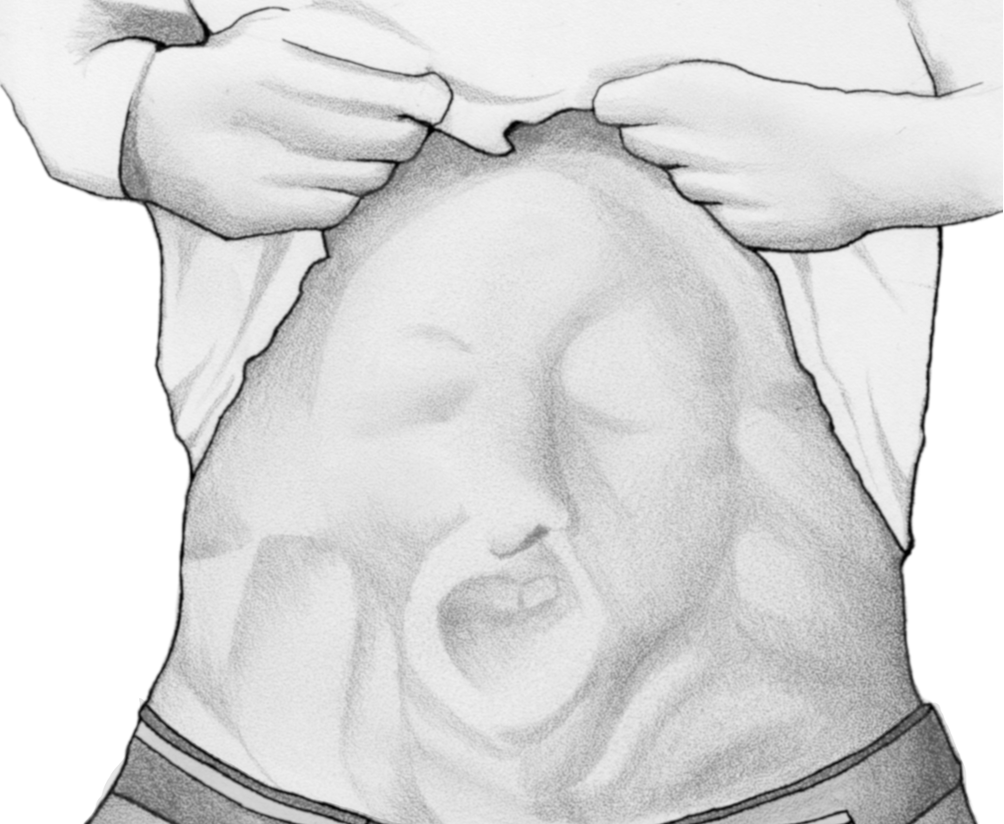
‘It was around 2001. I got a Staphylococcus infection in my stomach and then, from having a stomach of steel, it became a cotton wool stomach’. Michael 1 laughs at his own description and continues in a serious tone of voice: ‘Previously, I could eat everything – anything. No matter what and how spicy it was. […] And then, suddenly, I cannot manage anything. I have to think about everything I eat, how I eat, when I eat, whether I have the same food several days in a row’. Michael explains that he can often sense when he has eaten something wrong, such as carrots: ‘I can simply follow them as they pass through the intestines until they come out […] You can hear it. It’s not only because of the carrots, but I have so much gas in my stomach. All of a sudden, I may look like a Japanese fighting fish’. Michael laughs and adds: ‘I’m big enough already, but I can become completely like ‘fwoosh’. He makes a sound and waves his arms to show how his stomach inflates, and then he adds: ‘Other people are also not in doubt that something is not how it should be’.
Michael is a man in his 40s who suffers from multiple health problems, including gut trouble, diabetes, back pain, allergies, and a knee injury which has forced him to stop working. He is one of the people I have come to know during my ethnographic fieldwork at two outpatient gastroenterology clinics and among people diagnosed with irritable bowel syndrome (IBS) in Denmark. One afternoon in October 2016, Michael and I are sitting at the dinner table in his small farmhouse in rural Jutland. He recalls that he first consulted his doctor in 2004, when his stomach pain, bloating, and shifts between diarrhoea and constipation ‘had simply become too annoying [ træls ]’. In a later interview, he elaborates: ‘It was impossible to endure, so there was no other option than to get examined. […] If something could be done about it so that I could get my life back to some extent, it had to be done’.
Michael is not the only person in this study who describes his gut ailment as annoying or irritating. It may have been a slip of the tongue when another interlocutor told me that he thought that he was suffering from ‘ irritating bowel syndrome’ [ irriterende tyktarm ]. In this Research Article, I explore how afflicted individuals attend to, experience, and respond to gut trouble diagnosed as irritable bowel syndrome (IBS) in a Danish context in which citizens interact with the welfare state in multiple ways throughout their lives. Specifically, I explore the relation between IBS, attention, and irritation. As described by Donna J. Haraway, ‘trouble’ may refer to practices of disturbing, stirring up, or making cloudy (2016, 1). Following Haraway’s suggestion to ‘stay with the trouble’ (2016), to become capable of responding to it, that is, to pay attention to the trouble rather than trying to settle it or look for quick fixes, I stay with and wonder about what I term ‘gut trouble’ 2 : the bodily sensations associated with the gut which disturb, trouble, or complicate people’s lives.
Taking a cue from my interlocutors, I use irritation as a sensitising concept, one with a biosocial quality: on the one hand, irritation refers to a physical condition in which a part of the body is sensitive to a stimulus or agent and reacts to it with, for example, soreness or redness. This is in line with Michael’s description of the sensitive ‘cotton wool stomach’, which reacts to carrots and other food items with noise, smell, distension, and pain or discomfort. Although IBS is most commonly classified as a ‘medically unexplained’ or ‘functional’ disorder (because available biotechnologies cannot detect signs of organic disease), some biomedical researchers suggest that inflammation may figure as one of many aetiological factors (Enck et al. 2016; Fink and Rosendal 2015). On the other hand, I use irritation to describe an emotional, embodied response that can best be expressed through the Danish word ‘ træls 3 ’. Especially in Jutland, where my fieldwork took place, the word ‘ træls ’ is often used instead of ‘ irriterende ’ (which can be translated into ‘irritating’ or ‘annoying’) to articulate that something is bothersome, strenuous, unwanted, or uncomfortable. For people like Michael, it is associated with, and sometimes a collective term for different emotions such as embarrassment, frustration, and fear. Previous studies have described how people diagnosed with IBS feel burdened by recurring and embarrassing gut sensations, and become frustrated when the healthcare system can offer neither definite medical explanations nor cures. Some people find that their complaints are not taken seriously (Håkanson 2010; Rønnevig, Vandvik, and Bergbom 2009, 2014; White 2022, 2021). For health professionals, IBS is also an ‘irritating’ disorder. This is because IBS patients often seek healthcare repeatedly, and their symptoms, which may resemble those of life-threatening diseases such as cancer (Enck et al. 2016), challenge traditional biomedical ways of classifying, explaining and treating disease (Dixon-Woods and Critchley 2000).
Biomedical researchers estimate that IBS affects 11–16% of the Danish population (Krogsgaard, Engsbro, and Bytzer 2013; Rasmussen 2015). Acknowledging that IBS is not only a health challenge in Denmark 4 and that it will remain an open question how culturally specific my findings are, I seek to highlight the socio-cultural embeddedness of gut trouble. Denmark has often been portrayed as an affluent welfare society which helps citizens when they run into problems. For example, the welfare state offers free (tax-funded) health services as well as social security benefits when people become ill or unemployed (Wiking 2014). Most people in Denmark place high levels of trust in welfare institutions such as the healthcare system (Frumer et al. 2021). More than providing services to accommodate needs, the welfare state enables citizens to ‘fare well’ through life (Langer and Højlund 2011). In this understanding, ‘welfare’ may refer to practices, ethical orientations, and expectations; ‘an interpretation of a way to fare well, a means of order in and ordering of life’ (Gulløv 2011, 29). In a Danish welfare context, citizens are expected to lead active, independent lives with family and friends, to be productive parts of the labour market, and to care for themselves to the extent possible (Bruun, Krøijer, and Rytter 2015; Merrild and Andersen 2019; Mik-Meyer and Villadsen 2013). Notions of health are linked to individual responsibilities of leading a healthy ‘lifestyle’ and paying attention to possible signs of life-threatening disease while not overusing the healthcare system (Kristensen, Lim, and Askegaard 2016; Offersen et al. 2018, 2016). How may a focus on irritating guts offer a window onto expectations, moral strivings (Mattingly 2014), and notions of ‘faring well’ (Langer and Højlund 2011) among people in Denmark?
As argued by Sjaak van der Geest, gut-related matters constitute particularly suitable cases for studying the ‘complex intertwinement of what we call “nature” and “culture”’ (2016, 77). Based on her study of defecatory practices, toilet training, and excremental language in Britain, Rachel Lea (2001) argues that defecation is a cultural performance associated with intimacy, privacy, and values of feeling in control. However, she notes that this is different in, for example, Ghana, where van der Geest (1998) described how excretion is often not a solitary act, and many people consume laxatives to avoid constipation, which itself is associated with dirt and poor health. Other studies have shown how excretion and the management of excrement have been made part of colonial projects of disciplining (Anderson 2006) and executions of power in contexts of war (Al-Mohammad 2007). As phrased by Eileen Moyer and Vinh-Kim Nguyen, ‘the gut is where violence, irritation, and absorption occur; it is where substance can be transformed into physical endurance – or can sap vigour’ (2015, iii). Thomas Cousins also invites us to think with the gut as an entity which emphasises the absorption of nature into culture and vice versa, and which shows that we can ‘neither assume that processes of health and disease are purely social constructs, nor can we take nature to have an autonomy from the social’ (2015, 14). In this article, I pursue these anthropological explorations of the gut, and in particular Cousins’ call to take the material body seriously, acknowledging that defecation is both a biological necessity and a social and culturally shaped practice. Rather than entering discussions about power, disciplining, or semiotics, however, I contribute to phenomenological discussions on attention.
I understand ‘attention’ as the embodied, socially and culturally mediated foregrounding of certain aspects of the world. Attention is selective, that is, not all aspects of our being-in-the-world are pulled forward to constitute our experience (Pedersen, Albris, and Seaver 2021; Throop and Duranti 2015; Throop 2010; Csordas 1993). Usually, the gut withdraws from one’s direct perception and control. As part of the viscera, it is characterised by what Drew Leder terms ‘depth disappearance’ (1990, 53). However, for people like Michael, the gut does not hide in the visceral depths. Contrary to Michael’s expectation that his gut should recede in everyday life, it flares like a Japanese fighting fish, continuously grabbing his attention when it inflates, hurts, or makes loud noises. Along these lines, I draw on Leder’s analysis of ‘dys-appearance’ (1990) and Jason Throop and Alessandro Duranti’s conceptualisation of ‘attentional pulls’ (2015) to analyse how people like Michael experience gut sensations as irritating in a Danish welfare context. I highlight how practices and expectations of ‘faring well’ (Langer and Højlund 2011) may contribute to moments of ‘dys-appearance’ (Leder 1990), and how irritation can ‘pull’ attention in an affective and biological sense, meaning that not only aspects of our surrounding world, but also our physical bodies as situated in this world, can exercise such ‘attentional pulls’ (Throop and Duranti 2015). Furthermore, I emphasise an agentive form of attention at play when afflicted individuals consciously experiment with paying attention to gut sensations to try to alleviate their gut trouble. Overall, I suggest that using irritation as a heuristic concept may enable a focus on that which does not quite fit, empirically and analytically. It may also help remind us of general problems with categorisation and causality, as irritation is situated ‘in between’ the ‘biological’ and the ‘social’, ‘mind’ and ‘body’.
Attention, irritation, and gut sensations
What biomedicine terms IBS was once believed to be ‘a psychiatric disorder in which patients paid greater attention to bowel complaints’ (Drossman 1988, 122). Although this view has changed over time, it has recently been proposed that certain gut-brain interactions make IBS patients experience signals from the gastrointestinal tract more intensely than other people (Enck et al. 2016). This article explores relations between IBS and attention from an anthropological perspective, approaching attention as an embodied, socially and culturally mediated ‘discriminating faculty in the organization of experience’ (Throop 2010, 9), but also as a ‘form of action’ (Pedersen, Albris, and Seaver 2021, 318).
From a phenomenological perspective, attention is grounded in bodily ways of being-in-the-world. As we move through the world, we attend to certain aspects of it, whereas other aspects fade into the background (Desjarlais and Throop 2011). Drawing on this understanding, Throop and Duranti (2015) propose five kinds of ‘attentional pulls’, of which I will highlight two for the purposes of the forthcoming analysis: the ‘breakdown’ and the ‘breakthrough’. When something is not working as expected or breaks down, our attention is ‘pulled’ towards it, and we seek to ‘repair’ it. Likewise, our attention is pulled towards something which we experience as conspicuous. For example, a loud noise which shocks us or a sudden pain may constitute ‘breakthroughs’ which we cannot ignore (2015, 1061–62). In particular, the ‘breakdown’ echoes Leder’s concept of ‘dys-appearance’ (1990), through which he describes how we become increasingly attentive to our bodies when they do not work as expected, as for example, when we feel pain. According to Leder, the viscera most often become expressive in relation to dysfunction. However, people can train themselves to bring otherwise unnoticed gut sensations into experience (1990, 38–44), whereby their bodies become sentient subjects, but also the objects to which they attend. This is in line with Csordas’ concept of ‘somatic modes of attention’ (1993) which describes that we pay attention to and with our bodies, but also emphasises that this happens in ‘culturally elaborated ways’ in milieus shared with the bodies of others.
In this article, I suggest that ‘dys-appearance’ and ‘attentional pulls’ unfold in relation to particular bodies in particular contexts, in line with other anthropologists who have described how bodily sensations are experienced, articulated, interpreted and responded to in embodied ways which are socially and culturally embedded (e.g., Throop 2010; Geurts 2002; Andersen, Nichter, and Risør 2017; Nichter 2008; Hay 2008; Hinton, Howes, and Kirmayer 2008; Offersen et al. 2016; Csordas 1993). For example, Throop has argued that the cultural patterning of attention affects whether bodily sensations are experienced as, for example, meaningful or intolerable (2010, 9–10). My analysis suggests that attention appears in two forms in relation to IBS. The first is attention as affection (cf. Throop & Duranti 2015, 1058–60), that is, when people cannot help being disturbed or distracted by their gut because gut sensations force themselves to the foreground of experience. The second is attention as a conscious act of care involved in experiments of paying attention to irritation to try to treat gut trouble. I thus argue that attention is not always the opposite of distraction, that it may involve agency on the part of afflicted individuals, and that irritation (as a physical condition and emotional response) has the potential to ‘pull’ attention towards the body.
Researching gut trouble in a Danish context of welfare
This article draws on 12 months of ethnographic fieldwork conducted between 2016 and 2020. The fieldwork began at two outpatient gastroenterology clinics where I participated in and observed daily routines, including consultations about different kinds of gut trouble, and interviews with key doctors, nurses, and dieticians. In Denmark, citizens are registered with a general practitioner (GP) who can refer them to specialised care, often at public hospitals. At the two public hospitals that participated in this study, IBS was a prevalent diagnosis. Yet the disorder was often associated with irritation, which was expressed in different ways. Some health professionals complained that IBS patients were often on their guard, presumably expecting yet another consultation in which they would not be taken seriously or helped, and they often demanded further examination and treatment. Many doctors felt dissatisfied when being unable to offer further treatment options or guarantee that treatments would work. Some health professionals were annoyed that IBS patients were even admitted to the clinics, which were busy and lacked (specialist) doctors. They argued that IBS was not life-threatening and rarely required specialised diagnostic interventions or medical treatment.
Through the clinics, I recruited 18 interlocutors. During the consultations I attended, they were diagnosed with IBS or informed that IBS seemed to be the most likely diagnosis for their condition. Most of these people had not been to the gastroenterology clinic before, but they had been in contact with other parts of the healthcare system several times. I entered their lives at a time when their gut trouble constituted such a big problem that they had been referred to a hospital, and they had expectations and hopes that specialists might finally diagnose and treat their gut trouble. Most people were offered one or a few consultations at the hospital. Some were offered medical treatments and consultations with a dietician, while others were offered advice on exercising, eating habits and fibre supplements.
The interlocutors were 11 women and 7 men, aged 21–61. One man withdrew from the study after one interview, but the rest of the interlocutors were interviewed at least twice. The first semi-structured interview, which was conducted shortly after our meeting at the clinic, concerned their healthcare seeking practices, their everyday experiences of their gut, and understandings of the gut trouble they were undergoing. The second interview was about life events and the everyday management of gut trouble. In addition to these interviews, I stayed in contact with interlocutors through emails, text messages, phone calls, and physical meetings. I continuously obtained informed consent from all interlocutors, and our interactions were guided by their needs and wishes. This meant that I interviewed some people more than twice, often in combination with home visits. Others invited me to participate in additional clinical appointments or to spend time and eat with them and their families. Including the two interviews, I met with the interlocutors up to five times during a period of four years. This time frame allowed me to explore how gut trouble fluctuated and was interwoven with their lives. Many were troubled for years, but some gradually felt better or accepted living with gut trouble. The interlocutors belonged to the middle or lower social classes. No matter if they were students, unemployed, or had time-consuming jobs, they had plans and dreams and expressed that they had enough to do in their lives and gut trouble restricted them.
In this article, I focus on four interlocutors whom I call Michael, Sandra, Emma, and Victoria. They share a frustration about gut trouble, which they find to be embarrassing, irritating, and difficult to manage. Their experiences and ways of acting on gut trouble exemplify what I also saw among other interlocutors.
The gut calls for attention: Irritation and ‘faring well’ through life
‘It feels like your gut is burning. You know, a really irritating, smarting pain. And the stomach, when it distends, then it feels like it’s empty, but I can sense my intestines in there. I mean, you can almost imagine how they lie in there, and then it feels like it’s burning inside them, and it’s terribly painful’. Here, Sandra describes her stomach pain as a kind of irritation or inflammation. In Leder’s words, pain effects a spatiotemporal constriction and an intentional disruption (1990, 73–76). Sandra’s stomach pain pulls her to the here and now, and her attention is directed towards the gut and away from her everyday activities, which are as a result disrupted. The pain represents a ‘breakthrough’ which she cannot ignore, a conspicuous experience which has suddenly afflicted her (Throop and Duranti 2015, 1062). No longer working as expected, her gut has ‘dys-appeared’ (Leder 1990, 84). Sandra’s gut sensations affect her as a call. They ‘pull’ her attention, not as a ‘conscious turning toward an object’ (Schutz 1970 in Csordas 1993, 138), but in the sense that they impose themselves on her and distract her (cf. Waldenfels 2011, cited in Throop and Duranti 2015, 1058). Her stomach distends, and the insides of her gut are brought to an experiential foreground. Throop and Duranti describe how such dynamics of attention can be guided by ‘different types of acts, events, and human and non-human entities’ (2015, 1057). Rather than surrounding acts, events, or entities, Sandra’s attention seems to be directed by a call from within her own body. Irritation appears in the form of a distended, painful body, but also, as I will show in the following, in the form of an interpretation that this body acts unexpectedly and is annoying.
When I meet Sandra at a gastroenterology clinic in September 2016, she is 26 years old. She experiences stomach pain every day, but sometimes also nausea, hot flashes, diarrhoea, and bloating. Sandra is frustrated when the doctor tells her that her blood and stool tests do not indicate that she is suffering from anything other than IBS. After the consultation, she explains to me that her brother-in-law was also told that he had IBS until a colonoscopy revealed that he had Crohn’s disease. Sandra’s mother-in-law, a nurse, is quite sure that Sandra has an inflammation in her intestines. Although Sandra exercises regularly and tries different diets and fibre supplements, as recommended by the clinic’s nurse, nothing improves. She doubts the diagnosis of IBS, and it makes her nervous to think about what could be wrong. ‘They [the doctors] ought to be able to look for something, right? It’s not such a big area after all’. Sandra points to her stomach and explains that she would like a colonoscopy or a scan. ‘There is something irritable in there, for sure. Because I have that burning sensation. There is something weird in there’. In Leder’s terms, Sandra’s gut trouble exerts a telic demand which includes hermeneutical and pragmatic moments (1990, 77–79). Her gut becomes an object of an ongoing interpretive quest, and this quest is complicated by the fact that her bodily sensations are difficult to predict and their causes remain obscure. Her body also becomes a subject and object of actions directed at a pragmatic goal: to get rid of or be able to manage gut trouble, that is, to ‘repair’ what is perceived to be ‘broken’. In this way, the aims of understanding and acting on gut trouble are two sides of the same coin, and gut trouble is experienced as irritating because it is both (medically) unexplained and unmanageable.
As such, the analysis could end here, with a conclusion that guts become irritating when they ‘dys-appear’ (Leder 1990) and that they ‘pull’ people’s attention (Throop and Duranti 2015). However, a ‘dysfunction’ or ‘breakdown’ is experienced in relation to expectations and perceptions of ‘normality’. In her study in Britain, Lea argues that health is associated with self-control, which is in turn associated with notions of maturity. To be a respectable, ‘normal’ grown-up is to have learned to hold on and let go at appropriate times—whether that be with regards to excrement, speech, or emotions (2001, 196–203). Other studies remind us that it is not a universal tendency to attend to indigestion as an expression of a gut ‘dysfunction’ or disease. For example, the ethnographic studies by Mark Nichter (2008) and Stefan Ecks (2004) describe how people in India sometimes approach indigestion as a sign of humoral imbalances, lack of self-control, or problems of modernisation, and Nichter’s study in Sri Lanka (1988) suggests that diarrhoea is considered ‘normal’ rather than a sign of illness when it occurs during periods of life transition. How, then, may a Danish welfare context contribute to the experience of gut trouble as ‘irritating’ and something to seek healthcare for?
As part of the Danish welfare state, the healthcare system is expected to help citizens when they get into trouble and to support them in ‘faring well’ through life (Langer and Højlund 2011). Many people in Denmark consider it a matter of course to consult a doctor if they have health concerns (Offersen et al. 2016). As Michal Frumer’s fieldwork among people in cancer surveillance makes clear, people in Denmark place high levels of trust in biomedicine and biotechnologies (Frumer et al. 2021). My interlocutors’ relationship with the healthcare system is simultaneously characterised by trust and mistrust, dependence and independence. Sandra’s statement that doctors ‘ought to be able to look for something’ testifies to a relationship with doctors which, despite an undertone of frustration, involves trust and expectations. The same may be said of what she refers to as a ‘Danish mentality’: a sense that you sometimes have to be your own doctor, check up on things yourself, and insist on getting the right examinations and treatments. Inherent in this assumption is that if people are vigilant about their bodies and seek healthcare ‘appropriately’, the biomedical profession will be able to ‘fix’ their problems. In this context, sufferers may interpret the lack of a biomedical explanation as meaning there is no explanation at all, neither biomedical nor any other kind. Sandra’s suspicion that ‘there is something irritable in there’ indicates that she connects her embodied experiences to an imagined anatomical map. This may exemplify what Rikke Sand Andersen has termed ‘disease sensitisation’ (2017) in the sense that the contemporary societal desire to alleviate and prevent suffering has pushed people in Denmark to become increasingly attentive to bodily sensations as possible signs of life-threatening disease. This societal desire relies on expectations that individual citizens are able to distinguish between being ‘sick’ and being ‘fine’ (Hay 2008) and seek healthcare at the ‘right’ time, neither being ‘too late’ for treatment, nor being ‘hypochondriacs’ who misuse the tax-funded common good (Offersen, Vedsted, and Andersen 2017). Drawing on ethnographic fieldwork exploring healthcare seeking practices in the Danish middle class, Sara Offersen and colleagues have referred to this as a ‘moral sensescape’ (ibid.). Navigating this ‘moral sensescape’ creates particular challenges for people who struggle with gut sensations which, I argue, may both constitute possible signs of a life-threatening disease and form part of everyday embodied life. As indicated in Sandra’s story, opinions and stories of family members and friends may also affect evaluations of bodily sensations and healthcare seeking practices.
While worries about severe diagnoses play into Sandra’s decision to seek healthcare, she emphasises that her main problem is that she has ‘an extremely irritating stomach’ which stands in the way of her life. ‘It annoys me when it hinders my life. Then I notice it’, she says. Sandra’s story exemplifies how irritation as an embodied response can offer a window onto practices and expectations of ‘faring well’ through life (Langer and Højlund 2011), including moral strivings towards a ‘good’ life (Mattingly 2014).
In Sandra’s view, it is particularly irritating to have a troublesome gut when you are young: ‘It’s irritating to have to worry about such things. I mean, also at my age, right? Geez, if I had been over 50 and I had 20 kids, then I wouldn’t have cared, I think. However, I’m 26 years old and I feel like my life has just begun’. The afflicted individuals in this study are young and middle-aged people who imagine that much of their lives lie ahead of them. Supported by the welfare state, people in Denmark are, to a large extent, able to—and expect themselves to be able to—shape their own lives. As articulated in Tine Tjørnhøj-Thomsen’s ethnographic study among involuntarily childless people in Denmark (1999), many people imagine that they will get an education and a job, settle in a house, and then have children, in line with the Danish saying ‘ villa, Volvo og vovse’ (villa, car and dog), which epitomises ideas about an ‘ordinary’ Danish middleclass family life. When I meet her, Sandra is living with her boyfriend in an apartment in a provincial town. She remarks that she is happy that she has been in a committed relationship for eight years so that she does not have to go out to party and impress boys. ‘I just know that I can’t go out in some tight-fitting dress, because when I have eaten, my stomach is just big’. Sometimes, her stomach becomes so distended that she thinks it looks as if she is five months pregnant. She has always imagined herself as a young mother, and she has dreamt of having a baby for a few years. However, it currently seems like an overwhelming thought. If her stomach is already troublesome, how should it be able to manage a pregnancy?
Sandra describes herself as a person who loves to spend time with her family and friends. However, her gut trouble sometimes gets in the way of the social life she imagines herself to be living. In Denmark, eating and drinking together is often associated with hygge , a celebrated Danish idea best translated as a cosy atmosphere or style of social interaction (Linnet 2011). Eating together is often more important than what is consumed (Jenkins 1999) ; yet Sandra’s experience of a Christmas dinner exemplifies how the food consumed may become most important, and how, when this happens, the gut becomes an irritating presence which disturbs social conventions of a hyggelig meal. Christmas Eve in Denmark is usually associated with a shared home-cooked meal including duck, stuffed turkey or roast pork with crackling, boiled potatoes, caramelised potatoes, brown sauce (gravy), pickled red cabbage, and risalamande (a sweet rice pudding with almonds) for dessert. Sandra explains that eating the food served on Christmas Eve means that she has to go to the toilet during dinner: ‘I can’t sit down and eat together with the others. That’s irritating […] If I get that type of food which is too greasy, then the gut opts out completely’. For Sandra, the Christmas menu constitutes a prominent example of what she cannot eat, yet she has also experienced gut trouble during other social gatherings and when eating at home with her boyfriend.
Sandra works as a manager in a beauty store. She explains that she tries to ignore it when her stomach suddenly hurts and she is in the middle of a task at work:
I can’t just say to my customer: ‘You know what, my stomach hurts, so I will have to leave’. Because it happens every day. One time, when I was in the store around Christmas, I felt really bad, and I had actually called in sick, but it’s so busy in the Christmas period, right? So I went to work, and there was a couple who wanted to have their gifts wrapped. And right when I began wrapping the first gift, I could just sense that … Okay, this hurts very much. And it hurt so much when I tried to ignore it that I was going to vomit. So I had to tell them: ‘You know what, I have to go and answer the phone now, I can hear it ringing’. And of course, it didn’t ring, but I simply had to go out and vomit.
In this situation, Sandra’s stomach pain and urge to vomit constitute a ‘breakdown’ and a ‘breakthrough’ (Throop and Duranti 2015) which she cannot ignore. The imminent need to vomit represents an unexpected happening which she seeks to ‘repair’ in order to comply with the norms of the social situation in the shop. She makes an effort to avoid awkwardness and embarrassment in the social interaction with her customers and to continue her working day as a ‘good’ employee: she comes to her colleagues’ rescue when it is busy, even though she feels sick; she conscientiously provides customer service despite stomach pain, and when she has to vomit, she politely excuses herself by referring to her obligation to answer the phone. Sandra’s embodied response (struggling to ignore impulses of vomit) may indicate that gut trouble is tabooed, but it also follows ‘a culturally valued sense of agency—of being productive, working and busy and being heroically able to overcome illness’ (Offersen, Vedsted, and Andersen 2017, 9). To Sandra, ‘the everyday’ with its mundane routines cannot be taken for granted. Rather, it may be thought of as ‘a fragile achievement, a hard-won moment of mundaneness’ (Mattingly 2014, 79). During moments when this struggle to achieve an ‘ordinary’ everyday life becomes especially challenging, the gut emerges as an irritating companion, or what I have described elsewhere as a ‘frenemy’ (Laursen, Meinert, and Grøn 2022), that calls for attention.
Experimenting to alleviate gut trouble: Attention as a conscious act
So far, I have analysed IBS as a problem of unexpected, distracting, and unwanted bodily sensations which pull people’s attention. In the following, I describe how attention may not only be understood as an aspect of experience; something which can be mediated, distributed or organised (Throop and Duranti 2015; Throop 2010). Attention may also involve agency. Below, I explore how afflicted individuals are impelled to experiment with paying attention to the gut, emphasising that attention as a ‘form of action’ (Pedersen, Albris, and Seaver 2021, 318) may help people to manage IBS. This, I will argue, comes close to the examples that Csordas (1993) provides of ‘somatic modes of attention’, e.g., when people who practise athletics or meditation consciously turn towards their bodies as subjects and objects of attention.
For many people suffering from gut trouble, the realisation that biomedical care cannot cure their trouble causes frustration and prompts them to scan their bodies to decipher signals of how their everyday habits of, for example, eating, drinking, and exercising affect their guts. Some are also encouraged by health professionals to pay attention to what makes them feel better. Emma, a 31-year-old woman who has suffered from stomach cramps since the age of 16 and was diagnosed with IBS in 2017, explains that disappointing experiences with the healthcare system in relation to her gut trouble have pushed her to take matters into her own hands: ‘I thought that I should be able to do something myself. Of course, it’s difficult for them [the doctors] to say something when everyone is so different. What is it actually that triggers it?’ In a Danish welfare context, the relationship between state (including the healthcare system) and citizens is characterised by trust and collectivist ideals, but also by expectations of individualism in the form of self-dependence or self-management (Bruun, Krøijer, and Rytter 2015; Gulløv 2011). Like Sandra, Emma embodies an ideal of being a productive, busy citizen who lives an active life and takes responsibility for her own health (cf. Offersen, Vedsted, and Andersen 2017). She works as a self-employed consultant specialising in weight loss and dietary supplements, and she describes herself as a strong-willed woman who keeps several balls in the air: she participates in four-wheel drive races, spends much time with her friends and in the gym, and dreams of starting a climate-friendly fitness centre in the small provincial town in which she lives with her seven-year-old daughter. She also avidly reads books about the gut to learn more about her condition, now that she has been told about IBS at the gastroenterology clinic. She hopes to alleviate her gut trouble by acquiring biomedical knowledge about the associations between food and the gut microbiome, and by attending to her own gut. Emma is not quite sure what the health professionals mean by IBS, but she understands it as a bodily warning signal that she is living or eating in inappropriate ways. Acknowledging that her body is not like a car, she uses a car metaphor to talk about her process of experimenting with food items and noting down her bodily sensations:
A car needs oil and gas and water and air and other stuff to function. If it doesn’t have any of that, or if it lacks oil or something else, then a red light begins to flash. Perhaps the body works in the same way. I mean, we need carbohydrates, fat, proteins, and minerals and all those things. […] I think it was a similar process when I had to begin figuring out what makes my gut feel better. Should I fill up with some other proteins, should I reduce my intake of carbohydrates, or should I add vitamins? I think this has been my way of adjusting … Of making my own manual for my body.
Admitting that it is sometimes difficult to make a ‘manual’ for one’s own body, Emma stresses the importance of sensing oneself 5 , since no one manual works for all guts. Her way of approaching her gut resonates with Michael D’Arcy’s description of patient Paul, who, during D’Arcy’s ethnographic fieldwork at a psychiatric inpatient unit in Dublin, becomes an active experimenter who reads books on psychoanalysis and whose embodied experience comes to serve as ‘both a measure and, in a sense, laboratory for exploring the effects of antipsychotics’ (2019, 104). More than swallowing his medications, Paul chews and gargles to taste them, and measures their effects as they pass his gums, tongue, and enter his digestive system. In this way, he becomes a kind of scientist who collects data through attending with and to his own body.
As noted by Cheryl Mattingly, the words ‘experience’ and ‘experiment’ are etymologically related (2014, 16), implying that experience is experimental, but perhaps also, as I will stress here, that experiments are practices which draw on experiences (of irritation, for example). Through the trope of the ‘moral laboratory’, Mattingly highlights the experimental nature of experience, showing how African Americans in Los Angeles become ‘researchers or experimenters of their own lives’ in the face of serious illnesses and disabilities (ibid.). Like Mattingly’s interlocutors, my interlocutors are reflective, agentive individuals rather than passive patients to whom things happen. In one sense, this article describes moral experiments in ‘how life might or should be lived’ (idem, 15). For afflicted individuals, gut trouble constitutes an obstacle to ‘faring well’ (Langer and Højlund 2011), but it also sets them on an experimental path towards best possible everyday lives and futures. In another sense, this article describes problem-oriented bodily experiments, highlighting the experiential nature of experiment. When people experiment with food to alleviate gut trouble, their gut sensations are ‘pulled’ to an experiential foreground and come to constitute ‘data’ which they need to pay attention to in order to figure out what works and what not. Similar to the experiments that Mattingly describes (2014), these experiments take place in and are inseparable from the messy, changeable, social circumstances of everyday life. As I have argued elsewhere (Laursen, Meinert, and Grøn 2022), experiences of gut trouble are often characterised by unpredictability: gut trouble may fluctuate in erratic ways, and similar food items do not always induce similar gut sensations. Thus, afflicted individuals are left to try out explanations and treatments in a subjunctive mood (Whyte 2005). They never know for sure what will work, yet when something does work, it becomes a ‘falsifiable truth’ about their guts, and the practical solution constitutes a (provisional) answer to their problem.
I argue that IBS can be understood as a diagnosis which fosters a ‘climate of experimentation’ (Nichter and Thompson 2006) in which afflicted individuals begin to pay closer attention to bodily changes than before, interpret these changes, and prioritise embodied experience over, for example, dietary guidelines. When Victoria, a woman in her early 40s, was diagnosed with IBS in April 2017, she was disappointed because she felt that the diagnosis placed the responsibility for treatment on her: ‘If it had been celiac disease, for example, then I would have known that I should avoid gluten […] However, this [IBS diagnosis] is really one where … Well, what are your thoughts about it? And then you will have to begin figuring out what you think’. In this sense, Victoria has turned the frustration about the IBS diagnosis into an agentive moment in which her gut becomes the subject and object of experiments. Victoria lives with her husband and her young daughter in a middle-class neighbourhood in a provincial town. As a disability pensioner, she spends much time at home, and her new role as a mother is an important part of her identity. In her view, everyone could learn from going back to listening to their guts, like her daughter: ‘I think that she’s in contact with that spontaneous feeling, that she senses what is actually good for her’. Victoria explains that she has realised the importance of relying on individual, embodied knowledge instead of general pieces of health advice:
I try to listen to myself, I mean, there are so many pieces of health advice and so many pieces of advice in general which state that you should do this and that, and then everything will be great, right? And that’s… We’re just different, people are just different, and I’ve discovered that what makes me feel good is not necessarily what’s recommended. So I try to listen to myself, […] my own gut feeling, and when I don’t do that, I feel worse, and when I do that, I feel better.
For example, Victoria has discovered that she should not eat too much rye bread, although this is considered a healthy Danish staple (Karrebæk 2012). With a smile, she notes that the extent to which rye bread is praised in Denmark is crazy: ‘When I eat that, my body just says: “No, not really …” It actually makes me feel pretty terrible, and then that’s just not something I should eat. It’s about daring to trust what the body tells you’. She explains that she is often not in doubt when she has eaten something wrong: ‘Then I get stomach pain or get extremely bloated or react with … I begin to feel tired and sluggish. It affects my energy and my stomach, and my digestion can break down. There may be many reactions. It may also be a sudden problem with stomach acid’.
During fieldwork, it seemed as if the voices of my interlocutors’ guts, when they were finally discerned, raised questions: When should they listen to the gut and when should they not? How should they pay attention to the gut without being perceived as overly sensitive? Emma’s account of an autumn holiday in a summer cottage with her friends and her daughter exemplifies how the voice of the gut may compete with other voices or needs:
One day, it was raining heavily, and we stayed inside and watched TV and made pancakes with ice cream and jam and all that other stuff you put on pancakes. I don’t mind eating pancakes at all, but as soon as the weather improved, I thought: Well, why not go for a walk to the beach? So I got everyone out on a trip to the beach. That was not only because of my stomach, but because I like the whole thing about that lifestyle: To go outside and be active. I feel that it gives my body energy, right? So I have no problem with eating unhealthy stuff, but I could also feel that… That was a day when we had had pasta one day and pizza the day after, and then we had pancakes the following afternoon, and I could just feel that my stomach was completely devastated [ fuldstændig smadret ]. I got constipated and it took four or five days before I could go to the toilet again.
Emma interprets her feeling of constipation as a sign that her stomach is ‘completely devastated’ because she has spent much time on the sofa, watching TV, and she has eaten pancakes, pizza and pasta. She values these activities and foods as part of socialising and having a hyggelig (cosy) time, yet they conflict with her wish of listening to her gut and leading what she perceives as a ‘healthy lifestyle’. She strives to eat ‘healthy’, ‘gut-friendly’ food, yet she emphasises that she also allows herself to eat ‘unhealthy’ food associated with hygge . Thus, the act of paying attention to the gut is an act of balance.
This is also the case for Michael, who was introduced in the beginning of this article, yet in a different way. His phone consultation with a doctor from the gastroenterology clinic raises the question of how to distinguish between paying ‘positive’ and ‘negative’ attention to the gut? For Michael, paying attention to the gut has helped him to identify certain foods which cause trouble. Yet, the doctor suggests that he pays too much attention to his gut and that he seems to have ‘negative thoughts’ about his gastrointestinal system and would benefit from taking antidepressants. Thus, while Michael and other people in Denmark are expected to be highly attentive to bodily changes to discover signs of life-threatening disease, they must not be overly worried (Offersen, Vedsted, and Andersen 2017). Furthermore, while they are encouraged to pay attention to their bodies to identify ‘triggers’ of gut trouble, they must not be (hyper)sensitive, following a logic that a heightened awareness of health, including eating habits, may cause increased bodily introspection and amplified sensations (Barsky 1988, 416).
Paying attention to irritation
Based on long-term ethnographic fieldwork at two Danish gastroenterology clinics and among 18 people afflicted by gut trouble diagnosed as IBS, I have highlighted a relationship between irritation and attention which I find to characterise everyday experiences of living with and trying to manage gut trouble. I have argued that afflicted individuals are impelled to pay attention to their guts, both because the irritation associated with their guts demands their attention, and because experimenting with consciously paying attention to gut irritation may help them to alleviate their gut trouble. The analysis has drawn inspiration from Leder’s concept of ‘dys-appearance’ (1990) as well as Throop and Duranti’s conceptualisation of ‘attentional pulls’ (2015). Both of them build on a phenomenological understanding of attention as a faculty which organises what is foregrounded and placed in the background in experience (Desjarlais and Throop 2011; Throop 2010). I have argued that my interlocutors seek healthcare because their guts do not work as expected. Their episodes of stomach pain, bloating, diarrhoea, and constipation represent ‘breakdowns’ and ‘breakthroughs’ (Throop and Duranti 2015) which inevitably ‘pull’ their attention, and their gut trouble exerts a telic demand (Leder 1990) to seek out explanations and treatments. Furthermore, I have described how an active or agentive form of attention may also play a role in relation to IBS: when medical care cannot cure gut trouble, afflicted individuals are impelled to experiment with remedies and food items while paying attention to gut sensations. IBS emerges as a diagnosis which fosters a ‘climate of experimentation’ (Nichter and Thompson 2006) in which people become experimenters of their own guts—and lives (Mattingly 2014). These experiments involve discerning the voice of the gut and balancing how and when to listen to it. What if paying attention to the gut is, on the one hand, expected and necessary to alleviate gut trouble, and, on the other hand, perceived as a sign of hypochondria or hypersensitivity? What if the gut’s voice contradicts general perceptions of a ‘healthy’ diet and lifestyle, or expectations of social life?
Through the analysis, I have argued that the Danish welfare context of my fieldwork manifests itself in and contributes to the particular ways that my interlocutors experience their guts as ‘irritating’ and the ways in which they respond to gut trouble. I have suggested that taking the experience of IBS seriously as an irritating disorder can offer a window onto the messy forms of attention and action which are at play when people try to cultivate ‘good lives’ or ‘lives worth living’ (Mattingly 2014) in a context of welfare. In this sense, an analytical focus on irritation as an embodied response directs attention towards the inseparability of (evaluations of) bodily sensations and the environments in which they are lived. IBS may not threaten life in the sense that people risk dying, but the irritation associated with the disorder testifies to the experience of a lived life which is threatened, or to ways of living in and organising society that do not accommodate gut trouble and other bodily troubles. Specifically, I have highlighted how practices and notions of ‘faring well’ (Langer and Højlund 2011) in Denmark include the concept of hygge that promotes an ideal of eating together. These practices also encompass the ideal that one should follow public health advice and the expectation that one should be able to shape and control one’s own life. Finally, they involve ideals of agency and productivity, and norms, expectations, and moral ambiguities in relation to healthcare seeking. Practices and expectations of ‘faring well’ are of course not only about national identity, but also dependent on social class, age, and gender. For example, concerns about (future) pregnancies and being able to wear tight dresses may foreground gut trouble as being ‘too irritating’ for some, but not for others, and although most people in Denmark are in the lucky position to have almost endless choices in their search for a remedy, not everyone has the same access to social and material resources.
IBS challenges imaginaries of a well-functioning Danish welfare machinery. People diagnosed with IBS have been found to make significant demands on healthcare resources and social benefits (Poulsen et al. 2018). IBS is difficult for health professionals to diagnose, explain and treat; it challenges the expectation that health professionals can heal and cure and does not fit into a traditional biomedical disease model. Its treatment often requires that patients and health professionals try out remedies together, and sometimes, it also demands the help of other actors such as family members, psychologists, and social workers. Sometimes, gut trouble disappears without any apparent rational explanation. It is not either biological or social, either mental or somatic. Or not always at least. It is a time-consuming disorder which puts pressure on a healthcare system which is already under pressure from cutbacks and a shortage of doctors (Andersen and Vedsted 2015). This apparent mismatch between IBS, welfare institutions, and ‘well-faring’ may prompt the question of whether the expectations in relation to healthcare, of both health professionals and patients, are too high. Is the irritation —the feeling that the gut is irritated and that this is ‘ træls ’—a sign that something in society could or should be different?
Finally, I suggest that paying attention to irritation may offer insights which go beyond the topic of IBS in Denmark. Irritation may be used as an analytical lens which directs attention towards the potential of that which causes trouble or does not fit in. It may hold the potential of irritating or disturbing other concepts and the ways we perceive reality. This is in line with Mattingly’s revival of Hannah Arendt’s idea of ‘defrosting concepts’ and her suggestion that empirical trouble may shake or disrupt understandings which have become ‘frozen’ and taken for granted (Mattingly 2019). My argument can also be seen as a continuation of a long tradition of troubling categories in medical anthropology (e.g., Rhodes 1996; Good 1993). In the example of IBS, we may ‘stay with the trouble’ (Haraway 2016) to continue to refine our thinking about categories such as the ‘biological’ and the ‘social’, the ‘mind’ and the ‘body’, which seem to continuously haunt us although the dichotomies have been challenged innumerable times (e.g., Leder 1990). Or to refine our thinking about concepts such as attention and dys-appearance (Leder 1990). In this analysis of gut trouble, I have suggested that attention is not always the opposite of distraction, and that irritation—as a physical condition and an emotional, embodied response—can ‘pull’ attention. Furthermore, I have distinguished between two kinds of attention: attention as a ‘call’ which imposes itself on afflicted individuals, also from within their own bodies, and attention as an act; a conscious ‘turning toward’, (cf. Csordas 1993). Furthermore, I have nuanced Leder’s analysis of dys-appearance (1990) by highlighting the need to contextualise what it means to say that bodies do not ‘work as expected’. In this sense, the article raises questions of an analytical kind: What may the presence of irritation in an analysis tell us? How may we refine concepts to better understand things that do not fit in?
Authorship statement
This article is authored by Camilla Brændstrup Laursen based on research planned and conducted by her.
Ethics statement
The data collection was approved by the Danish Data Protection Agency (journal no. 2015-57-0002) and Aarhus University (journal no. 2016-051-000001, sequential no. 560). The Central Denmark Region Committees on Health Research Ethics confirmed that no further ethical approval is required since the study is based on interviews and observation.
Acknowledgements
I thank my afflicted interlocutors and people at the two gastroenterology clinics for letting me into their everyday lives and routines, and for sharing their experiences and reflections with me. I also thank my PhD supervisors, Rikke Sand Andersen, Lotte Meinert, and Cheryl Mattingly for our discussions of the article’s analytical direction. I am grateful to the three anonymous reviewers and the MAT Editorial Collective who provided useful comments that especially helped me to strengthen my conceptualisation of irritation. This research project was made possible by funding from the Graduate School of Arts, Aarhus University, Denmark.
About the author
Camilla Brændstrup Laursen is a medical anthropologist and author of the PhD dissertation, ‘Gut Trouble: Irritation, Experimentation, and Welfare in Denmark’, written at the Department of Anthropology, Aarhus University, Denmark. Her research interests centre on bodily sensations, healthcare seeking practices, and everyday managements of medical uncertainties. In her new research project, ‘The Acute Healthcare System for Citizens’, located at the Emergency Medical Services, the Central Denmark Region, she will explore evaluations of bodily sensations and pathways through the Danish acute healthcare system.
Camilla Brændstrup LaursenReferences
Al-Mohammad, Hayder. 2007. ‘Ordure and Disorder: The Case of Basra and the Anthropology of Excrement’. Anthropology of the Middle East 2 (2): 1–23. https://doi.org/10.3167/ame.2007.020202 .
Anthropology of the Middle East https://doi.org/10.3167/ame.2007.020202Andersen, Rikke Sand. 2017. ‘Directing the Senses in the Contemporary Orientations to Cancer Disease Control: Debating Symptom Research’. Tidsskrift for Forskning i Sygdom og Samfund 14 (26): 145–71. https://doi.org/10.7146/tfss.v14i26.26282 .
Tidsskrift for Forskning i Sygdom og Samfund https://doi.org/10.7146/tfss.v14i26.26282Andersen, Rikke Sand, Mark Nichter, and Mette Bech Risør. 2017. ‘Introduction: Sensations, Symptoms and Healthcare Seeking’. Anthropology in Action 24 (1): 1–5. https://doi.org/10.3167/aia.2017.240101 .
Anthropology in Action https://doi.org/10.3167/aia.2017.240101Andersen, Rikke Sand, and Peter Vedsted. 2015. ‘Juggling Efficiency. An Ethnographic Study Exploring Healthcare Seeking Practices and Institutional Logics in Danish Primary Care Settings’. Social Science and Medicine 128: 239–45. https://doi.org/10.1016/j.socscimed.2015.01.037 .
Social Science and Medicine https://doi.org/10.1016/j.socscimed.2015.01.037Anderson, Warwick. 2006. Colonial Pathologies: American Tropical Medicine, Race, and Hygiene in the Philippines . Durham, NC: Duke University Press.
Colonial Pathologies: American Tropical Medicine, Race, and Hygiene in the PhilippinesBarsky, Arthur Joseph. 1988. ‘The Paradox of Health’. The New England Journal of Medicine 318 (7): 414–18. https://doi.org/10.1056/NEJM198802183180705 .
The New England Journal of Medicine https://doi.org/10.1056/NEJM198802183180705Bruun, Maja Hojer, Stine Krøijer, and Mikkel Rytter. 2015. ‘Indledende Perspektiver: Forandringsstaten Og Selvstændighedssamfundet’. Tidsskriftet Antropologi (72): 11–37. https://tidsskrift.dk/tidsskriftetantropologi/issue/view/3800 .
Tidsskriftet Antropologi https://tidsskrift.dk/tidsskriftetantropologi/issue/view/3800Cousins, Thomas. 2015. ‘A Mediating Capacity: Toward an Anthropology of the Gut’. Medicine Anthropology Theory 2 (2): 1–27. https://doi.org/10.17157/mat.2.2.175 .
Medicine Anthropology Theory https://doi.org/10.17157/mat.2.2.175Csordas, Thomas J. 1993. ‘Somatic Modes of Attention.’ Cultural Anthropology 8 (2): 135–56. https://doi.org/10.1525/can.1993.8.2.02a00010 .
Cultural Anthropology https://doi.org/10.1525/can.1993.8.2.02a00010D’Arcy, Michael. 2019. ‘“It Tastes Like Order”: Psychotic Evidence for Antipsychotic Efficacy and Medicated Subjectivity’. Ethos 47 (1): 89–107.
Ethoshttps://doi.org/10.1111/etho.12227 .
https://doi.org/10.1111/etho.12227Desjarlais, Robert, and C. Jason Throop. 2011. ‘Phenomenological Approaches in Anthropology’. Annual Review of Anthropology 40: 87–102.
Annual Review of Anthropologyhttps://doi.org/10.1146/annurev-anthro-092010-153345 .
https://doi.org/10.1146/annurev-anthro-092010-153345Dixon-Woods, Mary, and Sophie Critchley. 2000. ‘Medical and Lay Views of Irritable Bowel Syndrome’. Family Practice 17 (2): 108–13.
Family Practicehttps://doi.org/10.1093/fampra/17.2.108 .
https://doi.org/10.1093/fampra/17.2.108Drossman, Douglas A. 1988. ‘Irritable Bowel Syndrome: A Multifactorial Disorder’. Hospital Practice 23 (9): 119–33. https://doi.org/10.1080/21548331.1988.11703538 .
Hospital Practice https://doi.org/10.1080/21548331.1988.11703538Ecks, Stefan. 2004. ‘Bodily Sovereignty as Political Sovereignty: “Self‐Care” in Kolkata, India’. Anthropology and Medicine 11 (1): 75–89.
Anthropology and Medicinehttps://doi.org/10.1080/1364847042000204906 .
https://doi.org/10.1080/1364847042000204906Enck, Paul, Qasim Aziz, Giovanni Barbara, Adam D. Farmer, Shin Fukudo, Emeran A. Mayer, and Beate Niesler, et al. 2016. ‘Irritable Bowel Syndrome’. Nature Reviews: Disease Primers 2: 1–24. https://doi.org/10.1038/nrdp.2016.14 .
Nature Reviews: Disease Primers https://doi.org/10.1038/nrdp.2016.14Fink, Per, and Marianne Rosendal. 2015. Functional Disorders and Medically Unexplained Symptoms: Assessment and Treatment . Aarhus: Aarhus University Press.
Functional Disorders and Medically Unexplained Symptoms: Assessment and TreatmentFrumer, Michal, Rikke Sand Andersen, Peter Vedsted, and Sara Marie Hebsgaard Offersen. 2021. ‘“In the Meantime”: Ordinary Life in Continuous Medical Testing for Lung Cancer’. Medicine Anthropology Theory 8 (2): 1–26.
Medicine Anthropology Theoryhttps://doi.org/10.17157/mat.8.2.5085 .
https://doi.org/10.17157/mat.8.2.5085Geurts, Kathryn Linn. 2002. Culture and the Senses: Bodily Ways of Knowing in an African Community . Berkeley, CA: University of California Press.
Culture and the Senses: Bodily Ways of Knowing in an African CommunityGood, Byron J. 1993. Medicine, Rationality and Experience: An Anthropological Perspective . Cambridge: Cambridge University Press.
Medicine, Rationality and Experience: An Anthropological PerspectiveGulløv, Eva. 2011. ‘Welfare and Self Care: Institutionalized Visions for a Good Life in Danish Day-Care Centres’. Anthropology in Action 18 (3): 21–32. https://doi.org/10.3167/aia.2011.180303 .
Anthropology in Action https://doi.org/10.3167/aia.2011.180303Haraway, Donna. 2016. Staying with the Trouble: Making Kin in the Chthulucene . Durham, NC: Duke University Press.
Staying with the Trouble: Making Kin in the ChthuluceneHay, M. Cameron. 2008. ‘Reading Sensations: Understanding the Process of Distinguishing “Fine” from “Sick”’. Transcultural Psychiatry 45 (2): 198–229. https://doi.org/10.1177/1363461508089765 .
Transcultural Psychiatry https://doi.org/10.1177/1363461508089765Hinton, Devon E., David Howes, and Laurence J. Kirmayer. 2008. ‘Toward a Medical Anthropology of Sensations: Definitions and Research Agenda’. Transcultural Psychiatry 45 (2): 142–162. https://doi.org/10.1177/1363461508089763 .
Transcultural Psychiatry https://doi.org/10.1177/1363461508089763Håkanson, Cecilia. 2010. ‘Living with Irritable Bowel Syndrome: A Patient Perspective on Everyday Life, Health Care Encounters and Patient Education’. PhD dissertation, Karolinska institutet.
Håkanson, Cecilia. 2014. ‘Everyday Life, Healthcare, and Self-Care Management among People with Irritable Bowel Syndrome: An Integrative Review of Qualitative Research’. Gastroenterology Nursing 37 (3): 217–25.
Gastroenterology Nursinghttps://doi.org/10.1097/SGA.0000000000000048 .
https://doi.org/10.1097/SGA.0000000000000048Jenkins, Richard. 1999. ‘Fællesspisning Midt I Jylland: Når Det Drejer Sig Mere Om Spisning Og Drikning End Om Mad Og Drikke’. Tidsskriftet Antropologi 39: 37–52. https://tidsskrift.dk/tidsskriftetantropologi/issue/view/8325 .
Tidsskriftet Antropologi https://tidsskrift.dk/tidsskriftetantropologi/issue/view/8325Karrebæk, Martha Sif. 2012. ‘“What's in Your Lunch Box Today?”: Health, Respectability, and Ethnicity in the Primary Classroom’. Journal of Linguistic Anthropology 22 (1): 1–22. https://doi.org/10.1111/j.1548-1395.2012.01129.x .
Journal of Linguistic Anthropology https://doi.org/10.1111/j.1548-1395.2012.01129.xKristensen, Dorthe Brogård, Ming Lim, and Søren Askegaard. 2016. ‘Healthism in Denmark: State, Market, and the Search for a “Moral Compass”’. Health 20 (5): 485–504. https://doi.org/10.1177/1363459316638541 .
Health https://doi.org/10.1177/1363459316638541Krogsgaard, Laura Rindom, Anne Line Engsbro, and Peter Bytzer. 2013. ‘The Epidemiology of Irritable Bowel Syndrome in Denmark. A Population-Based Survey in Adults ≤50 Years of Age’. Scandinavian Journal of Gastroenterology 48 (5): 523–29. https://doi.org/10.3109/00365521.2013.775328 .
Scandinavian Journal of Gastroenterology https://doi.org/10.3109/00365521.2013.775328Langer, Susanne, and Susanne Højlund. 2011. ‘An Anthropology of Welfare: Journeying Towards the Good Life’. Anthropology in Action 18 (3): 1–9. https://doi.org/10.3167/aia.2011.180301 .
Anthropology in Action https://doi.org/10.3167/aia.2011.180301Laursen, Camilla Brændstrup, Lotte Meinert, and Lone Grøn. 2022. ‘Alien Guts? Exploring Lives of and with Irritable Bowels in Denmark’. Medical Anthropology Quarterly 36 (1): 139–54. https://doi.org/10.1111/maq.12669 .
Medical Anthropology Quarterly https://doi.org/10.1111/maq.12669Lea, Rachel V. 2001. ‘The Performance of Control and the Control of Performance: Towards a Social Anthropology of Defecation’. PhD dissertation, Department of Human Sciences, Brunel University.
Leder, Drew. 1990. The Absent Body . Chicago, IL: The University of Chicago Press.
The Absent BodyLinnet, Jeppe Trolle. 2011. ‘Money Can't Buy Me Hygge: Danish Middle-Class Consumption, Egalitarianism, and the Sanctity of Inner Space’. Social Analysis 55 (2): 21–44. https://doi.org/10.3167/sa.2011.550202 .
Social Analysis https://doi.org/10.3167/sa.2011.550202Mattingly, Cheryl. 2014. Moral Laboratories: Family Peril and the Struggle for a Good Life . Oakland, CA: University of California Press.
Moral Laboratories: Family Peril and the Struggle for a Good LifeMattingly, Cheryl. 2019. ‘Defrosting Concepts, Destabilizing Doxa: Critical Phenomenology and the Perplexing Particular’. Anthropological Theory 19 (4): 415–39. https://doi.org/10.1177/1463499619828568 .
Anthropological Theory https://doi.org/10.1177/1463499619828568Merrild, Camilla, and Rikke Sand Andersen. 2019. ‘Welfare Transformations and Expectations of Sameness. Living on the Margins in Denmark’. Nordic Journal of Social Research 10 (1): 66–84. https://doi.org/10.7577/njsr.2858 .
Nordic Journal of Social Research https://doi.org/10.7577/njsr.2858Mik-Meyer, Nanna, and Kaspar Villadsen. 2013. Power and Welfare: Understanding Citizens' Encounters with State Welfare . Abingdon, Oxon: Routledge, Taylor and Francis.
Power and Welfare: Understanding Citizens' Encounters with State WelfareMoyer, Eileen, and Vinh-Kim Nguyen. 2015. ‘Everyday Afflictions in Global Context’. Medicine Anthropology Theory 2 (2): i–iii. https://doi.org/10.17157/mat.2.2.521 .
Medicine Anthropology Theory https://doi.org/10.17157/mat.2.2.521Nichter, Mark. 1988. ‘From Aralu to Ors: Sinhalese Perceptions of Digestion, Diarrhea, and Dehydration’. Social Science & Medicine 27 (1): 39–52.
Social Science & Medicinehttps://doi.org/10.1016/0277-9536(88)90162-1 .
https://doi.org/10.1016/0277-9536(88)90162-1Nichter, Mark. 2008. ‘Coming to Our Senses: Appreciating the Sensorial in Medical Anthropology’. Transcultural Psychiatry 45 (2): 163–197.
Transcultural Psychiatryhttps://doi.org/10.1177/1363461508089764 .
https://doi.org/10.1177/1363461508089764Nichter, Mark, and Jennifer Jo Thompson. 2006. ‘For My Wellness, Not Just My Illness: North Americans’ Use of Dietary Supplements’. Culture, Medicine, and Psychiatry 30 (2): 175–222. https://doi.org/10.1007/s11013-006-9016-0 .
Culture, Medicine, and Psychiatry https://doi.org/10.1007/s11013-006-9016-0Offersen, Sara Marie Hebsgaard, Mette Bech Risør, Peter Vedsted, and Rikke Sand Andersen. 2016. ‘Am I Fine? Exploring Everyday Life Ambiguities and Potentialities of Embodied Sensations in a Danish Middle-Class Community’. Medicine Anthropology Theory 3 (3): 23–45. https://doi.org/10.17157/mat.3.3.392 .
Medicine Anthropology Theory https://doi.org/10.17157/mat.3.3.392Offersen, Sara Marie Hebsgaard, Mette Bech Risør, Peter Vedsted, and Rikke Sand Andersen. 2018. ‘Cancer-before-Cancer: Mythologies of Cancer in Everyday Life’. Medicine Anthropology Theory 5 (5): 30–52. https://doi.org/10.17157/mat.5.5.540 .
Medicine Anthropology Theory https://doi.org/10.17157/mat.5.5.540Offersen, Sara Marie Hebsgaard, Peter Vedsted, and Rikke Sand Andersen. 2017. ‘“The Good Citizen”: Balancing Moral Possibilities in Everyday Life between Sensation, Symptom and Healthcare Seeking’. Anthropology in Action 24 (1): 6–12. https://doi.org/10.3167/aia.2017.240102 .
Anthropology in Action https://doi.org/10.3167/aia.2017.240102Pedersen, Morten Axel, Kristoffer Albris, and Nick Seaver. 2021. ‘The Political Economy of Attention’. Annual Review of Anthropology 50. https://doi.org/10.1146/annurev-anthro-101819-110356 .
Annual Review of Anthropology https://doi.org/10.1146/annurev-anthro-101819-110356Poulsen, Chalotte H., Lene F. Eplov, Carsten Hjorthøj, Lene H. Hastrup, Marie Eliasen, Thomas M. Dantoft, Andreas Schröder, and Torben Jørgensen. 2018. ‘Irritable Bowel Symptoms, Use of Healthcare, Costs, Sickness and Disability Pension Benefits: A Long-Term Population-Based Study’. Scandinavian Journal of Public Health 47 (8): 1–9. https://doi.org/10.1177/1403494818776168 .
Scandinavian Journal of Public Health https://doi.org/10.1177/1403494818776168Rasmussen, Sanne. 2015. ‘Gastrointestinal Symptoms in the General Population: Prevalences, Overlap and Contact to General Practice’. PhD dissertation, Research Unit of General Practice, University of Southern Denmark.
Rhodes, Lorna A. 1996. ‘Studying Biomedicine as a Cultural System’. In Medical Anthropology: Contemporary Theory and Method , edited by Carolyn F. Sargent and Thomas M. Johnson, 165–182. Westport, CT: Praeger.
Medical Anthropology: Contemporary Theory and MethodRønnevig, Marit, Per Olav Vandvik, and Ingegerd Bergbom. 2009. ‘“Patients” Experiences of Living with Irritable Bowel Syndrome’. Journal of Advanced Nursing 65 (8): 1676–85. https://doi.org/10.1111/j.1365-2648.2009.05030.x .
Journal of Advanced Nursing https://doi.org/10.1111/j.1365-2648.2009.05030.xSperber, Ami D., Shrikant I. Bangdiwala, Douglas A. Drossman, Uday C. Ghoshal, Magnus Simren, Jan Tack, and William E. Whitehead, et al. 2021. ‘Worldwide Prevalence and Burden of Functional Gastrointestinal Disorders, Results of Rome Foundation Global Study’. Gastroenterology 160 (1): 99–114.
Gastroenterologyhttps://doi.org/10.1053/j.gastro.2020.04.014 .
https://doi.org/10.1053/j.gastro.2020.04.014Throop, C. Jason. 2010. Suffering and Sentiment: Exploring the Vicissitudes of Experience and Pain in Yap . Berkeley, CA: University of California Press.
Suffering and Sentiment: Exploring the Vicissitudes of Experience and Pain in YapThroop, C. Jason, and Alessandro Duranti. 2015. ‘Attention, Ritual Glitches, and Attentional Pull: The President and the Queen’. Phenomenology and the Cognitive Sciences 14 (4): 1055–82. https://doi.org/10.1007/s11097-014-9397-4 .
Phenomenology and the Cognitive Sciences https://doi.org/10.1007/s11097-014-9397-4Tjørnhøj-Thomsen, Tine. 1999. ‘Tilblivelseshistorier: Barnløshed, Slægtsskab Og Forplantningsteknologi I Danmark’. PhD dissertation, University of Copenhagen.
van der Geest, Sjaak. 1998. ‘Akan Shit: Getting Rid of Dirt in Ghana’. Anthropology Today 14 (3): 8–12. https://doi.org/10.2307/2783049 .
Anthropology Today https://doi.org/10.2307/2783049van der Geest, Sjaak. 2016. ‘Not Knowing About Defecation’ In On Knowing and Not Knowing in the Anthropology of Medicine , edited by R. Littlewood, 75–86. Walnut Creek, CA: Left Coast Press.
On Knowing and Not Knowing in the Anthropology of MedicineWhite, Lauren. 2021. ‘“I Have to Know Where I Can Go’: Mundane Mobilities and Everyday Public Toilet Access for People Living with Irritable Bowel Syndrome (Ibs)’. Social & Cultural Geography : 1–19.
Social & Cultural Geographyhttps://doi.org/10.1080/14649365.2021.1975165 .
https://doi.org/10.1080/14649365.2021.1975165White, Lauren. 2022. ‘Like Clockwork? (Re)Imagining Rhythms and Routines When Living with Irritable Bowel Syndrome (IBS)’. Sociology of Health & Illness : 1–17. https://doi.org/10.1111/1467-9566.13504 .
Sociology of Health & Illness https://doi.org/10.1111/1467-9566.13504Whyte, Susan Reynolds. 2005. ‘Uncertain Undertakings: Practicing Health Care in the Subjunctive Mood’. In Managing Uncertainty: Ethnographic Studies of Illness, Risk and the Struggle for Control , edited by V. Steffen, R. Jenkins and H. Jessen, 245–64. Copenhagen: Museum Tusculanum Press.
Managing Uncertainty: Ethnographic Studies of Illness, Risk and the Struggle for ControlWiking, Meik. 2014. The Happy Danes: Exploring the Reasons Behind the High Levels of Happiness in Denmark. The Happiness Research Institute (Copenhagen). https://www.happinessresearchinstitute.com/_files/ugd/928487_7f341890e9484a279416ffbc9dc95ff4.pdf .
The Happy Danes: Exploring the Reasons Behind the High Levels of Happiness in Denmark. https://www.happinessresearchinstitute.com/_files/ugd/928487_7f341890e9484a279416ffbc9dc95ff4.pdf-
All names are pseudonyms. Quotes have been translated from Danish by the author. ↩︎
-
This is also an emic term used by my interlocutors to talk about gut-related problems (in Danish: maveproblemer , træls mave or bøvlemave ). ↩︎
-
The Danish word ‘træls ’ is thought to derive from the word ‘ træl ’, which can be translated as ‘thrall’, that is, a slave during the Viking Age in Denmark. In this understanding, something that is ‘ træls ’ can be associated with a slave’s work. ↩︎
-
Prevalence rates are difficult to ascertain and compare across countries, e.g., because ways of diagnosing and measuring IBS differ (Sperber et al. 2021). ↩︎
-
Many people in this study talk about experimenting with ‘sensing oneself’ [ at mærke efter ] when trying to alleviate gut trouble. In Danish, ‘attention’ translates into opmærk somhed (my emphasis). ‘ At mærke’ means to feel, sense or perceive. In Danish, then, attention is closely connected with bodily acts of sensing or feeling. ↩︎
-
All names are pseudonyms. Quotes have been translated from Danish by the author. ↩︎
-
This is also an emic term used by my interlocutors to talk about gut-related problems (in Danish: maveproblemer , træls mave or bøvlemave ). ↩︎
-
The Danish word ‘træls ’ is thought to derive from the word ‘ træl ’, which can be translated as ‘thrall’, that is, a slave during the Viking Age in Denmark. In this understanding, something that is ‘ træls ’ can be associated with a slave’s work. ↩︎
-
Prevalence rates are difficult to ascertain and compare across countries, e.g., because ways of diagnosing and measuring IBS differ (Sperber et al. 2021). ↩︎
-
Many people in this study talk about experimenting with ‘sensing oneself’ [ at mærke efter ] when trying to alleviate gut trouble. In Danish, ‘attention’ translates into opmærk somhed (my emphasis). ‘ At mærke’ means to feel, sense or perceive. In Danish, then, attention is closely connected with bodily acts of sensing or feeling. ↩︎
All names are pseudonyms. Quotes have been translated from Danish by the author. ↩︎
All names are pseudonyms. Quotes have been translated from Danish by the author. ↩︎
↩︎This is also an emic term used by my interlocutors to talk about gut-related problems (in Danish: maveproblemer , træls mave or bøvlemave ). ↩︎
This is also an emic term used by my interlocutors to talk about gut-related problems (in Danish: maveproblemer , træls mave or bøvlemave ). ↩︎
maveproblemer træls mave bøvlemave ↩︎The Danish word ‘træls ’ is thought to derive from the word ‘ træl ’, which can be translated as ‘thrall’, that is, a slave during the Viking Age in Denmark. In this understanding, something that is ‘ træls ’ can be associated with a slave’s work. ↩︎
The Danish word ‘træls ’ is thought to derive from the word ‘ træl ’, which can be translated as ‘thrall’, that is, a slave during the Viking Age in Denmark. In this understanding, something that is ‘ træls ’ can be associated with a slave’s work. ↩︎
‘træls træl træls ↩︎Prevalence rates are difficult to ascertain and compare across countries, e.g., because ways of diagnosing and measuring IBS differ (Sperber et al. 2021). ↩︎
Prevalence rates are difficult to ascertain and compare across countries, e.g., because ways of diagnosing and measuring IBS differ (Sperber et al. 2021). ↩︎
↩︎Many people in this study talk about experimenting with ‘sensing oneself’ [ at mærke efter ] when trying to alleviate gut trouble. In Danish, ‘attention’ translates into opmærk somhed (my emphasis). ‘ At mærke’ means to feel, sense or perceive. In Danish, then, attention is closely connected with bodily acts of sensing or feeling. ↩︎
Many people in this study talk about experimenting with ‘sensing oneself’ [ at mærke efter ] when trying to alleviate gut trouble. In Danish, ‘attention’ translates into opmærk somhed (my emphasis). ‘ At mærke’ means to feel, sense or perceive. In Danish, then, attention is closely connected with bodily acts of sensing or feeling. ↩︎
at mærke efter opmærk somhed opmærk At mærke’ ↩︎