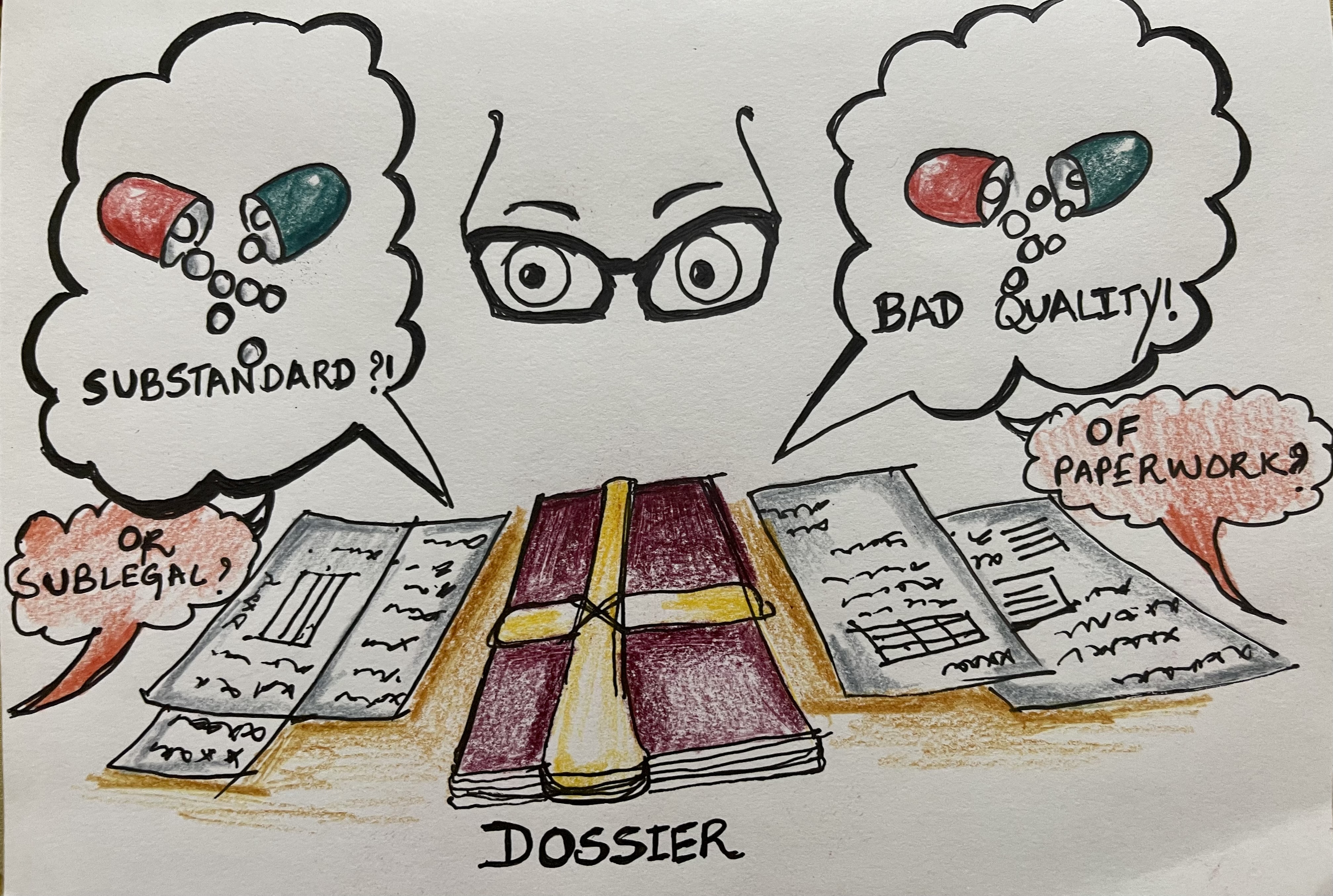
Sub-standard or Sub-legal?
Distribution, Pharma Dossiers, and Fake-talk in India
—
Received: 1 July 2022; Accepted: 27 April 2023; Published: 27 September 2023
India, Pharmaceutical industry, Security, Drug distribution, Regulation.
https://doi.org/10.17157/mat.10.3.7279
Abstract
In this article, I look at Indian pharma ‘dossiers’—the bundles of paperwork that testify to pharmaceutical quality and adherence to regulatory standards—and how they illustrate a wider and ongoing shift from a paradigm of drug safety to one of drug security. By examining how dossiers enact and enable claims of ‘quality’, I argue that it is in a drug’s paperwork—rather than its chemical composition—that quality or fake-ness is produced. Based on interviews with Indian traders and officials, and an examination of how their work has changed over time in accordance with the regulatory shift to drug security, I show that in many instances the paperwork has come to be more important than the pill itself. This analysis contests the dominant pharmaco-regulatory notion of fake-ness, which privileges chemical composition above all else. In this way, my analysis of the dossier shows that drug security is itself a powerful form of fake-talk, one that informs the entire market and the conditions of possibility of international commerce today.